Anesthesia: what is it?
Under the term anesthesia the medical layman can often not imagine much. In our following topic the concept of anesthesia will be brought a little closer.
Synonyms in a broader sense
- general anesthetic
- anesthesia
- anesthesia
- Pain therapy
- Emergency medicine
- Intensive care
English: anesthesia
Definition of terms
The specialist in anesthesiology is commonly referred to as anesthetist or Anesthetist designated. This suggests the anesthesiology would focus on that anesthesia (Anesthesia). However, anesthesia, i.e. anesthesia, is only a part of anesthesiology. It also includes: Intensive care medicine, pain therapy and Emergency medicine
education
The training for Specialist in "Anesthesia and Intensive Care Medicine" requires a completed medical degree and includes five years of advanced training in the areas of anesthesia, intensive care medicine, emergency medicine and pain therapy.
In the field of anesthesia there are various possibilities for professional activity.
In addition to the anesthetists, a so-called anesthetic assistant, in short, is required for every operation to run smoothly ATA. This profession can be learned through appropriate training, which usually lasts three years.
In order to be able to start an apprenticeship, you need at least secondary school leaving certificate. It can also be helpful to complete an internship in anesthesia before applying for training as an anesthesiologist assistant. You can get first impressions of the job description, exchange ideas with colleagues and then see whether you find this training suitable for yourself.
The training is school-based, which means that many units of theoretical instruction take place in an educational institution. In addition, practical lessons in a clinical facility are also guaranteed, where you can learn to apply the knowledge you have acquired and are supervised by ready-made anesthetic assistants.
In addition to numerous intermediate exams, there is a theoretical and a practical final exam at the end of the training.
The range of tasks of anesthesia assistants includes the care and support of patients before and / or after their surgical intervention. This included, among other things Putting on a pulse oximeter, Blood pressure cuff and EKG electrodeswhich provide the patient's parameters that must be observed during an operation.
In addition, their tasks include everything necessary for the upcoming surgery anesthesia- and Painkiller to select and prepare individually, as well as to provide for their replenishment.
Intubation is also helped by providing the material and handing it to the anesthetist. The sterilization of used instruments, such as a spatula for intubation, is also carried out by anesthesiologists.
In addition to the typical operating theater with the patient moving in and out of the operating room, in the recovery room, in the sterilization room, and in a practice with outpatient interventions, this job can be practiced.
Since a shift system determines the working hours in clinical operations, a high degree of flexibility is required from the trainees, both in terms of working hours and the cooperation with changing colleagues and surgical requirements.
History of anesthesia
In the first book of Moses (2:21) it says:
“The Lord God let fall a deep sleep on man, and he fell asleep. And he took one of his ribs and closed the place with meat ”.
Strictly speaking, the first application of anesthesia is already described in the Bible. The first anesthesia performed by a person did not come until almost 2000 years later: Ever since Humphrey Davy recognized the pain-relieving properties of laughing gas in 1800, medicine has tried to use these properties in practice. However, the first public demonstration of anesthesia using nitrous oxide in 1845 failed. Horace Wells, a dentist from Hartford, wanted to demonstrate the anesthetic effect of laughing gas at the time, but the patient screamed loudly when he tried to pull a tooth. It was William Thomas Green Morton, a dentist from Charlton, Massachusetts, who performed the first successful anesthetic a year later (October 16, 1846). The patient suffered from an ulcer on his neck which should be removed. Unlike Wells, Morton used ether for anesthesia. The ether ball specially made by him was used to enable the patient to inhale the volatile gas. This day went down in medical history as “Ether Day”.
Also read: Ethereal anesthesia
On its successful way to today's professional anesthesia, anesthesia often had to assert itself against adversaries. For a long time, the meaning of pain was not understood and it was believed that suppressing the pain would be detrimental to the patient's recovery. Pain is just part of life.
Most of the anesthetics in use today are not more than 20 years old - with the exception of the nitrous oxide itself.
General anesthesia

Under general anesthesia (= General anesthesia) one understands the reversible deactivation of consciousness, so an artificial sleep. This sleep state can e.g. used to perform an operation. The loss of consciousness is due to either Medicationthat are injected directly into the bloodstream via a venous catheter (so-called. TIVA = total intravenous anesthesia) or through a mask over the mouth and nose in the form of gases (so-called. Inhalation anesthesia) reached. Often both forms are combined in practice: The process of falling asleep is brought about by injection anesthetics (e.g. propofol), while the maintenance of sleep is ensured by gases (e.g. sevoflurane, desflurane). Such a combination is called "Balanced anesthesia" designated.
The state of deep unconsciousness is accompanied by a failure of the reflexes - including the breathing reflex. Therefore, the patient must be artificially ventilated during general anesthesia.
General anesthesia is always supported by the administration of strong painkillers (Opioids) and often supplemented with drugs that relieve the tension in the muscles (Muscle relaxants). General anesthesia can be used in many surgical procedures Regional anesthesia (e.g. spinal anesthesia, epidural anesthesia) can be added (for more details below under "Pain Therapy")
General anesthesia are also used in intensive care medicine to keep the patient in an artificial coma for a longer period of time (in severe cases, even for several months).
General anesthesia always carries some risk Side effects.
You can find more information under our topic: general anesthetic
Pain therapy
Pain therapy as a branch of anesthesiology can be divided into three areas:
- Preventive painkillers that prevent previously foreseeable pain (e.g. during operations) from occurring in the first place
- Short-term treatment of acute painful conditions, such as can occur in the wound area in the days after surgery
- Therapy of long-term pain conditions, such as those described as chronic pain e.g. occur with tumor diseases, chronic back pain or headache.
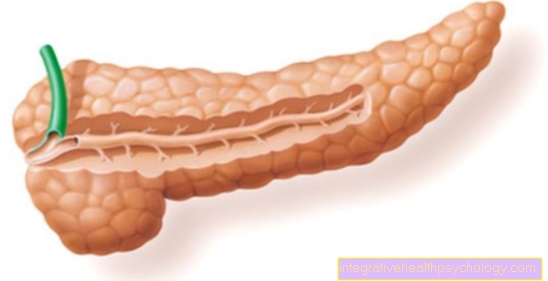
A wide range of drugs are available for treating this pain, which differ in their potency and in the form in which they are administered to the body. Oral pain relievers (Medicines to be swallowed) are available in the form of drops and tablets and are used for both mild pain (e.g. paracetamol) and severe pain conditions (e.g. opioids). Painkillers can also be introduced directly into the bloodstream via a venous catheter (so-called iintravenous application). The onset of action is significantly faster than in the case of oral intake; however, the drugs available are very similar to oral medication; Here too, opioids are often used for severe pain conditions. However, since the direct administration of the drug into the bloodstream carries the risk of overdosing, this form of pain therapy is rarely used in the home environment.
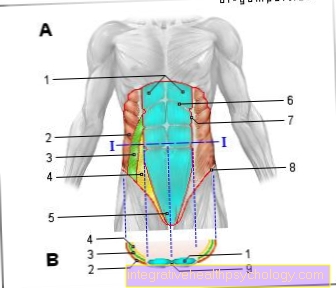
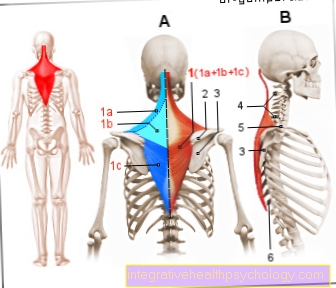
If freedom from pain is to be achieved in a certain region of the body, the use of Regional anesthesia procedure on. Here, a thin plastic tube is placed near a nerve. Rinsing the nerve with a pain reliever (here: local anesthetic) switches off the sensation of pain in all body regions that are connected to the brain via these nerves. This is done e.g. Use on nerves in the armpit area to perform operations on the arm or in the groin to be able to operate on the leg. In addition, the local anesthetic can be injected near the spinal cord. The freedom from pain then extends to the entire body region below the puncture site. Regional anesthesia procedures are often used in an operation, since this requires lower doses of painkillers and anesthetics that are detrimental to the circulation. The plastic tube can also be connected to a pump (so-called pain pump) in order to continuously deliver local anesthetic over a longer period of time. In this way, freedom from pain can be achieved for up to several weeks - in practice, the pain pump is usually not used for more than a few days as part of acute pain therapy. This is due, among other things, to the risk of infection at the injection site.
Another possibility of pain relief is the administration of medication through the skin (so-called. TTS = transdermal therapeutic system). A patch stuck to the skin continuously releases pain relievers (opioids) through the skin to the body.
Read more on the topic
- Pain therapy
- Femoral catheter
Note: pain patches
The region in which the plaster is stuck on (often in the area of the back) does not have to correspond to the location of the pain.
This procedure can also be used in long-term pain therapy.
All of the forms of pain therapy presented here can also be combined with one another.
Emergency medicine

Emergency medicine is an area of anesthesiology, but an interdisciplinary approach with the participation of specialists from various medical fields is often necessary. Often internists or surgeons complete further training in "emergency medicine". Emergency medicine extends to the area outside of medical facilities (Rescue medicine) as well as emergency care within a hospital. The task of emergency medicine is to restore and maintain acutely threatened vital functions. The vital functions include all organ systems that are important for survival: heart, blood circulation, lung, brain. In order to restore adequate cardiac function and an intact blood circulation, emergency medication is available that strengthen the heart's strength and make it beat rhythmically. The use of power surges (so-called Defibrillation) aims to make the heartbeat rhythmic. To with one Cardiac arrest Replacing the heartbeat can be a Chest compressions carried out, often combined with artificial ventilation of the patient, since the cardiovascular system and lung function are closely related.
Blood loss is often responsible for functional restrictions in the area of the blood circulation in emergency medicine. The aim of therapy is to stop the source of bleeding quickly and, if necessary, to compensate for the loss of blood by means of fluids or blood donations. Impending functional limitations of the brain, e.g. due to increased water accumulation in the head after an accident, therapy can also be given by administering medication.
Intensive care
Intensive care medicine is usually used in a hospital made in an intensive care unit. During your stay in an intensive care unit, you should life threatening conditions diagnosed and treated. In most hospitals, these highly specialized wards are also subdivided into specialist disciplines (e.g. neurointensive wards for neurological diseases, Cardio-intensive units for acutely life-threatening Diseases of the heart).
Intensive care units have a special complex equipment and a high ratio of skilled personnel to patients. The medical staff working here have often completed a corresponding specialist training, and employees of the nursing staff also mostly have specialist nursing training. An essential aspect of intensive care medicine is one detailed continuous monitoring of all vital functionslike heartbeat, Heart rate, Blood circulation, oxygen content in the blood, Awareness, etc. Further cornerstones of intensive care medicine are artificial ones coma, artificial respiration of the patient using ventilators, Pain therapy and maintenance and stabilization of all vital functions.