What are Cholinesterase Inhibitors?
Cholinesterase inhibitors are part of various drugs that, due to their diverse modes of action, can be used for very different diseases.
Cholinesterases increase the activity of certain cell connections, which are located both in the brain and in various organs such as the eyes or the bladder. The available cholinesterase inhibitors differ from one another so that the best possible active ingredient can be selected depending on the desired effect.
Nevertheless, the drugs can never specifically affect only one organ, so that the ingestion can also lead to side effects in other organs.

Indications for a cholinesterase inhibitor
Since the cell connections that transmit signals through the messenger substance acetylcholine can be found in very different organs of the body, there are also very different starting points and indications for choline sterase inhibitors.
On the one hand, the drugs can be used to treat a mild to moderate form of dementia of the Alzheimer's type. In this disease there is a deficiency of the messenger substance aethylcholine in the brain, so that one reduces the breakdown of the substance by taking cholinesterase inhibitors and tries to slow down the progression of the disease.
Whether this approach actually has a positive effect is, however, controversial and the use of cholinesterase inhibitors in Alzheimer's dementia should be weighed up on an individual basis. Completely different indications for choline sterase inhibitors arise in cases of emptying disorders of the bladder or bowel, such as those that can occur as a result of an operation.
The cholinesterase inhibitors increase the muscular activity of the bladder or intestinal wall and thus promote their emptying.
Because of this effect, another important indication for cholinesterase inhibitors is the rare muscle paralysis disease myasthenia gravis. In this disease, a defective action of the immune system destroys the sites of action (receptors) of the messenger substance acetylcholine on the muscle cells, so that the nervous system disrupts the activation of the muscles and thus leads to progressive paralysis.
If left untreated, the disease ends fatally in extreme cases due to paralysis of the respiratory muscles.
Cholinesterase inhibitors increase the concentration of acetylcholine at the point of transmission of nerves and muscles (motor end plate), so that the reduced number of receptors can be compensated and the course of the disease can be slowed down.
Read more on the subject at:
- Myasthenia Gravis
- Alzheimer's dementia
Which cholinesterase inhibitors are there on the market?
The cholinesterase inhibitors available on the drug market can be broadly divided into two groups.
- On the one hand, there are drugs that, due to their chemical properties, can penetrate the brain and are therefore used to treat dementia. These are the preparations with the active ingredient donzepil, galantamine or rivastigmine. There are drugs from different manufacturers and in different dosages, whereby the mechanism of action does not differ.
- The other large group of cholinesterase inhibitors are those that do not penetrate the brain and only reach all other organs of the body. The most common active ingredients on the market are neostigmine, pyridostigmine and distigmine. These are used, for example, to treat bowel or bladder emptying disorders. This group also has preparations with different trade names from different manufacturers.
The active ingredient and the effect of cholinesterase inhibitors
The cholinesterase inhibitors are a group of active substances that differ somewhat in their chemical structure but are characterized by basically the same effect.
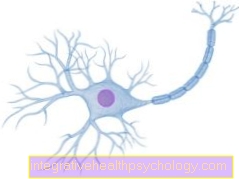
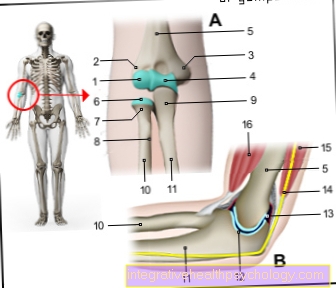
The site of action are the connections between nerve cells (synapses) and the connection between nerve and muscle cells (motor end plate). There signals are transmitted by means of the body's own messenger substance acetylcholine. This in turn is broken down by the so-called cholinesterases in order to regulate or stop the effect.
The cholinesterase inhibitors reduce the effect of cholinesterase and thus increase the effect of the released acetylcholine. This leads to an increased signal transmission at the synapses or the motor end plates.
This ultimately results in the effect of the cholinesterase inhibitor in increased activity of the muscles, for example of the bladder or intestine.
In the case of active substances that can also enter the brain and are used to treat Alzheimer's dementia, signal transmission between the cells is also amplified. By increasing the activity in certain brain areas, the memory and concentration should be improved or at least the mental degradation slowed down.
Read more on the subject under: Acetylcholine
Side effects of cholinesterase inhibitors
The cell connections on which the cholinesterase inhibitors develop their effect are located in very different organs throughout the body.
If a drug with a cholinesterase is used, only one organ can therefore never be targeted or only a certain effect can be achieved.
The active ingredient is distributed throughout the body, so that wherever the body uses the messenger substance acetylcholine, side effects can occur.
For example, cholinesterase inhibitors can:
- In the lungs, this leads to a constriction of the bronchi and increased secretion production, making breathing difficult.
- The heart rate may slow down (bradycardia).
- In addition, the activity of the sweat glands is increased, so that some people complain of increased sweating when taking it.
- Furthermore, it can lead to gastrointestinal complaints such as
- Nausea,
- Vomiting or
- Diarrhea coming.
- Side effects that could affect the brain usually do not occur.
- Most of the cholinesterase inhibitors used do not cross the so-called blood-brain barrier due to their chemical properties.
- Cholinesterase inhibitors, which can penetrate the brain, are only used when an effect in the brain is desired (as in Alzheimer's dementia). Then it is also possible for side effects to occur in the brain, which can be expressed, for example, by dizziness or hallucinations.
Interactions of Cholinesterase Inhibitors
Because of their effects on a large number of organs throughout the body, various interactions with other drugs can occur when taking cholinesterase inhibitors.
The prescribing doctor must therefore use the patient's further medication to assess whether interactions are to be feared and whether the cholinesterase inhibitor can be used.
- An important interaction occurs when a beta blocker is taken at the same time. Both drugs slow the heartbeat and, in combination, can lead to a life-threatening arrhythmia (AV blockage).
- Patients who use a spray to widen the bronchial tubes (for example in asthma) also have to fear an interaction, since the mechanism of action of the choline sterase inhibitor is opposite to that of the spray.
- In addition to this and other direct interactions in individual organs, many other drugs (possibly also herbal preparations!) Can influence the metabolism of the cholinesterase inhibitor.
- On the one hand, the breakdown of active substances in the liver can be inhibited and the effect can be increased. Conversely, it can also lead to an accelerated degradation, so that there is an insufficient effect as an interaction.
Because of this large number of possible interactions, the doctor who prescribes the cholinesterase inhibitor should be aware of all other drugs and substances that the patient is taking.
Read more about this under: Beta blockers and asthma therapy
Contraindications - When should a cholinesterase inhibitor not be given?
A cholinesterase inhibitor must not be given in the case of various diseases affecting different organs, as otherwise the disease can worsen and, in some cases, threaten life-threatening consequences.
First of all, there are diseases of the heart in which there is a disruption of the electrical conduction (AV block) or a heart rate that is too low.
Furthermore, cholinesterase inhibitors must not be given in diseases of the lungs that are associated with narrowing of the bronchi (for example bronchial asthma).
Another counter-sign is increased intraocular pressure. Otherwise, if there is a glaucoma (glaucoma), the worst case scenario is loss of the eye.
In addition, a cholinesterase inhibitor must not be used during pregnancy or breastfeeding. Another contra-sign is severe liver or kidney dysfunction.
dosage
The recommended dosage for cholinesterase inhibitors differs on the one hand depending on the active ingredient and on the other hand depending on the indication.
- The cholinesterase inhibitors Donezepil and Galantamine, which are approved for the treatment of Alzheimer's dementia, are, for example, often administered as plasters, with which about 10 mg of active ingredient is absorbed through the skin within 24 hours.
- Neostigmine, a representative of the cholinesterase inhibitors that do not work in the brain, is given into the blood in a single dose of 0.5 to 2 mg via a vein.
- Distigmin in the form of tablets contains 5mg of active ingredient and is usually taken once a day. However, if the liver or kidney function is impaired, a reduced dosage may also be necessary.
In any case, the attending physician will try to select the most suitable preparation in the dosage that is suitable for the patient.
price
If a cholinesterase inhibitor is medically indicated, both statutory and private health insurances will cover the costs.
For example, the price of the active ingredient distigmin is the equivalent of two euros per tablet. The other active ingredients differ only slightly in price.
The cost of treating Alzheimer's dementia with one of the approved cholinesterase inhibitors is between 1,000 and 2,000 euros per year.
The use in the form of capsules is usually cheaper than in the form of plasters.
Cholinesterase inhibitors and alcohol - are they compatible?
In principle, caution is advised when consuming alcohol when taking medication. There is no direct interaction with the cholinesterase inhibitor, but since alcohol can also affect the signal transmission of nerve cells, consumption should be avoided if possible.
However, small amounts such as a bottle of beer or a glass of wine in the evening are of little concern.
However, larger amounts can have a strong impact on the effect.
Alternatives to a cholinesterase inhibitor
The alternatives to cholinesterase inhibitors depend on the disease or the complaints that are to be treated. In the therapy of Alzheimer's dementia, on the one hand, plant products are available, for example based on gingko extract.
On the other hand, there is an alternative active ingredient that attacks another messenger system in the brain, memantine.
For the treatment of glaucoma, drugs are preferred which, unlike cholinesterase inhibitors, do not increase the effectiveness of the acetycholine-mediated signal transmission indirectly but directly, which leads to a reduction in intraocular pressure.
Read more on the subject under: Green Star
Poisoning with a cholinesterase inhibitor
Cholinesterase inhibitor poisoning can result from excessive use of the drug.
Depending on how high the overdose turns out to be, different signs of intoxication occur.
A moderate overdose can lead to increased tears and saliva flow, muscle twitching, decreased respiratory drive and hypothermia.
If the overdose is severe, symptoms such as nausea, vomiting and a drop in blood pressure may occur.
In the worst case scenario, respiratory paralysis or cardiovascular failure can result in death.
In the case of poisoning with a cholinesterase inhibitor, an antidote (atropine) may be given.