Aortic dissection
definition
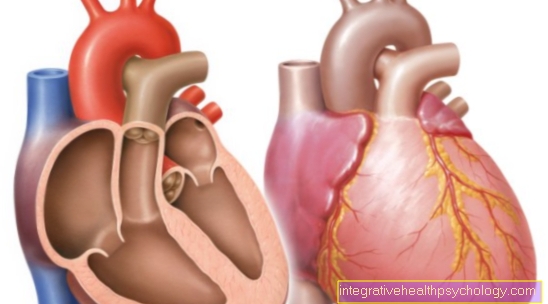
The term aortic dissection (syn. Aneurysm dissecans aortae) denotes a splitting (Dissection) the wall layers of the main artery (aorta). As a rule, the innermost layer of the wall tears suddenly (Tunica intima) and as a result bleeding between the wall layers (the aorta, like any artery, is made up of the three wall layers Tunica intima, Tunica media and Tunica adventitia built from the inside out).

Through the crack in the Tunica intima Blood escapes from the lumen of the main artery through the high pressure in the vessel between the wall layers, where it creates a new space (false lumen) between the intima and adventitia. Depending on how high the blood pressure is in the main artery and how resistant it is Media the dissection may extend only a few millimeters or the entire length of the aorta. In the majority of cases it is thoracic aorta (lying in the chest), most often directly above the aortic valve in the ascending part of the aorta (ascending aorta).
In the clinic, aortic dissection is divided into types A and B, which will be discussed below. In addition, a distinction is made between acute and chronic dissection. A chronic dissection is present if the symptoms have existed for more than two weeks after the acute event; in some cases, a chronic dissection that lasts for several years occurs. The following article focuses on acute dissection.
differentiation
Aortic dissection type A
According to Stanford, there is a simplified and clinically applied classification of aortic dissection that only distinguishes between A and B. In the Stanford type A aortic dissection, the intimal tear is in the area of the Ascending aorta (the ascending part of the aorta, which arises directly from the left ventricle and which is connected at the top by the aortic arch). An acute type A dissection is always an immediate indication for emergency surgery to prevent rupture. A rupture (tear) of the aorta in the Ascendens part would result in bleeding into the pericardium and immediate heart failure or tamponade of the pericardium, which would also lead to death. The standard of surgical therapy here is replacement of the aorta (usually ascending) with a vascular prosthesis made of Goretex. If the part of the aorta close to the valve is affected, a prosthesis with an integrated prosthesis of the aortic valve is usually used; the body's own aortic valve can rarely be reconstructed. A chronic type A dissection (symptomatic for more than 2 weeks) also usually has to be treated surgically, but the intervention does not have to be an emergency.
Read more on the topic: Aortic dissection type A
Aortic dissection type B
All dissections of the Descending aorta (descending part of the main artery behind the aortic arch) counted, or everything below the outlet of the Left subclavian artery. With type B dissection, the risk of rupture is much lower than with type A dissection. Since the mortality with uncomplicated type B dissections after surgical treatment is almost 25% higher than with purely drug treatment with about 10%, one usually limits oneself to conservative therapy. Exceptions to this are life-threatening conditions such as an impending or already completed rupture. Less dramatic complications can often be corrected interventionally, using catheters with stents inserted through the skin into the vascular system.
Read more on the topic: Aortic rupture
Causes of aortic dissection
As most important risk factor an aortic dissection is the arteriosclerosis to call one Calcification of the inner vascular layer of the arteries (promoted by increasing age, smoking, diabetes, high blood lipid levels, etc.). A weakness of the tunica media (so-called Media degeneration) is predisposing to dissection. This usually leads to a widening in the area of the ascending aorta, most often caused by high blood pressure. Less often can congenital connective tissue diseases as the Marfan's Syndrome or Ehlers-Danlos Syndrome cause a weakness of the media layer. One is rarer Coarctation of the aorta (a congenital tightness in the area of the aortic arch) or inflammatory diseases of the aorta (so-called. Vasculitis) Causal in an aortic dissection. Medical interventions such as cardiac catheterization can also encourage aortic dissection. External force is rather uncommon for the development of an aortic dissection, it rather results in bruises or with strong force the main artery is torn off.
Diagnosis of aortic dissection
For a patient with typical symptoms, that is Sudden back, chest or abdominal pain the suspicion is confirmed if high blood pressure, one Pulse or blood pressure difference between the right and left side of the body or a so-called. diastolic heart murmur (this can be heard by the doctor with the stethoscope). If there is a suspicion of a dissection, this must be confirmed or excluded immediately using suitable imaging. The Computed Tomography is very suitable for this, as it is available in many hospitals and, unlike magnetic resonance imaging or angiography, only takes a few minutes. If no CT is available, an aortic dissection can also be easily recognized by means of echocardiography (ultrasound of the heart). The emergency doctor can also carry out this examination if he has an ultrasound device with him in the ambulance and can thus save important minutes.
Differentiation from myocardial infarction using an EKG
Due to the typical symptoms with sudden onset of violent chest pain, an aortic dissection is sometimes clinical difficult to differentiate from a heart attack. An EKG can be written here, where a heart attack can be shown. A Aortic dissection, on the other hand, does not produce any typical changes in the EKG, which only shows the electrical conduction in the heart and can often be normal even with an acute life-threatening dissection.
roentgen
Conventional X-rays play a subordinate role in the diagnosis of cardiovascular diseases. While a chest x-ray may show evidence of an acute dissection, this is not always the case. In the case of the typical dissection patient with severe pain and unstable clinical condition, no time is spent on an X-ray, but in the potentially life-threatening condition, a CT or echocardiography is performed immediately, with which the suspicion can be confirmed or excluded.
Read more on the topic: Chest x-ray (chest x-ray)
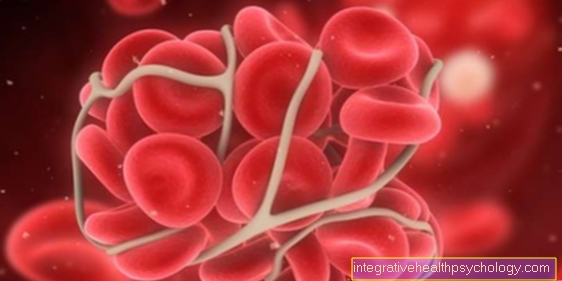
D dimers
The D-dimer is a cleavage product of fibrin, which is obtained during the coagulation process. The laboratory value is usually determined to rule out a thrombosis. Research has shown that a Normal D-Dimer value excludes an aortic dissection with a probability bordering on 100%. On the other hand, an increased D-dimer value is not very meaningful for the presence of an aortic dissection, as the value can increase in various diseases and the time window between the appearance of symptoms and the blood sample also plays a role.Imaging (CT, angiography, echocardiography, MRI) is currently always performed if a life-threatening aortic dissection is suspected, since the D-dimer is only of indicative importance as a laboratory value.
Symptoms of aortic dissection
The so-called Leitsypmtom, which more than 9 out of 10 patients describe with an acute dissection, is an acute onset, very severe pain in the chest or abdominal area or in the back. The pain is described by those affected as very intense and stabbing or tearing, sometimes the patients lose consciousness due to the pain intensity alone. With type A dissection, the pain is felt more in the chest area, with type B dissection more between the shoulder blades and into the abdomen and back. If a wandering pain occurs, this speaks for a spreading dissection.
In rarer cases, the dissection is completely painless, so that it is noticeable as part of an incidental finding. Depending on the level at which the dissection is located and which outgoing blood vessels are affected, complications can arise in a wide variety of organ systems. If the heart is involved, it can lead to shortness of breath and shock symptoms. If the arteries supplying the brain are affected, stroke-like symptoms can occur. In the case of insufficient blood flow to the intestines or kidneys, severe abdominal or flank pain occurs. If the blood supply to the arms and legs is reduced, pain in the extremities occurs. An undersupply of the spinal cord with paraplegia is also possible.
Read more on this topic at: Symptoms of aortic dissection
Treatment of aortic dissection in line with guidelines
A medical guideline gives a recommendation for the therapy and diagnosis of certain clinical pictures. In contrast to the guideline, it is not binding, but must always be adapted to the patient. A classification system differentiates between different quality levels, with an S3 guideline being more important than an S1 or S2 guideline.
Currently exist several recommendations for the management of patients with aortic dissection (e.g. from the German Society for Vascular Surgery or the European Society for Cardiology). There is currently no generally recognized S3 guideline, so the Ultimately, the decision is always made by the attending physician lies. However, general standards in diagnostics (e.g. imaging procedures such as CT, echocardiography or MRT and angiography) and therapy (operative vs. interventional vs. medicinal treatment) are handled similarly in all hospitals in Germany (see Treatment / Therapy).
Therapy of aortic dissection
When treating aortic dissection, it is important to distinguish between acute and chronic, as well as between type A and type B dissections. An acute type A dissection is always an immediate indication for emergency surgery, as the risk of a fatal rupture increases with time. A chronic type A dissection usually has to be corrected surgically, but the risk of rupture is much lower, which is why the operation does not have to be performed as an emergency. With type B dissection, the risk of rupture is much lower than with type A, so that if the course is uncomplicated, it is treated conservatively (medication). Analyzes have shown that the 30-day mortality with surgical treatment of a type B dissection is around 30%, whereas the 30-day mortality with purely medicinal treatment is only 10%. In the event of complications such as insufficient blood flow in various organ systems (see symptoms), endovascular / interventional use of catheters, e.g. be worked with stents. A type B dissection is only operated on in selected cases, including an impending or already existing rupture, increasing enlargement of the aortic diameter, in patients with Marfan's syndrome or in the case of retrograde expansion into the ascending aorta.
surgery
An acute type A dissection requires immediate emergency surgery to prevent a fatal rupture. The patient must be transported to a specialized center for this, as this is a major procedure. As a standard, the ascending aorta is replaced by a vascular prosthesis made of Goretex during the operation. If the dissection affects the aorta in the immediate vicinity of the aortic valve, a vascular prosthesis with an integrated aortic valve replacement is usually used. In rare cases, the patient's own aortic valve can be preserved and reconstructed. Depending on the patient's condition and previous illnesses, the mortality within the first 30 days after the operation is between 15 and 30%. In the case of type B dissection, surgery is only indicated in certain cases (see therapy). Depending on the length / extent of the dissection, in which vital arterial branches can be blocked, the mortality of the operation is between 25 and 60%. In the case of the operation of the chronic type B dissection, on the other hand, the mortality is less than 10%.
You might also be interested in: Aortic prosthesis
When do you need an operation?
With type A, an operation is always indicated. Without surgery, the disease can lead to death within a few days. For type B aortic dissection, surgery is only indicated if there are complications. These consist of already existing bleeding or obstruction of vital arteries due to the pressure of the split vessel.
Complications of the operation
The operation of an aortic dissection is a really serious procedure, which can bring many complications. Since some important vascular branches have to be replaced by vascular prostheses during the operation, the mortality rate in the first 30 days is very high. This is an averaging of the statistics in order to make different procedures comparable. Complications include bleeding, which can cause pressure to constrict important adjacent structures. Basically, it must be said that the clinical picture of an aortic dissection can be particularly serious and life-threatening, so that a patient can often only benefit from the operation in comparison.
You might also be interested in this topic: Aortic rupture - that's how dangerous it is
Duration of the operation
Different procedures are required depending on the location and extent of the aortic dissection. From a stent insert (a stent) to a complete replacement of the vascular segment, the various procedures can take different lengths of time. In some cases, a connection to the heart-lung machine is required, which requires careful preparation and follow-up. Thus the duration of the operation can be several hours.
How does the operation work?
Depending on the surgical procedure, a stent is either inserted via a large blood vessel on the thigh, where wire (catheter) is pushed into the blood vessel to the crucial point, or in a so-called open procedure to open the chest, with careful preparation of the relevant structures . With this open procedure, the heart-lung machine is also necessary, which switches off the affected area of the vessel from the bloodstream and leaves the surgeon freedom to edit and replace the vascular section.
Life expectancy with aortic dissection
Life expectancy with an aortic dissection depends largely on whether it is type A or B., with type B generally having a better view. In addition, life expectancy naturally depends on the Previous illnesses of the patient and its clinical condition at the time of the acute event. Next to it has one ruptured dissection (type A or B) without immediate emergency medical treatment has a very poor prognosis from a few minutes to a maximum of hours or days. Without surgery, the mortality rate from a type A dissection increases by around 1% per hour. On the other hand, if these patients have survived the operation and the critical days and weeks afterwards, they still have a relatively age-appropriate life expectancy as long as no late complications occur. At Type B dissections life expectancy is quite good apart from ruptured dissections. Around 80-90% survive the first year with conservative treatment and complications can often be resolved with interventional methods (catheters and stents). If the course is uncomplicated, life expectancy is usually not drastically reduced.
forecast
Due to new surgical techniques and advances in emergency medicine, the prognosis of aortic dissection has improved dramatically. Nevertheless it remains acute aortic dissection a dangerous clinical picture with a relatively high Lethality (Mortality). About 20% of the patients with the acute clinical picture no longer reach the hospital alive. Another 20 to 25% die in the clinic before the diagnosis is made. Without therapy, the death rate increases by one percent per hour. Early detection of the emergency is crucial for the prognosis, so that an operation can be initiated before there is an insufficient supply of the brain, intestines or extremities or serious cardiac complications. It is also crucial whether the dissection has already ruptured, which drastically worsens the prognosis. While previously only 1 to 2 out of 10 patients with type A dissection survived the first week and hardly any one survived the first year, today 90% of patients survive an operation and 80% the following month. Without surgery, however, only about half of the patients with type A dissection survive the first month after the acute event. In the case of patients with type B, however, 80-90% of the patients survived the first year on purely drug therapy.


















.jpg)