Aplastic anemia
introduction
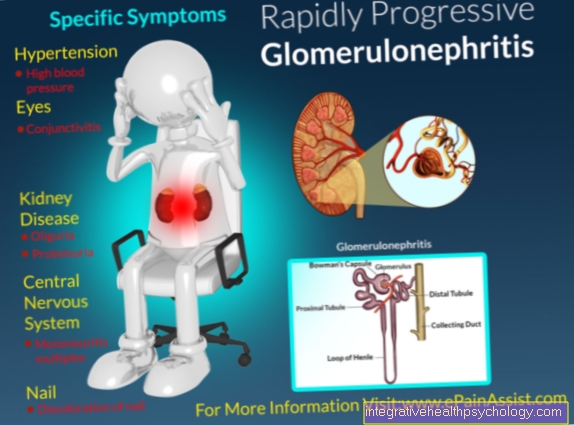
Aplastic anemia is a group of different diseases, the commonality of which is a weakness (Insufficiency) of the bone marrow, which leads to decreased production of blood cells. This not only results in anemia, i.e. a reduction in red blood cells (Erythrocytes) or the hemoglobin value, but also to a deficient formation of immune cells, especially the so-called neutrophil granulocytes (Neutropenia), as well as the platelets (Thrombopenia). If all three named cell groups are affected, one speaks of one Pancytopenia. In most cases the cause is autoimmune diseases, but aplastic anemia can also be caused by chemotherapy or be congenital.

How does aplastic anemia occur?
Aplastic anemia, also known as panmyelopathy, is not a single disease, but a group of different diseases and syndromes that ultimately lead to a deficient production of blood cells due to weakness of the bone marrow.
The causes of such bone marrow insufficiency can generally be congenital or acquired, although the acquired forms are much more common. The congenital forms include, in particular, Fanconi anemia and Diamond-Blackfan syndrome; there are also other rare enzyme defects.
The main triggers of acquired aplastic anemia are autoimmune reactions against the bone marrow, the cause of which can often not be determined. Other haematological diseases such as myelodysplastic syndrome (MDS).
Another important trigger are certain drugs, especially cytostatic drugs used in chemotherapy, have a toxic effect on the bone marrow, as they often have to be given in high doses. Other drugs that in rare cases can lead to aplastic anemia are metamizole (Novalgin) or the neuroleptic clozapine.
Aplastic anemia after chemotherapy
Most chemotherapy drugs work by attacking rapidly dividing cells, primarily cancer cells. However, other cells in the body are also attacked, including stem cells in the bone marrow, which form the blood cells so that they sink during chemotherapy.Normally, however, the bone marrow is not completely destroyed, it regenerates after the end of therapy. In rare cases and depending on the therapy protocol, however, the bone marrow may no longer recover after chemotherapy and aplastic anemia may occur.
Read more about chemotherapy
Aplastic anemia after Metamizole (Novalgin)
In addition to cytostatic drugs, aplastic anemia can also be caused by other drugs, important examples are metamizole (Novalgin) and the neuroleptic clozapine. Bone marrow failure is independent of the dose and is based on the body's hypersensitivity to certain substances. Although this side effect is extremely rare, it must be taken into account, especially if these drugs are given for the first time or in high doses!
Symptoms of aplastic anemia
The symptoms of aplastic anemia are caused by a lack of the respective blood cells. There are three lines of blood cells:
- the red blood cells (Erythrocytes), mainly responsible for the transport of oxygen
- the white blood cells (Leukocytes), Cells of the immune system
- the platelets (Platelets), Part of the blood clotting system
If there is a shortage of erythrocytes, the cells in the entire body can no longer be supplied with oxygen as well. The main consequences are a feeling of weakness, circulatory problems, paleness and ringing in the ears. This is treated from a critical Hb level with the transfusion of so-called red cell concentrates.
A deficiency of leukocytes cannot be subjectively noticed by the patient, but it is the most dangerous effect of aplasia. This is mainly due to a subgroup of white blood cells, the neutrophils. If these are absent, neutropenia occurs. The patient is no longer adequately protected from opportunistic pathogens - that is, pathogens that are actually relatively harmless and only become dangerous if the immune system is weak. Normal infections can then also be very drastic and life-threatening.
The platelet deficiency is also often not noticed at first. The poor coagulation can lead to bruises more quickly. However, it becomes dangerous when the platelets are very low, which can lead to dangerous internal bleeding.
Therapy and measures
The treatment of aplastic anemia is very complex and would go beyond the scope of such an article. The aim of the therapy is to cure the aplastic anemia by combating the cause. Depending on the cause, it must therefore be planned individually by the attending physician. It also depends on the age of the patient, the severity of the disease, and other factors. A "last resort" is allogeneic stem cell transplantation, also known as bone marrow transplantation. However, this very effective option is fraught with many risks, which is why its use must always be weighed up individually by an experienced haemato-oncologist.
Another very important component is supportive therapy, which includes all medical measures that are carried out in an accompanying and supportive manner. Studies have shown that supportive measures can significantly increase the probability of survival.
First and foremost is infection prophylaxis, because for patients with aplastic anemia, even commonplace infections and actually relatively harmless such as mold represent an acute life threat. This includes paying attention to special hygiene, i.e. regular hand washing or disinfecting, no contact with colds or even so-called reverse isolation in the hospital. It may also be necessary to take preventive antibiotics. Furthermore, an "aplastic diet" should be adhered to, for example:
- Use up opened food within 24 hours, otherwise discard
- no fresh food that cannot be peeled (especially no salad!)
- Cook or cook well food that has not been industrially packaged
- no consumption of raw milk products
These measures do not have to be fully adhered to by every patient; the treating doctor should always decide on the details.
Further supportive measures are the transfusion of blood products, the stimulation of the bone marrow and the treatment of the side effects caused by the respective therapy.
Life expectancy in aplastic anemia
Life expectancy depends on several factors. Initially, aplastic anemia can be divided into three degrees of severity (moderate, severe, very severe). The classification is based on the number of different blood cells. The fewer blood cells the bone marrow makes, the more serious the disease. The number of neutrophils, which belong to the white blood cells, and the age at diagnosis are the most important prognostic factors. A low number of granulocytes suggests a severe course with a poor prognosis, as the immune defense system, which is actually harmless, such as fungi (e.g. Aspergillus) is severely impaired. If the disease is mild, however, life expectancy is hardly limited. In the case of moderate and severe courses, so-called allogeneic stem cell transplantation (ASZT) can be carried out as the last measure, if the disease cannot be controlled by other measures. This therapy is a very drastic measure in which the patient's bone marrow is destroyed and then replaced by the one donor. ASZT has many side effects and can be life-threatening in the case of rejection reactions, but the severe form of aplastic anemia is also often fatal.
Supportive measures, i.e. the prevention and treatment of complications, are also very important. Infection prophylaxis is very important here, but bleeding and anemia must also be carefully monitored and treated if necessary.
What are the chances of recovery?
The chances of recovery depend on the course and severity of the disease, as well as the individual physical condition and age of the person affected. In general, younger patients have better therapeutic results than older ones. If a stem cell transplant has to be carried out in the case of severe disease, the chances of recovery depend largely on this. With a suitable donation from a family member, about 80% of the sick are still alive after 5 years. If the donation is from an unrelated donor, 70% are still alive. Also, stem cell transplants from bone marrow produce better results than stem cell transplants from peripheral blood. If a stem cell transplant is not possible, intensified immune system-suppressing therapy is used. Here the 5-year survival rate is approx. 80%, whereby with this therapy no complete cure but only an improvement of the symptoms can be achieved. As almost always, starting therapy early has a positive effect on the course of the disease and the chances of recovery. However, recurrences, i.e. a new disease gene after successful therapy, are not uncommon, so patients must be checked regularly even after therapy.
Also read our article on Stem cell transplant
Is Aplastic Anemia Fatal?
Yes, aplastic anemia is an acutely life-threatening disease. If left untreated, it is fatal in 70% of adults. The aplastic anemia is characterized by the lack of all different blood cells, from a certain level this is no longer compatible with life, especially serious infections and heavy bleeding are problematic here. It is all the more important to start therapy as soon as possible, preferably in a specialized center for hematology!
Leukemia and aplastic anemia
Particularly in the case of special congenital forms such as Fanconi anemia, which results in mutations in the DNA repair system, other hemato-oncological diseases such as myelodysplastic syndrome or a form of acute leukemia (AML) can develop from aplastic anemia. Because of the aplastic anemia, this leads to a malignant change in the bone marrow stem cells from which the blood cells arise. This causes immature and non-functional blood precursor cells to be released into the blood.
On the other hand, aggressive, high-dose chemotherapeutic agents are also administered in acute leukemia, which, as mentioned above, can lead to aplastic anemia in rare cases.
Further information
- anemia
- Bone marrow
- Erythrocytes
- Thrombopenia
- Autoimmune diseases
- chemotherapy
- Metamizole
- allogeneic stem cell transplantation (ASZT)
- hematology