Treatment of hip osteoarthritis from a physiotherapeutic point of view
Synonyms
- Coxarthrosis treatment
- Hip osteoarthritis treatment
- Rehabilitation for hip osteoarthritis

General recommendations for hip osteoarthritis
- Movement / activity without strain within the framework of the current resilience of the hip joint instead of protection
- Everyday stress such as climbing stairs, long hikes, lifting and carrying weights, reducing knees and doing them consciously and economically
- Avoid sitting deeply, use an armchair and possibly wedge cushions or special arthritis seat cushions
- Strength training, mobilization, balance, endurance and fitness training
- Recommended sports: functional gymnastics with strength-stretching, coordination and balance exercises, pendulum exercises to compensate for stress on the joints in everyday life, medical strength equipment training, cycling, possibly with an E.Bike or bicycle ergometer, swimming, aqua jogging
- Use group offers such as rehabilitation sports or senior sports in a club
- Avoid jogging, skiing, tennis, squash, soccer
- Weight reduction, already at 5% weight reduction there is a clinically relevant relief of the hip joint
- Healthy, balanced nutrition, Avoid consumption poisons
- Food supplement with chondroitin sulphate, hyaluronic acid
Hip osteoarthritis: painful problem area
- Pain in the area of the hip joint, groin, buttocks, equilateral knee joint, muscle pain, nocturnal pain
- Starting pain in the morning after sitting for a long time
- Pain amplification - tiredness and exertion pain during the day after prolonged walking, climbing stairs or hiking, after carrying heavy objects or gardening
- Primary or secondary back pain as a result of hip osteoarthritis
Appointment with a hip expert?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The hip joint is one of the joints that are exposed to the greatest stress.
The treatment of the hip (e.g. hip arthrosis, hip impingement, etc.) therefore requires a lot of experience.
I treat all hip diseases with a focus on conservative methods.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Hip osteoarthritis: physical therapy for the problem area of pain
- Heat application about fango, hot role
- Transverse stretching, transverse friction and trigger point treatments
Transverse expansion are performed passively by a therapist. The transverse stretch is transverse (in contrast to the longitudinal stretch, which the patient can carry out independently) to the course of the muscle and can be used for pain relief and as preparation for a longitudinal stretch.
Transverse frictions are also carried out passively by a therapist. The tendons of the affected muscles are worked across their course at the bone attachment. The fascia ball offers a possibility of self-treatment.
In the Trigger point treatment a therapist treats the local muscle hardening, especially in the hip flexors, splay, splay and external torsion muscles of the hip joint with various techniques. The fascia ball offers a possibility of self-treatment.
- Ice cream application, curd wrap
- Baths
- Electrotherapy, also in the form of a TENS device for the home
- Bemer therapy
The use of electromagnetic fields can lead to a regeneration of the cartilage and bone tissue in the arthritic joint. Particularly in combination with other pain and movement therapies, pain relief and functional improvement can be achieved.
- Medical taping
In medical taping of coxarthrosis, elastic tapes are applied to the skin in a specific form. The aim is not to immobilize the joint, but rather to relieve pain and improve mobility by acting on the muscles (reducing tension, improving metabolism) and the joint (improving the feeling of movement).
- Connective tissue - fascia treatment for hip osteoarthritis:
- In addition to stretching and strengthening the muscles around the hip joint, the treatment of the connective tissue around the hip joint has a pain-relieving and movement-enhancing effect. This treatment can be considered passive Connective tissue massage / friction techniques by a physiotherapist or as personal therapy.
- With the help of the fascia roll and the fascia ball, adhesions of the connective tissue are loosened, elasticity and blood circulation are improved.
- Dosage: 2-3 / week, 10-20 times over the affected pain area until there is significant relaxation, longer if the pain is more severe. The pressure on the connective tissue surface to be worked on can be varied by supporting the hands.
- The worked muscle areas should not be tensed while rolling out despite the pain provocation.
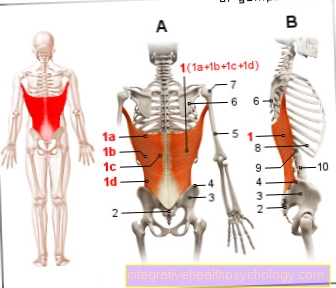
- Lower back fascia:
Starting position: Lie on your back over the roller, hands supported backwards
Exercise execution: Roll out the lumbar area over a small area piece by piece from the beginning of the lumbar spine to the sacrum
Alternative starting position: Stand against the wall, roll between the lumbar area and the wall
- External rotators gluteal fascia:
Starting position: Sit on the roll or the fascia ball (more selective)
Exercise execution: Shift your weight to one side of your buttocks, look for the pain point in the pain area, roll back and forth over a small area
- Lateral hip joint fascia:
Starting position: Lying on the side on the affected leg over the fascia roll, other leg placed in front of it, hands propped up in front of the body
Exercise execution: In the pain area, roll out the entire area between the hip joint and knee over a small area
Alternative starting position: Stand sideways against the wall, roll between your thighs and the wall
Hip osteoarthritis: the problem area is restricted mobility and reduced strength

- Often restricted directions of movement are the internal rotation, extension, splaying and flexion of the hip joint
- This often results in restricted movement of the spine, the knee and ankle joint with poor posture and a changed gait pattern ("limping")
- Loss of strength in the hip, leg, foot and trunk muscles
- Muscular imbalances (The optimal cooperation of all joint-guiding muscles that are necessary for movement is known as muscle balance. Loss of strength, tension and muscular shortening lead to an imbalance (Muscular imbalance) in the tension between agonist (player) and antagonist (opponent) and in the cooperating muscle chains.) In hip osteoarthritis, the hip flexor muscles in particular are over-proportionally stressed, which in turn leads to inhibition and loss of strength in the hip extensor muscles.
- Weak coordination and balance with the risk of falls
Physiotherapeutic techniques and exercises for the problem area of restricted mobility
Manual therapy for hip osteoarthritis
Aim: Pain relief, increased range of motion, metabolic improvement in the joint and counteracting the capsular contracture.
The current resting position of the hip joint in the supine position is chosen as the starting position for manual therapy in coxarthrosis. This often corresponds to a slight flexion and outward rotation position of the joint. So that the patient can really relax, it is advisable to "hang up" the affected leg in the sling table.
From this position the joint is then relieved with intermittent traction (pull) and / or vibration techniques. This has a relaxing effect on the muscles, the improvement in the elasticity of the joint capsule leads to improved freedom of movement of the hip joint, the surrounding tissue is decongested and the pain relief achieved is often reflected in the improved gait pattern immediately after the treatment.
After passive joint mobilization has taken place, the patient can further consolidate the gained range of motion through active exercises in the sling table while the sling reduces the weight of the leg.
A second useful way of increasing the freedom of movement of the hip joint is to mobilize the joint from the prone position. Above all, the hip extension and the internal rotation are improved with the aim of achieving a more fluid sequence of movements when walking in the standing leg phase.
Manual therapy is also used for secondary movement restrictions and pain in the area of the sacrum and the lumbar spine caused by hip arthrosis.
Dosage: 2/3 per week
Pendulum exercises for hip osteoarthritis
The pendulum exercises can be done independently. To do this, the patient stands sideways with his sound leg on a step and holds on to the banister. The affected leg is now loosely swung back and forth within the freedom of movement of the hip joint. To exert a pull on the hip joint capsule, a weight cuff can be attached to the affected leg for support. The pelvis should be kept as still as possible during the pendulum exercises so that the movement takes place in the hip joint and not in the lumbar spine.
Dosage: daily
Muscle stretching techniques for hip arthrosis
Due to the muscle shortening caused by the coxarthrosis and the resulting restrictions in movement (among other causal factors), the hip flexors, the splay muscles and the external rotors of the hip joint must be stretched.
In preparation for the stretching, we recommend a relaxed, general warm-up program (e.g. on the bicycle ergometer) and passive, soft transverse stretching and friction of the shortened muscles by the physiotherapist.
This is followed by the actual active / passive stretching techniques (e.g. postisometric relaxation - PIR link stretching) for the shortened muscles.
All important stretches are explained to the patient as homework as self-exercise.
Dosage: 2/3 per week, detailed description of the stretching techniques and the execution under stretching
Hip flexion stretch

Starting position
Lie on your back, the affected leg in the overhang on the edge of the table, the sound leg is fixed in flexion on the body.
Exercise execution
the affected leg is left for 5-10sec. raised in the direction of hip flexion, 5-20sec. relax, while letting the leg sink further towards the floor, repeat the procedure 3 times = 1 series, a total of 4 series of tension / relaxation and stretching
Another option for hip flexion stretching from the side position.
Stretching the back thigh muscles

Starting position
Lie on your back, stretch the affected leg towards the ceiling, while stretching the calf muscles, pull your foot towards your nose, your hands support you under the thigh
Exercise execution
the leg will be for 5-10sec. stretched against the hands towards the floor, 5-20sec. relax and go further into the stretching position, repeat the process 3 times = 1 series, a total of 4 series of tension / relaxation and stretching
Stretching the hip muscles


Starting position
Lateral lunge with hold on the back of a chair, the affected leg is extended
Exercise execution
the foot is anchored in the ground for 5-10sec. and stretched down into the ground, 5-20sec. relax and at the same time bend the bent leg further towards the floor, the affected leg remains extended, repeat the procedure 3 times = 1 series, a total of 4 series of tension / relaxation and stretching
Alternative starting position
It is on a chair, the affected leg is placed with the foot on the thigh of the healthy leg, with the hand supporting the opening of the hip
Exercise bath
Active exercise therapy in warm water is recommended, as the buoyancy of the water relieves the hip joint, the warmth relaxes the muscles and allows greater range of motion to be moved with less pain.
Strength training can also take place in the water by moving against the water resistance and using equipment.
Important
Pay attention to evasive movements! It is therefore advisable to practice exercise therapy in the water under the guidance of a physiotherapist.
Exercises on the problem area of strength and coordination
The increasing pain and restricted mobility associated with hip osteoarthritis, and the resulting rest, cause a significant loss of strength in the muscles surrounding the hip, the leg muscles and the trunk muscles.
Intensive preoperative strength training helps to postpone hip replacement surgery for longer and offers the chance of improved preoperative quality of life and a more optimal postoperative result. This can be seen in faster postoperative mobilization and a lower frequency of dislocation (risk of "balling out" the prosthesis, see: Hip dislocation after a hip prosthesis.)
Even after a hip endoprosthesis (artificial hip joint), the existing force reductions are only made up to a small extent. In follow-up examinations 6 months after the operation, only 50% of the strength endurance was measured in a comparison of strength ratios with healthy subjects. A lack of strength in the area of the hip extensor muscles and abdominal muscles worsens the prognosis with regard to the durability of the prosthesis. These investigations speak clearly in favor of intensive pre-operative strength, coordination and mobilization training.
General training recommendation for hip osteoarthritis:
- Dosage: 2/3 week
- 3-6 series / muscle group with 20-30 repetitions, slow execution, at the end of the number of repetitions you should feel a clear feeling of exertion (intensity 40-60% of maximum strength)
- Regular training instead of individual load units with high intensity
- Continue to breathe regularly during exercises or endurance exercise, avoid pressure breathing
- Possibly mirror control to avoid evasive movements during the exercises
- Avoid aggravating pain through exercise or training
A particular focus in muscle strengthening is the entire musculature surrounding the hip, as pain and shortening reduce the strength potential, especially the hip extension, splay and twist muscles are affected.
In addition, when choosing an exercise, emphasis should be placed on strengthening exercises for the core muscles, as the restriction of movement of the hip joint often results in posture and gait changes and back pain.
Small supporting devices for the home:
Theraband, Elastiband, wrist weights, unstable surfaces such as mats, air pads
In addition, the patient can be introduced to medical strength training on equipment. This can take place in the physiotherapeutic practice in individual or group therapy, as part of a rehab sports program or in the fitness studio (requirement: functional equipment and good guidance and control).
Exercise examples: Strengthening the back muscles, buttocks and back leg muscles with Theraband
Strengthening of the back muscles in the lumbar area and the back thigh muscles

Starting position:
Lie on your back with legs hip-width apart, feet close to your buttocks, a Theraband stretched across the pelvis
Exercise execution:
Starting at the lumbar spine, roll up and hold vertebrae by vertebra against the resistance of the Theraband, then unroll again in the same controlled manner.
In order to strengthen the back muscles of the legs in particular, put your feet on your heels and pull your heels towards your buttocks without moving.
Beware, the exercise is very crampy!
Strengthening of the hip splaying muscles, these centers the hip joint head in the socket, which is also decisive for the postoperative function of the artificial hip joint

Starting position
Lying on the side or forearm support on the side, front hand propped up, the upper leg is extended, the lower leg is bent
Exercise execution
lift the affected leg towards the ceiling and lower it again
Important: the heel leads the movement, the pelvis must not roll backwards
Caution: please do not perform the exercise in forearm support with a hip joint prosthesis
Strengthening the hip splaying and straightening muscles in the seat

Starting position:
Upright seat on a stool, lower legs open, Theraband in 8th loop around the thighs
Exercise execution:
the thighs open and close against the resistance of the ligament, feet remain standing, upper body erect
Strengthening the thigh muscles, which are needed to get up from the seat

Starting position
upright seat on a stool, Theraband in 8th loop around the feet and thighs, the ends are wrapped around the hands
Exercise execution
Stand up from the stool against the pull of the Theraband, at the same time straighten your upper body and open your forearms (external rotation of the shoulder
Strengthening of the hip-extending muscles


Starting position:
Quadruped, Theraband wrapped around the foot of the affected leg and held in place by hand
Exercise execution:
Stretch your leg back against the resistance of the Theraband at hip height, the pelvis should not move upwards towards the ceiling.
Hip osteoarthritis: exercises for the problem area of balance
Even without suffering from osteoarthritis of the hip, the ability to balance deteriorates from the 4th decade if there is no training stimulus.
In addition to strength and mobility, the degenerative hip osteoarthritis also affects coordination (optimal interaction of the muscles involved in joint guidance) and balance regulation, the movement sequence when walking and the feeling of movement are changed. The adaptation reaction of the muscles to a spontaneous shift in the center of gravity, falls, fears and rest worsen.
Intensive balance training / proprioception training (feelers in muscles, capsules, ligaments for neuromuscular control), in particular the deep muscles close to the joints in the hip joint and lumbar spine, complete the strength and functional training in hip osteoarthritis.
Information about balance regulation and exercise examples for balance training and fall prevention can be found at Fall in old age.
Hip osteoarthritis: problem area handicap in everyday life and when walking
- Restriction in everyday work and at home or in leisure activities
- Problems coping with longer walking distances
- Difficulty bending down, kneeling, climbing stairs, body care, especially foot care, getting dressed
- Changes in gait pattern: increased track width
- "Hollow back" due to the restricted hip extension
- Incline of the pelvis and chest to the side of the standing leg (the leg that is on the floor), creating a so-called limp
- Lowering of the pelvis on the free leg side (the leg that is in the air)
- Step shortening of the healthy leg due to the painful load phase on the affected leg
The physiotherapist analyzes the patient's gait and can use this to identify which goals can be achieved for the patient and which exercises are useful. In doing so, he must take into account the age of the patient, the individual structural functional impairment and personality structure. Depending on the degree of damage to the hip joint, a limping mechanism can be achieved by improving mobility, pain relief, muscle condition and coordination (optimal interaction of the muscles) can definitely be overcome again.
A patient can best accept irreversible walking difficulties if no false hopes are aroused and the patient is not overwhelmed with the exercises and demands.
The gait school includes exercises to train weight transfer while standing and walking, emphasizing hip extension when walking upright, climbing stairs and gait training with walking aids.
General recommendations for walking in everyday life:
- We recommend soft shoes, low heels, cushioned shoe soles, and Velcro fasteners if the hips are severely restricted
- Instructions for using everyday aids e.g. Shoe or stocking puller
- Do not use walking aids such as walking sticks, forearm crutches or walking carts too late, otherwise back pain will result from the asymmetrical gait
- Avoiding long hikes with unusual stress (e.g. climbing), long strolls through town, jogging
- Cope better with longer distances by bike
All therapeutic measures and exercises carried out so far create the prerequisites for improving the gait pattern.
This is an important motivational incentive for the patient to do the stretching and strengthening exercises as intensively as possible at home, in rehab or in the gym.
Hip osteoarthritis: Anxiety problem area
- Fear of pain and pain amplification
- Fear of movement and strain, resulting in rest with further functional impairment
- Fear of disability
- Fear of surgery
Information and advice for hip patients about the medical background and the course of the disease relieves fears and makes it easier to deal with existing complaints.
The aim is to find the right balance between load and resilience of the hip joint in everyday life and to learn the best possible compensation mechanisms for the handicap. Depending on the stage at which physiotherapy and sports therapy begins, joint replacement surgery (TEP) can be postponed a long way.
Information about any planned operation, the purpose of preparation and the subsequent rehabilitation alleviate understandable fears before the operation. With the knowledge of pain relief and rapid functional improvement after the operation through to the possibility of doing sports again, those affected can look forward to an operation with a confident attitude.
Examination of hip arthrosis
back to the main topic: Hip osteoarthritis