Bed-wetting in children (enuresis)
Synonyms in the broadest sense
Wetting, urinary incontinence
English: enuresis
definition
As bed-wetting (Enuresis) is the name given to the involuntary excretion of urine in children who are 5 years of age or older. age have completed. The wetting occurs several times in a month.
.jpg)
There are three different forms of enuresis (bed-wetting). If the wetting occurs only during the day, one speaks of one Diurnal enuresis. As Nocturnal enuresis is called the nocturnal wetting. The combination of both types is called Nocturnal and diurnal enuresis. Furthermore, a distinction is made between primary and secondary enuresis. In the primary form, the child was never dry; in the secondary form, the child has arbitrarily controlled its urine output for at least six months. The distinction between the various forms ultimately plays hardly any role in therapy, but primarily serves the purpose of diagnosis.
Often, organic causes, such as an open back (spina bifida) or malformations of the urethra, are responsible for wetting. In addition, mental problems are known to be the trigger, especially for secondary wetting. Due to the diverse causes and the high level of suffering for the child, especially in social interaction, a doctor should be consulted for clarification. Various options are available for treatment, whereby wetting can usually be successfully treated through behavioral therapy and counseling.
Wetting at the age of 6
Each individual child takes a different amount of time before the maturation of bladder control in the brain is fully completed. The main cause of nocturnal wetting is that the connection between a full bladder and the child waking up is not yet firmly established is. The children are therefore not too comfortable to get up at night, but simply do not notice the urge to urinate. Therefore, with some children it takes a little longer until the nights and days are dry. Up to the age of 5, the nocturnal wetting is to be regarded as a delayed development.
One speaks of bedwetting only from the age of 6 and should then initiate a detailed diagnosis to find out the possible cause. In addition to a organic voiding disorder can also psychosocial factors play a significant role. With age-appropriate development, the cause can also be in a Disruption of the hormonal regulation of the water balance lie. A hormone called ADH regulates the water balance and causes the bladder to fill up less at night and therefore less need to go to the toilet at night. In some children, this hormonal regulatory cycle is not yet fully developed and therefore promotes wetting at night.
Bed-wetting usually only becomes a problem when it is extremely stressful for the child and their family. Older children in particular withdraw a great deal from their social life and limit themselves in their everyday life due to fear or shame, because they fear being discovered during school trips or overnight stays with classmates.
frequency
The illness Bedwetting occurs differently depending on the age of the child. So suffer about 30% of five year olds from involuntary wetting. Up to this age, the disease occurs equally in boys and girls. With increasing age, boys are affected significantly more often than girls.
Overall, there are 5 out of 100 children among ten-year-olds who wet themselves, and the incidence of the disease is 2% in adolescents between twelve and fourteen years of age. Overall that is secondary enuresis, i.e. wetting with urine control previously achieved, the rarer form.
root cause
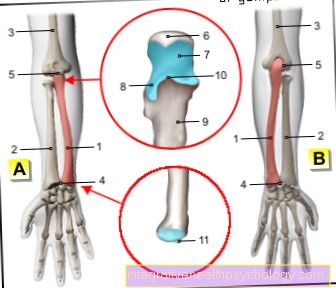
First of all, it should be noted that voluntary urination is an important step in the development of the child. However, this is associated with a very complex learning process, in which both the filling of the bladder and the voluntary opening and closing of the bladder muscle must optimally mesh and interact with one another.The beginning of this development begins around the age of 2 years. However, every child has a different speed until it is finally completely dry and the learning process is completed. For this reason, the problem usually solves itself. If this has not happened by the child's fifth year of life, the causes of the wetting should be found out.
There are two big pillars to explain the causes of bed wetting. On the one hand there are biological and physically conditioned causes, which usually result in primary enuresis. This includes one genetic predispositionwhich is present in about two thirds of all affected children. Some children have impaired regulation of the hormone Vasopressin, which is required for controlling the water balance. In these children, the hormone is not released in a certain rhythm as usual, so that they do not have a less full bladder at night than during the day, as intended.
But malformations and anatomical variants of the urinary tract, such as a defective nerve supply to the bladder muscles, also belong to this group and can cause bedwetting. Increased urinary tract infections are also a risk factor for the development. Children who are delayed in their overall development or who have not yet matured physically can also show enuresis.
Also to be considered is that psychosocial as well as the psychological Page.
Mental causes
In addition to organic causes or disorders in the child's maturation process, psychosocial factors can also play an important role in the occurrence of nocturnal wetting. Children can heavily burdened by external factors in their everyday environment and build up a great deal of insecurity and lack of self-esteem. Above all, drastic experiences like a family death, the Separation of parents or the birth of a new sibling can represent an acute stressful situation and act as a trigger for bed-wetting at night, even though the child was previously dry.
The other is behind the ability to control the bladder complex learning process. This can be slowed down or misdirected by various measures, such as inconsistency or severity, or in the case of intellectually impaired children and lead to the development of the disease. Especially in children with secondary enuresis, one often finds an emotional cause of the complaints.
Additional risks are concomitant illnesses such as disturbances in the child's social behavior or a known attention deficit or hyperactivity disorder. In addition to wetting, it can also lead to additional feces in some cases. If psychological causes come into question, a visit to a child and youth psychiatrist can be helpful in order to work out the cause, but at the same time to strengthen and relieve the child and to involve the parents in the healing process.
Symptoms
For a full diagnosis it is important to know what time of day, how often and with what intensity the wetting occurs. If the criteria just mentioned vary greatly from day to day, the present enuresis rather speaks against an anatomical malformation or inadequate nerve supply. If there is a functional disorder behind the wetting process, some of the children show behaviors that are supposed to help contain the urine, such as pressing their thighs together or jumping from one leg to the other. It can also be observed whether small amounts of urine can be found in the underpants just after tensing the stomach, for example when coughing or sneezing. Sometimes the wetting occurs at the same time as an involuntary rectal inspection (Encopresis) on.
Some of the children show a low self-esteem and exclude themselves from social activities because they are ashamed of being discovered or are afraid of the reactions. This disease poses a problem for children, especially on excursions or visits to friends, and increases their level of suffering.
diagnosis
About the disease Bed-wetting in children To be able to determine the doctor must first detailed survey carry out. Attention is also drawn to the family history. How was the cleanliness of the parents or siblings? Questions are also asked about the child's current situation, so if necessary mental stress to recognize. In addition, options are being clarified that might maintain wetting, such as wearing diapers and methods of toilet training that have been used so far. In addition, physical exams are available, also with the help of Ultrasonic and urine tests in the laboratory, on. The bladder measured, possible residual urine accumulation recorded in this and the composition of the urine assessed. In addition, it will be clarified whether there is a urinary tract infection. Psychological tests can also be part of the examination. In order to capture all of these points, it may be necessary for the child to be admitted to the hospital.
therapy
In general, good spontaneous healing is observed in enuresis. In addition, small measures that are discussed during a consultation with the doctor often lead to success. This includes the omission of threats and punishments in the event of renewed wetting and rewards for a “dry” day or a “dry” night. The child should drink a lot in the morning and reduce the amount of fluid in the evening. The family can be relieved with mattress protectors or washable duvet covers. You can also consciously wake the child up at night and put them on the toilet so that they can prevent them from getting wet. However, the disease can become chronic and lead to other problems, including social ones, so treatment is necessary.
Due to the different causes of wetting, the therapy must be tailored to the individual patient. The therapy options can be roughly divided into three groups.
On the one hand, drugs are available. Be there Imipramide antidepressants used to relax the bladder muscle. Since more damage to the heart muscle was observed here, this drug is increasingly being abandoned. The synthetically produced hormone desmopressin, which promotes water absorption (Reabsorption) in the kidney and can be taken as a tablet or nasal spray. There is also a muscle relaxing (spasmolytic) and local pain reliever drug that contains oxybutinin as an active ingredient. All drugs are only used for behavior therapy that is not possible and are by no means the sole treatment regimen.
Furthermore, behavioral therapies are used as treatment methods. The focus is on an alarm clock, a pair of bell pants as an alarm system.
There are also behavioral therapies that work with rewards every dry night or day, or precautionary awakening at night. Overall, almost all of the above-mentioned behavioral therapies require a high degree of motivation on the part of the caregivers, but also on the part of the children, and are the basis for a successful therapy.
Read more on the topic: Behavior therapy
The third therapy option is bladder training. The aim is for the child to fully develop their bladder control through practice. Interrupting urination (micturition) the child learns to arbitrarily influence his urine output.
Often the therapy options mentioned above are combined and used together, which also brings the best chances of success.
alarm
This is the first choice therapy for bedwetting at night, without any organic causes Alarm system in the form of bell pants or bell mats. These systems come with a sensor fitted, that reacts to moisture. With modern bell pants, this sensor is attached to the pants in the genital area. If it comes into contact with moisture, a circuit and a bell that is attached to the top of the pajamas closes, Makes a sound designed to wake the child so they can make their way to the bathroom and completely empty the bladder.
This alarm system is also available in the form of so-called bell mats. The moisture sensor is located here in the mattress. With this system, the bell is on the bedside table and is louder than the bell on the bell pants. This is particularly advantageous when it is difficult to wake up which is the cause of the nocturnal wetting. These alarm systems will always be combined with a toilet diary, in which it is recorded how often the child wets, when it remained dry and how large the amount of urine deposited was during the subsequent visit to the toilet.
If the child has been continuously dry for 2 weeks, the bell device can be stowed away in most cases. About 60-70% are completely dry after treatment with one of these alarm systems at the end of the therapy period.
Diapers
Nowadays the retail trade offers a wide variety of diapers in the form of pants, pajamas or boxer shorts for bedwetters of all ages. They look like normal underwear, but have the function of a diaper by adding them absorbent are and catch the moisture. They come in different colors, sizes and shapes and are made from a fabric that doesn't rustle or crackle. These diapers can be put on by the children themselves and can be disposed of immediately after a single use. Wearing diaper panties at night can make the situation easier for many children because they do not have to wake up in a wet bed in the morning and develop a sense of security. Straight older children find this particularly humiliating, shameful and frustrating.
They also offer an alternative for children who want to spend a night outside of their home environment, but are very afraid of rewetting. Still, wearing such diapers should be just a short term solution be because of it the causal problem for the nocturnal wetting did not resolve can be. In addition, one should never force the diaper on the child or use it as a punishment, as this has a very degrading effect on the children.
homeopathy
In addition to conventional medical treatment options, homeopathic remedies are also used in the therapeutic treatment of bedwetting in children today. When choosing the right remedy, the main thing to consider is whether the affected child has never been permanently dry up to this point or whether it is a psychologically-related relapse. The duration of treatment should be several weeks, as only then can the first successes become apparent. The funds are administered in the form of globules in the evening.
Equisetum, Sepia officinalis or Pulsatilla pratensis can be used for children who have not been dry before. These are medicinal herbs that are mainly used by small, petite and insecure children.
If there is a relapse as part of psychological stress, Belladonna or Causticum is used in most cases. Overall, when using homeopathic remedies, contact should always be sought with a therapist with additional homeopathic training, as the treatment must be very individually tailored to the child.
Schüssler salts
Schüssler salts can also find their use in bed-wetting therapy for children. The Schüssler salts Potassium bromatum No. 14 and Potassium aluminum sulfuricum # 20 above all in states of restlessness and nervousness used. Children can take one tablet for each salt before going to bed. They are designed to reduce stress and tension and thereby prevent bedwetting.
forecast
In general, the healing prognosis for enuresis is good. Behavioral therapy can achieve success in 80% of children.