Facet syndrome
What is facet syndrome?
The facet syndrome is one of the degenerative (wear-related) diseases of the spine and describes a complex of various symptoms (syndrome) with advanced wear of the small vertebral joints (spondylarthrosis).
Also read our related article: Spinal osteoarthritis - this is how it is treated

The spondylarthrosis itself can either appear as an independent, leading clinical picture, then one speaks of a facet syndrome, or in turn be the cause of other clinical pictures (e.g. spinal canal stenosis, root compression syndrome)
Facet syndrome mainly affects people over the age of 50. The clinical picture occurs predominantly in the area of the lower lumbar spine (LWS), but can also affect the vertebral joints (facets) of the cervical spine (Cervical spine), least of all those of the thoracic spine (thoracic spine).
Local back pain that increases with exertion and improvement at rest are the leading symptoms.
A disc damage, as it occurs after a herniated disc, can be the cause of the facet syndrome.
Symptoms of facet syndrome
The main symptom of facet syndrome is pain along the spine. As a result of long-term wear and tear on the vertebral joints, facet syndrome can occur in all areas of the spine, but it is most commonly found on the lumbar spine.
The pain is caused by inflammation at the facet joint and can therefore be provoked and intensified locally by pressure. In addition, the pain often radiates. The progression depends on the height of the original joint. If the vertebrae of the lumbar spine are affected, the radiation into the leg is typical. In the thoracic spine, the transmission can be felt more on the upper body. If the cervical spine is affected, the pain can spread to the arms, hands and fingers. This is a so-called pseudoradicular Pain. “Radix” refers to the nerve root that arises at the affected joint. The pain spreads along the course of the nerve cords, but without causing the typical irritation to the nerve root. In the case of facet syndrome, this usually prevents tingling and numbness and the range of the pain is also less.
Read more on this topic in the main article: Symptoms of facet syndrome
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Facet Syndrome pain
The joint surfaces and joint capsules are also affected by the wear and tear of the joint. This can cause synovial fluid to escape and the joint capsule can become inflamed, which causes severe pain locally in the spine. This can be provoked by applying pressure above the affected vertebra. Depending on the course of the facet syndrome, the pain radiates along the nerve cords emanating from the affected vertebra. Pain often affects the legs in the lumbar spine, and especially the shoulders and arms in the cervical spine. The thoracic spine is rarely affected, but it can cause pain along the ribs.
You can find a lot more information under our topic: Facet joint pain
What is an activated facet syndrome?
An activated facet syndrome is an acute inflammation in the area of the small vertebral body joints (facet joints) on the basis of an existing facet syndrome, which leads to an acute occurrence of pain. An activated facet syndrome is thus a facet irritation. This can also be referred to as facet arthritis or activated facet arthrosis.
Localization of a facet syndrome
Lumbar spine facet syndrome (lumbar spine)
An enormous number of adults in Germany suffer from chronic back pain. The generic term "lumbar spine syndrome" summarizes a number of diseases that cause such pain.
Facet syndrome is a common underlying disease that causes lumbar spine syndrome. Several factors are to blame for the wear and tear on the facet joints. Nowadays, most of the people do long sedentary jobs. The back muscles, which significantly stabilize the spine, are too weak in the majority of adults. There are also harmful, incorrect movements, for example when lifting. Heavy lifting from the back puts enormous strain on the spine and especially the intervertebral discs.
Read more on this topic: Facet syndrome of the lumbar spine
The lumbar spine is particularly often affected, as large parts of the body weight bear on it. For this reason, obesity is an additional risk factor. In addition, the lumbar spine has a significantly higher mobility than the thoracic spine, which is severely restricted in its possibilities by the ribs.
In the facet syndrome of the lumbar spine, the origin of the wear is often in the intervertebral discs. Due to their loss of height, the intervertebral joints are closer to each other, which leads to greater wear and tear with every movement. In addition, the joint surfaces and joint capsules can become inflamed and lead to considerable pain. In the area of the lumbar spine, various nerves emerge from the spinal cord, which supply the legs, feet and groin region in a sensitive and motorized manner. In the case of a facet syndrome, the pain can progress in the area of these nerve cords.
Please also read: Signs of a herniated disc
Facet Syndrome of the Cervical Spine (Cervical Spine)
The cervical spine is affected by a facet syndrome much less often than the lumbar spine, but more often than the thoracic spine. This is because the cervical spine, as a very flexible, moving part of the spine, takes on many everyday tasks, but is exposed to less pressure and weight than the lumbar spine.
Read more on this topic: Facet syndrome of the cervical spine
When the painful facet syndrome occurs, however, the symptoms are all the more bothersome in everyday life. In addition to permanent neck pain, the back of the head, shoulders and shoulder blades are also noticeable. If the pain is passed on, the pain can radiate into the fingers. An upright posture and strong neck muscles are important factors in preventing facet syndrome of the cervical spine.
For mild pain, even warmth, for example by wearing a scarf, can provide relief. Treatment of facet syndrome on the cervical spine should generally be handled with care, as many vital structures are located on the neck in a small space. Manual interventions and vigorous exercises can even be life-threatening if the cervical spine is damaged
Please also read: Treatment of cervical spine syndrome
Facet syndrome of the thoracic spine (BWS)
The thoracic spine is rarely affected by facet syndrome. The rigid chest with the ribs largely restricts the mobility of the thoracic spine. Even when lifting heavy loads, only the lumbar spine is mostly affected.
The facet syndrome on the thoracic spine is particularly noticeable through pressure loads on the upper back. For example, this pain can be noticed for the first time when lying down. The pain can also be provoked by tensing the chest muscles or contracting the shoulder blades. In rare cases, the pain can spread down the ribs to the sternum. If the facet syndrome is at the transition to the cervical spine, shoulders and arms can also be affected.
Please also read: Thoracic spine pain
How does a facet syndrome of the cervical spine differ from that of the lumbar spine?
Facet syndrome occurs in the lumbar spine (LWS) much more frequently in the thoracic spine (thoracic spine). It occurs on both the cervical and thoracic spine as a result of increasing wear and tear on the small vertebral body joints (facet joints). This wear and tear is known as osteoarthritis.
Neck pain that can radiate towards the head, shoulders or arms is characteristic of facet syndrome of the cervical spine. The pain can depend on the posture and often increases during the day. If necessary, the mobility of the head is also restricted.
Read more on the subject at: Facet syndrome of the cervical spine
A facet syndrome in the lumbar spine is characterized by pain in the area of the lower back, which can radiate into the buttocks and legs. Often the pain also increases in the course of the day due to physical strain.
Read more on the subject at: Facet syndrome of the lumbar spine
Is there also a facet syndrome of the thoracic spine?
Facet syndrome in the thoracic spine (thoracic spine) area is very rare. It occurs less often here because the thoracic spine is severely restricted in its mobility by the ribs and the thorax and the wear and tear on the small vertebral joints (arthrosis) is less than in the area of the cervical or lumbar spine. If facet syndrome occurs in the chest area, those affected often feel pain at chest level. This pain can increase when you are lying down.
Where is facet syndrome most common?
Most often, a facet syndrome occurs at the transition from the lumbar spine to the sacral part (L5 / S1). This is due to the heavy physical strain in this area due to body weight and physical strain from lifting and carrying heavy objects. Of course, facet syndrome can also have other causes.
Causes of Facet Syndrome
Facet syndrome is an acquired disease of old age.
The causes of their formation include:
- Overwork in work and sport
- Disc degeneration / disc wear
- disc prolapse
- Spinal instabilities
- Spinal deformations (side curvatures: scoliosis; hyperlordosis: hollow back)
- rheumatism
- Obesity / muscle weakness
Read more on this topic in the main article: Causes of Facet Syndrome
In the context of intervertebral disc degeneration / intervertebral disc wear, the height and instability of the spinal column are reduced, with incorrect and overloading of the vertebral joints.
Heavy physical work (a lot of lifting and bending) promotes the occurrence of a facet syndrome of the lumbar spine due to increased wear and tear. Overhead work, such as painting, can lead to a facet syndrome of the cervical spine due to the increased stress on the vertebral joints when reclining (looking up, bending back).
Instabilities and curvatures of the vertebral joints lead to increased cartilage wear due to abnormally increased joint mobility or an incorrect load caused by the curvature.
Rheumatic diseases can also affect the spine and lead to premature spinal joint wear.
Reasons why vertebral joint pain can occur:
- Typical osteoarthritis pain (facet syndrome)
- Inflammatory pain (rheumatism, rheumatoid arthritis)
- Mucous membrane entrapment (acute back pain)
- Dysfunctional pain ("blockages") (acute back pain)
Read more on the topic: Lumbar spine syndrome causes
How is facet syndrome diagnosed?
In order to be able to make the diagnosis of a facet syndrome, the pain and accompanying symptoms must first be asked in a detailed anamnesis. The most important thing is the location of the pain in the spine. Depending on whether the pain is localized in the cervical, thoracic or lumbar spine, other symptoms can be typical. Often there is a so-called pseudoradicular Pain symptoms. The pain spreads and radiates into surrounding areas of the body. The location of these symptoms in turn allows conclusions to be drawn about their origin in the spine.
There are a few physical tests that can help diagnose facet syndrome. Typical is, for example, pain over the vertebrae, which can be triggered by targeted pressure from the outside. The symptoms of exercise can also be determined through a physical examination. Pain points and mobility are checked while the patient flexes and extends the spine.
Only when the symptoms are still unclear and indistinguishable from back pain of any other kind can diagnostic imaging be used. Since facet syndrome is a symptom of wear and tear, detailed images must be used, for example CT or MRI. A pure x-ray is often not enough to show the joints.
A so-called “facet injection” can also be used as a diagnostic tool. For this purpose, the suspected joint is sensitized with saline solution or anesthetized with an anesthetic in order to be able to confirm pain symptoms.
The facet syndrome must be differentiated in the diagnosis of herniated discs, vertebral fractures, spinal canal stenosis and various pain syndromes on the back in order to be able to initiate the correct therapy.
Read more on this topic in the main article: Diagnosis of facet syndrome
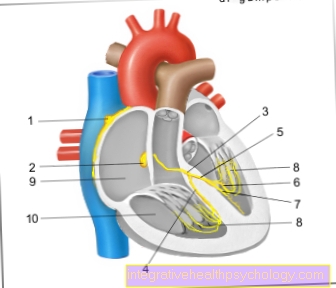
Computed tomography for facet syndrome

- Intervertebral disc
- Spondylarthrosis (osteoarthritis of the small vertebral joints)
- Spinal cord
- Narrowing of the nerve canal due to bony attachments (osteophytes) on the joint (due to wear and tear = arthrosis)
- Narrowing of the nerve canal
- Vertebral joint with osteoarthritis
- Spinous process
How is facet syndrome treated?
Therapy of facet syndrome of the lumbar spine
As a frequently affected area, the lumbar spine is an important trigger of the lumbar spine syndrome, which affects many people. It is a common factor in occupational disability and affects physically hard working people in particular, as well as those who sit for long periods of time. The therapy is extremely important to maintain the quality of life.
Read more on this topic in the main article: Therapy of facet syndrome
In the case of signs of wear and tear such as facet syndrome, many of the joint structures are often already damaged at the time of diagnosis. The goal of therapy is to stop the progression of the disease, relieve stress on the nerves, maintain movement in the spine, and reduce pain and symptoms. In most cases, a combination of symptomatic pain therapy and causal physiotherapy and exercise therapy is carried out for this purpose.
For mild pain, pain medication from the NSAID group is first prescribed. The most important representatives are ibuprofen and diclofenac. For pain that is more tolerable, opiates can be used, for example, in the form of a pain plaster.Newer methods of pain therapy also include heat therapy, ultrasound treatments, or electricity therapy.
A disciplined movement therapy is essential for the causal therapy of the facet syndrome of the lumbar spine. To do this, the back muscles must be strengthened intensively. Various exercises to maintain mobility in the joint can also be performed under the guidance of a physiotherapist.
Symptomatic long-term therapy options can be considered for treatment-resistant pain. For this purpose, the sensitive nerves at the affected joint can be treated using anesthetics and coagulation therapies. The latter therapy involves heat sclerotherapy of the nerves. The aim is to destroy the sensitive nerves in order to suppress the pain in the long term.
Read more about the topic here: Heat therapy.
Therapy of facet syndrome of the cervical spine
Facet syndrome is much less common in the cervical spine than in the lumbar vertebrae. However, due to the many possibilities of movement in the neck, pain is a much greater limitation in everyday life. The pain sometimes extends from the neck to the head. In order to stop the progression of the disease and maintain mobility in the neck, careful exercise therapy with symptomatic pain treatment is also important in the cervical spine. Exercise therapy on the cervical spine must be carried out carefully, as the joint and muscle structures here are significantly more sensitive than in the lumbar spine and there are many structures that are essential for survival in the cervical spine.
Pain therapy consists of several stages, depending on the severity of the pain and resistance to the treatment. Medications such as ibuprofen and diclofenac are prescribed initially. Natural remedies can also be used for mild complaints. Opiates can be used if the symptoms are unbearable. Ultrasound and heat therapies can also be used for facet syndrome of the cervical spine.
For causal therapy, it is also important to determine the trigger of the pain syndrome. This can be an incorrect, stooped posture, but also stress in sports and everyday life. In addition, the muscles must be strengthened and posture optimized. Special back schools can carry out appropriate therapies and instruct exercises for the neck.
Can a hyaluronic acid injection help?
A hyaluronic acid syringe can support the regeneration of the articular cartilage of the small vertebral joints (facet joints). This is hoped for a long-term reduction in pain.
Read more on the subject at: Hyaluronic acid used to treat joint diseases
How well does nerve obliteration in the facet joint help?
In the case of nerve sclerotherapy, the pain-causing nerves in the area of the small vertebral body joints (facet joints) are switched off, for example in a small operation, using heat or cold. This will ease the pain. Often an infiltration with a local anesthetic (local anesthetic) is carried out beforehand to check whether the pain subsides.
Exercises for facet syndrome
In the back school and physiotherapy, certain exercises can be learned for the treatment of the facet syndrome. The main purpose of these is that Spine stability to promote and the Muscle strength in the back too strengthen.
The Back school In addition to strength training for the long extensor muscles of the spine, it also includes exercises for the self-awareness of the body, promoting one's own daily activity, Posture training and Measures to cope with pain.
What is the prognosis?
How long does facet syndrome last?
Since facet syndrome cannot be cured, it will last a lifetime. However, that doesn't mean you have to suffer from pain for a lifetime. In addition to drug therapy, there are now various surgical therapies that reduce pain in the long term.
What are the chances of recovery?
There is no cure for facet syndrome. The pain that occurs with facet syndrome is caused by osteoarthritis of the small vertebral joints. This means that the cartilage wears out due to physical stress. Since the cartilage cannot regenerate, the osteoarthritis and with it the facet syndrome persist.
Long-term pain relief can be expected through drug therapy and physiotherapy. There is also the possibility of various surgical techniques to reduce pain in the long term.
How long are you on sick leave?
How long you are on sick leave or how long you are unable to work cannot be said in general terms. The decisive factors are the severity of the pain, how well a treatment works and what job you do. It is important to reduce the physical strain and to wait until the inflammation in the area of the facet joint has subsided before returning to working life.
Can you do sports if you have facet syndrome?
Exercise can be both a cause and a therapy for facet syndrome. First of all, many sports can strain the spine through vigorous, jerky movements and trigger the facet syndrome. Sports such as basketball put increased stress on the intervertebral discs and, as a result, on the facet joints.
Weight training and sports such as cycling and swimming can, however, have a positive effect on the course of the facet syndrome. All sports that are gentle on the intervertebral discs and joints, but require a high level of muscle activity and stability in the back, are preferable in facet syndrome. Which sports should be avoided in particular with facet syndrome and which can be practiced without hesitation should be clarified with the orthopedic surgeon or physiotherapist.
Spine anatomy
The lumbar spine (lumbar spine) is made up of the five lumbar vertebrae of the spine. Since they are located in the lower part of the spine, they have to carry the highest percentage of weight. For this reason they are also much thicker than the other vertebrae. However, this does not avoid the signs of wear and tear that occur very frequently, particularly in this area. For example, joint wear and herniated discs in the lumbar spine are the most common.
Each vertebral body has two upper and two lower vertebral joints. These create the connection to the next upper or lower vertebral body, which in turn has the same articular processes. Depending on the alignment of the vertebral joints and the structure of the vertebral bodies, different degrees of movement are possible for the relevant spinal column section.
The overall mobility of the spine is great, although only relatively small movements are possible between the individual vertebral bodies. By adding up these small freedom of movement, the result is the large range of motion.
The cervical spine (Cervical spine) and especially the lower cervical vertebrae have the greatest range of motion due to the almost horizontal alignment of the small vertebral joints. Movements in all directions are possible.
The range of motion of the thoracic spine (BWS) is small due to the special structure of the vertebral body and the attachment of the ribs. The main movement of the thoracic spine occurs when the torso is rotated in the lower thoracic spine region.
In the lumbar spine, mainly bending and straightening movements and sideways movements are possible. Due to the special structure of the vertebral body and the vertebral joint alignment (front / back), there is hardly any rotational movement.
How does facet syndrome develop?
The development of facet syndrome should be seen in connection with other degenerative diseases of the spine.
The wear and tear of the intervertebral discs begins as early as the 20s of a person. It can lead to a bulging disc or a herniated disc (Nucleus pulposus prolapse) come. The increasing loss of water from the intervertebral disc leads to a decrease in height of the intervertebral body section (Osteochondrosis). The consequences are an overload of the small vertebral joints, a malfunction of the spinal ligaments and a creeping instability of the so-called spinal column movement segment (each consisting of two vertebral bodies and the intervertebral disc).
The base and cover plates of the vertebral bodies are more stressed by the lowered intervertebral disc. The body reacts to this with bone compression in the area of these structures (Sclerotherapy), which can be seen radiologically.
The body tries to counteract the instability of the spine by adding bony attachments to the vertebral bodies (Osteophytes/Exophytes) that are looking for something to hold on to in their surroundings.
If the instability is very advanced, the spine can become warped due to wear and tear, which further weakens the statics of the spine (degenerative scoliosis).
In the further course of the facet syndrome, the statics of the spine changes. The points of origin and attachment of the muscles and ligaments of the spine change, with some muscles and ligaments getting too close and shortened and others being stretched too much. Both of these lead to the weakening of these structures through the loss of function. Painful muscle hardening (Muscle tension /Myogelosis) can train.
An incongruent (not congruent) position of the vertebral body joints to one another leads to premature cartilage wear of the joint partners. The same processes then take place that are well known for knee or hip arthrosis. With facet syndrome there is joint inflammation, capsule swelling and thickening, and joint deformity even more quickly than with large joints. The overall picture of a vertebral joint osteoarthritis (ppondylarthrosis) was created.
Displacements of the vertebral bodies caused by instability (Pseudospondylolisthesis), Thickening of the vertebral joint structures, bony spinal canal attachments, intervertebral disc protrusions and thickening of the vertebral ligaments (Ligamentum flavum) can eventually lead to considerable narrowing of the spinal canal (Spinal canal stenosis) and press the spinal cord itself or the nerve roots that come off. A pressure on the nerve root in the nerve root is called recess stenosis Lateral recess (lateral area of the vertebral canal), mostly due to degenerative changes in the upper vertebral joint process in facet syndrome (Superior articular process) caused.