Blood count
introduction
The blood count is a simple and usually inexpensive examination method used by the doctor, with which certain markers and parameters in the blood serum can be measured and determined in a laboratory using a blood sample from the patient's venous blood.
Read more on this topic at: Blood collection
The evaluation of the blood sample is now largely carried out automatically by a special device in the laboratories, so-called Hematology devices, blood smears are only examined under the microscope by the laboratory staff themselves for certain questions. In addition to the assessment of the blood cells, the solid blood components and the blood pigment, numerous organ-specific parameters (e.g. Liver values, kidney values, electrolytes, thyroid values, etc.) can be determined from the blood serum. These organ values are not determined in the actual blood count, but from the blood that is taken in a separate tube.

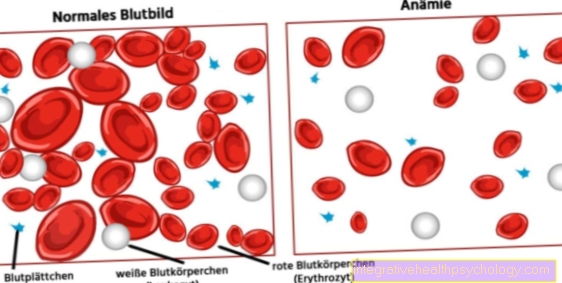
One generally differentiates between the acceptance of a small and one large blood count. The small blood count represents the Basic diagnostics in the blood test, in which only the number of redden and white blood cells (Erythrocytes, leukocytes), of the Platelets (Platelets), of the Blood pigment content (hemoglobin) and the Ratio of solid to liquid blood components (Hematocrit) is determined.
The complete blood count, on the other hand, is an extension: the small blood count is called the Differential blood count combined, in which the subclasses of white blood cells are determined individually and separately in their existing number.
Furthermore, numerous other parameters can be determined, which, however, are not included in the categories "small"Or"great"Blood counts fit, but are either determined in addition or, depending on the issue, are organ-specific, pioneering (Liver and kidney values etc.)
Both the large and the small blood count are made from what is known as EDTA blood Determined: The patient's blood to be examined is taken using an EDTA tube, which contains a substance that prevents the blood from clotting and thus also outside the body for the laboratory capable of investigation holds.
The small blood count
The small blood count is the basic form of the blood count. The parameters that are determined in a small blood count by the laboratory include the number of red blood cells (Erythrocyte count), the number of white blood cells (White blood cell count), the number of Platelets (Platelet count), the Concentration of the red blood pigment in blood (Hemoglobin concentration), the Amount of solid blood components or that Ratio of solid to liquid blood components (Hematocrit) and the so-called Erythrocyte indices MCH (mean corpuscular hemoglobin amount of a single erythrocyte), MCV (mean corpuscular volume of a single erythrocyte) and MCHC (mean corpuscular hemoglobin concentration of all erythrocytes).
The big blood count

A complete blood count is the combination of a small blood count (Hb, number of erythrocytes, leukocytes and platelets, MCH, MCHC, MVC) and a differential blood count (A.breakdown of the individual white blood cells). The complete blood count examines the subgroups of white blood cells more closely. Changes in their division allow indications of different diseases, since each subgroup has its own special task. In percent, the breakdown would look like this:
- 60% neutrophil granulocytes (= Granulocytes with rod and segment nuclei)
- 30% lymphocytes
- 6% monocytes
- 3% eosinophils
- 1% basophil granulocytes
The granulocytes represent the main part of the white blood cells, followed by the lymphocytes and monocytes.
The reason for having a complete blood count are suspected diagnoses, such as Blood system disorders, severe systemic diseases, infections, parasite infestation (e.g. Malaria etc.) or congenital red blood cell disorders (e.g. Sickle cell disease).
Important values
Erythrocytes

Erythrocytes are red blood cells whose main job is to carry oxygen in the blood. To do this, oxygen is bound to the protein hemoglobin, which is present inside the erythrocytes. The normal values for erythrocytes in a healthy adult man are between 4.3 and 5.9 million / µL blood; in a healthy adult woman between 3.5 and 5.0 million / µL.
The formation of erythrocytes occurs in the bone marrow and ends in the liver and spleen. The normal survival time for red blood cells is around 120 days. Pathological changes in erythrocytes can affect their number, shape, size and function and can be detected with the help of a blood count. If the number of erythrocytes is low, anemia is usually present. Anemia can be caused by acute or chronic bleeding, kidney disease (renal anemia) or an iron or vitamin B-12 and folic acid deficiency. Leukemia or other types of cancer can also be associated with decreased erythrocyte counts.
If erythrocytes die prematurely, this is called haemolytic anemia. The causes for this can be congenital erythrocyte defects, infections or heavy metal poisoning.
Increased erythrocyte values, on the other hand, are usually due to a lack of oxygen, which can be caused, for example, by diseases of the lungs or heart or by staying at high altitude. Bone marrow diseases such as Polycythemia vera can be associated with increased erythrocyte counts.
Erythrocytes that are too small are called microcytes. These usually occur with an iron deficiency. Erythrocytes that are too large (also called macrocytes) are usually the result of alcohol consumption or a vitamin B-12 and folic acid deficiency. Shape-altered erythrocytes can occur in anemia, genetic defects (sickle cell anemia) or heart valve replacement. The result is usually an increased breakdown of the erythrocytes with the following anemia.
hemoglobin
hemoglobin is also known as red pigment of the erythrocytes designates and owns the task oxygen inside the red blood cells to tie. The Normal values for hemoglobin are in an adult man between 13 and 18; at Women between 11 and 16.
A decreased hemoglobin level lies by Anemia (Anemia), at Kidney disease or at inflammatory bowel diseaselike that Crohn's disease in front. One increased hemoglobin One finds with increased erythrocyte countse.g. when staying at high altitudes.
MCV
Of the MCV value is a blood value that can be determined by the doctor as part of a small blood count and determined by the laboratory. MCV is the abbreviation for the so-called "mean corpuscular volume"Of red blood cells (Erythrocytes) what that medium volume a single red blood cell is meant.
This value is usually calculated in the laboratory using the Refraction the erythrocytes through a specific device (Flow cytometry) or a simple Calculation formulawhere the value of the cellular blood percentage (Hematocrit) divided by the total number of red blood cells in the blood.
The normal range for the MCV value is roughly between 83 and 97 fl (Femtoliter).
It applies in the (Blood-) Diagnostics as one of the important markers for various (Blood-) Diseases, especially for those Anemia (anemia).
As a rule, the MCV value is determined together with the MCH and MCHC value and then enables an important subdivision of an existing anemia. If the MCV value is reduced, this is often an indication that the red blood cells are too small (microcytic), if it is too high, the volume of the erythrocytes is too large (macrocytic).
MCH
Like the MCV value, the MCH value is a blood value that can be determined by the laboratory as part of a small blood count.
MCH stands for the "mean corpuscular hemoglobin content“Than the red one Dye contentevery single red blood cell (Erythrocyte) having.
This value is usually calculated automatically in the laboratory by a specific device (Flow cytometry) based on the Refraction Measure the amount of dye in the red blood cells in the erythrocytes.
The MCH value can, however, also be calculated by dividing the total hemoglobin value, which can also be determined in the blood count, by the total number of erythrocytes. The norm for the MCH value is between 28 and 33 pg (picogram).
Like the MCV and MCHC values, the MCH value is a diagnostic marker for diseases of the blood system, especially the Anemia (anemia). If the MCH value is low, this is an indication that the red blood cells too little red dye contain (hypochromic), if it is increased, they contain accordingly too much from that (hyperchrome).
MCHC
In addition to the MCV and MCH values, the MCHC value is another important diagnostic marker for diseases of the blood system - above all for Anemia (anemia) - which can be determined by the laboratory as part of a small blood count. The abbreviation MCHC stands for "mean corpuscular hemoglobin concentration“, So the Concentration of all the red dye (hemoglobin) of all erythrocytes in the blood of the respective patient.
This value can be calculated by dividing the total concentration of the red dye, which can also be determined by the laboratory, by the value of the solid blood components (hematocrit) in the blood. Another way of determining the MCHC value is to calculate it from the MCH and MCV values that may already be known (MCHC = MCH / MCV). The norm for the MCHC value is between 30 and 36 g / dl (grams per deciliter). Unlike the MCV and MCH values, the MCHC value often hardly changes because the MCH and MCV values usually move together in the same direction, i.e. they increase or decrease together and the quotient thus remains the same. That is why the MCHC value is generally only used by the assessing physician as a plausibility check.
Leukocytes
Leukocytes or "white blood cells" are certain cells in the blood whose main task is to ward off pathogens. The formation and maturation of leukocytes takes place in the bone marrow from a common precursor cell (stem cell). Incorrectly programmed or defective leukocytes are usually removed from the bone marrow; functioning, mature leukocytes are then released into the blood.In some cases, however, “incorrectly programmed leukocytes” may survive. These can then attack and destroy the body's own cells and tissue. The consequences are autoimmune diseases such as the well-known lupus erythematosus or multiple sclerosis. The determination of leukocytes is part of the routine blood tests. They are carried out if inflammation or infection is suspected, if leukemia is suspected, in the case of infarcts and poisoning, as well as radiation or immunosuppressive therapies.
The normal values for adults should be between 4-10,000 leukocytes / µL. Typical diseases that are associated with low leukocytes include Viral diseases, bacterial diseases such as typhoid, bone marrow diseases in which the formation of new leukocytes is prevented or an overactive spleen (hypersplenomegaly) in which leukocytes are broken down more quickly. The white blood cells are increased in inflammation (e.g. pneumonia), in many bacterial infections, in leukemia (blood cancer) or in very heavy nicotine consumption, this is also known as "isolated leukocytosis".

An increase in lymphocytes is mainly found in viral infections (mumps, measles), autoimmune diseases or leukemia. A decrease can occur in the context of various types of cancer or drug side effects.
Monocytes are mainly increased in tuberculosis. In the case of granulocytes, different subclasses of granulocytes are increased depending on the cause of the disease. Neutrophil granulocytes are increased, especially in bacterial infections. In severe infections such as sepsis, the so-called left shift often occurs. Here, due to the high need for cellular defense, precursors, i.e. immature granulocytes, are also released. This effect shows up in the full blood count as a left shift. Eosinophil granulocytes are mainly increased in the case of parasite infestation by worms or allergic reactions. Basophilic granulocytes are mainly increased in blood cancers such as chronic myeloid leukemia. If leukocytes, erythrocytes and thrombocytes are decreased, one speaks of pancytopenia (decrease in all cell rows). This is usually an indication of severe bone marrow damage. If two or more rows of cells are changed (e.g. increase in leukocytes and decrease in erythrocytes), this is usually an indication of leukemia.
Platelets
Are platelets small, disc-shaped plateletsthat in the body for the Blood clotting are responsible. This mainly plays at Cuts an important role. If there are too few or too many dysfunctional platelets in the body, bleeding cannot be adequately stopped. The result is that injuries bleed longer. The normal one Survival time of platelets 5-9 days. They are then broken down in the liver and spleen. Platelets are usually routinely determined in a blood count or especially determined when patients suddenly bleed more than usual, if Thrombosis occur or if one Heparin therapy should be monitored.
The Standard values for platelets in adults 150,000 to 400,000 per microliter. Causes of a Thrombocytopenia (too few platelets) can include Leukemias and myelodysplastic syndromes, Autoimmune diseases as the TTP or the Immune thrombocytopenia, chronic liver damage or a Hemolytic uremic syndrome (HUS) be. Cases where the number of platelets elevated are, are acute infections, Tumor diseases or myeloproliferative diseases, as the essential thrombocythemia.
CRP (C-reactive protein)
Behind the abbreviation CRP is the term "C-reactive protein“, Which stands for a protein in human plasma that is produced in the liver and then released into the blood.
It belongs to the so-called "Acute phase proteins“And is thus in the broader sense a Immune system proteinwhich in a "Acute phase“Sets the defense mechanisms in motion and subsequently attaches itself to bacteria, so that Complement system (Part of the immune system) and certain Immune cells (e.g. Macrophages) to be activated.
Under physiological or healthy circumstances, CRP is only present in very small amounts in the blood; the norm is an upper limit of 1mg / dl.
The CRP value is always increased when inflammatory processes occur in the body (e.g. infectious and non-infectious inflammations such as respiratory or urinary tract infections, appendicitis or gallbladder infections, etc.), although it is not possible to draw conclusions about a specific disease, so that more precise diagnostics are possible further investigations have to follow. In general, the CRP value increases with bacterial infections stronger than viral.
Normal values of the large blood count
In men
- Rod-like granulocytes: 150-400 / µL
- Segmented granulocytes: 3,000-5,800 / µL
- Eosinophil granulocytes: 50-250 / µL
- Basophil granulocytes: 15-50 / µL
- Lymphocytes: 1,500-3,000 / µL
In women
- Rod-like granulocytes: 150-400 / µL
- Segmented granulocytes: 3,000-5,800 / µL
- Eosinophil granulocytes: 15-50 / µL
- Basophils: 1500-3000 / µL
- Lymphocytes: 285-500 / µL
Cost of blood count
The cost of a blood count varies from case to case, depending on whether the patient is affected statutory or private health insurance heard and in which extent the blood test is carried out (small blood count, complete blood count, additional values such as Liver values, inflammation values, thyroid values, kidney values, eletrolytes etc..).
In general, the health insurance companies pay one Routine blood counts by the attending physician every two years, however, there is a plausible one medical need for more frequent blood withdrawals, these are also usually taken over by the health insurers.
Blood withdrawals without medical indication, purely at the request of the patient, however, often have to be paid for out of pocket. The costs for this are made up as follows according to the fee schedule for doctors (GOA): The blood sample itself costs 4.20 €, the symptom-related blood test costs 10.72 € and the medical consultation costs 10.72 (10 min conversation time) which can take place both before the blood sample is taken as an explanation, and after the blood sample is taken to discuss the results.
Liver values

„Liver values“Is a term for the measurable concentrations of certain enzymes in the blood serum, most of which are formed in the liver cells and can therefore be viewed as liver-specific parameters or markers.
They are usually determined as part of the diagnosis of liver and biliary tract diseases. In routine diagnostics, the concentration of four enzymes is determined: the gamma-glutamyl transferase (short: Gamma-GT / gGT), glutamate pyruvate transaminase (in short: GPT, also called alanine aminotransferase - in short: ALT or ALAT), glutamate oxaloacetate transaminase (in short: GOT, also called aspartate aminotransferase - in short: AST or ASAT) and alkaline phosphatase (in short: AP).
Please also read our page:
- Liver values
- increased liver values
- Bilirubin
Of the most liver specific The value is the GPT, the most sensitive liver and biliary tract marker is the gGT (GOT and GPT often only increase with severe damage to the liver cells) and strongest markers for biliary tract diseases such as A bile congestion from gallstones is the AP.
GPT (glutamate pyruvate transaminase)
GPT is one of the specific liver values, as it is mainly found in the cells of the liver, but it also occurs in small amounts in the cells of the skeletal and heart muscles, where its primary task is to participate in protein metabolism Cells or the respective organ.
If the GPT value in the patient's blood count is increased, this can usually be a sign that there may be a disease of the liver and / or biliary tract (e.g. Inflammation of the liver, fatty liver disease, drug / alcohol abuse, obstruction of the biliary tract due to gallstones, etc.).
The GPT is the enzyme that produces the most liver specific is because it is least produced in other organs. In the event of liver damage, however, the liver values do not increase the earliest (gGT, for example, rises earlier), as the enzyme is inside the (Liver / biliary tract) Cells are located, and are only released into the blood when they are damaged to the point that they perish.
Read more about this on our page "Increased liver values'.
AP (alkaline phosphatase)
The Alkaline phosphatase (AP) is typically at Diseases of the bile ducts (Biliary congestion, Viral hepatitis) and at Disorders in bone metabolism (Rickets, osteomalacia, M. Paget) elevated.
Of the INR is the modern reference value of the previously used Quick value and is a measure of the Blood clotting of the human. In order to make blood coagulation internationally comparable, the INR was invented, as the Quick value often used in the past was heavily dependent on the different laboratory methods used in a laboratory.
The INR value is calculated using Citrated blood determines which prevents premature blood clotting in the tube. Only in the laboratory is the blood clotting removed using special substances and the time until the first blood clot forms is measured. In healthy people this time is 20 seconds. This would one INR from 1 (Quick value = 100%). With certain diseases, like one Vitamin K deficiency (usually severe liver disease or with absorption problems of vitamin K from the intestine), with a Coumarin or Marcumar Therapy or at one Lack of fibrinogen the INR can be increased or the Quick decreased.
Read more about the topic here: INR
ammonia is a foul smelling gas that is found in the intestines of bacteria from undigested protein meals is produced. A healthy liver can intercept and metabolize harmful ammonia through the blood before it does damage to the human body.
If, on the other hand, the liver's performance is so reduced that it can no longer intercept and detoxify the ammonia; this is how the ammonia enters the great bloodstream. Ammonia can cause severe damage to the central nervous system (CNS) in particular. A typical consequence would be that Hepatic encephalopathywhich can be accompanied by convulsions, confusion and coma.
Normal values for liver values in men
- GOT (also ASAT): 10-50 U / L 10-30 U / L
- GPT (also ALAT): 10-50 U / L 10-35 U / L
- GGT (Gamma-GT): <66 U / L <39 U / L
- GLDH: <6.4 U / L <4.8 U / L
- Bilirubin: <1.1 mg / dL <1.1 mg / dL
- Alkaline Phosphatase (AP): 40-129 U / L 35-104 U / L
Normal values for liver values in women
- GOT (also ASAT): 10-30 U / L
- GPT (also ALAT): 10-35 U / L
- GGT (Gamma-GT): <39 U / L
- GLDH: <4.8 U / L
- Bilirubin: <1.1 mg / dL
- Alkaline phosphatase (AP): 35-104 U / L
Further information on the topic can be found here: How can I best lower my liver values?
Kidney values
GFR
Behind the abbreviation GFR in the context of the blood test, the so-called "glomerular filtration rate". It is a Kidney value, which indicates the volume of blood that the kidney (or the filtration apparatus of the kidney) filtered and thus "cleaned" becomes.
In addition to other kidney values in the blood count, the GFR is an important parameter that is used for Assessment of kidney function can be used. One problem with determining the value is that it cannot be measured directly in the blood serum, but using the so-called Creatinine Clearance must be determined. If the glomerular filtration rate is reduced, this can be an indication of a Renal failure be. The GFR value is not only used for the diagnosis or screening of kidney dysfunction, but can also be used for Follow-up and used to monitor kidney diseases.
The normal value for the GFR is around 120 ml / min for patients around 20 years old with normal, healthy blood pressure. Generally speaking, the normal value can fluctuate individually, depending on the time of day, the underlying blood pressure conditions of the patient and depending on age, height and weight.
leukemia
For the Diagnosis one suspected leukemia or leukemic disease as well as for process control and the Monitoring of blood cancer patients, blood sampling and blood counts are important tools. By identifying a large blood count the differential blood count can be used to determine whether and how the white blood cells are in the blood serum of the patient concerned (vicious) and whether other cell series, such as red blood cells or platelets, may also be affected and deviate from the normal values.
Thereby it is accordingly possible between different Types and subgroups of leukemia to distinguish that Extent of the disease to assess or - in the course of therapy – Treatment successes to assess.
If leukemia is present, it can show itself in the blood count in very different ways: The white blood cells can either humiliated or elevated, but sometimes even normal and inconspicuous depending on the type and stage of blood cancer.
The red blood cells and the Platelets are, however, mostly humiliated, as the production of these cells is often suppressed by the excess production of white blood cells. A blood test alone is usually not enough for leukemia diagnosis to make an absolutely reliable diagnosis, so you usually have one more Bone marrow examination follows.
Read more about the topic here: How do you recognize leukemia?

.jpg)