Urea increased
What does an increase in urea in the blood mean?
Urea is a breakdown product of the body, which is used for detoxification. Various substances are bound in such a way that they become water-soluble and can be excreted with the urine via the kidneys. In the case of urea, it is about the elimination of nitrogen, which is absorbed into the body in the form of proteins, for example. As a rule, an increase in the level of urea in the blood means that the kidneys are not functioning properly. However, a metabolic disorder can also lead to an increased production of urea or an excessive intake of proteins triggers an increase in urea in the blood.

What symptoms can indicate increased urea?
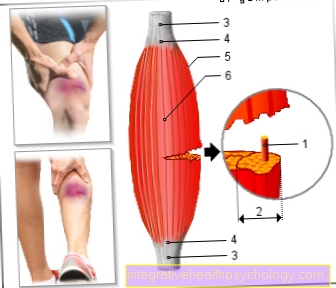
The increased urea in the blood causes the disease gout. A distinction is made between an acute gout attack and chronic gout. Nowadays in western society, which lives in abundance of food and has good medical care, acute gout attacks are particularly widespread. This leads to a very painful inflammation of individual joints. The big toes, the tarsal bones and the ankle are often affected, and the acute gout attack often affects the wrists, fingers and elbows. As a result, there is typically severe pain in the affected joint at night, and inflammation and swelling also develop there. After a few days, the symptoms of acute gout calm down again.
Chronic gout is very rarely seen here. This clinical picture is based on a permanently increased level of uric acids in the blood. The uric acid then builds up inside and outside the joints. Gout nodules can develop under the skin as well as in various organs (especially in the kidney). Since the increase in urea is often caused by a malfunction of the kidney, kidney dysfunction also often occurs. This manifests itself in a reduced urine excretion up to the complete drying up of urination.
Read more on the subject at: gout
Which diseases lead to an increased urea level?
There are various diseases that can lead to increased urea. The so-called primary hyperuricemia (increase in urine) is caused by kidney diseases and is often genetic. The impaired function of the kidneys leads to a disruption of uric acid excretion. The acute occurrence of the disease is usually caused by the consumption of alcohol as well as overeating and excessive consumption of meat.
The increased urea level is very rarely due to overproduction. These are mostly rare genetic defects. However, the increased urea level can also occur as a result of many drugs (aspirin and water tablets, some immunomodulating drugs). Poisoning or hormonal dysfunction can also lead to increased urea levels. More rarely there is an increased formation of urea due to sudden massive cell death, which can be caused, for example, by tumor diseases and leukemia.
The doctor does these examinations
The doctor usually first takes an anamnesis, in which a pronounced food intake or heavy alcohol consumption can be identified as decisive factors. In addition, the affected joint should be examined in the event of an acute gout attack. Usually there is swelling, redness and pain-related functional restrictions.
The joint can be punctured to clarify the diagnosis; many white blood cells (Leukocytes) and uric acid crystals can be seen under the microscope. If the joint cannot be punctured, an ultrasound of the joint can be performed instead.
In chronic gout, the gout nodules can be discovered in the X-ray, they usually appear in the form of a so-called soft tissue shadow or can appear as "holes" in the affected bones.
So an increased urea is treated
The therapy of the increased urea is based on a concept with many different starting points.
Since diet together with increased alcohol consumption is often the trigger of the disease, a low-meat (low-purine) diet should be carried out. Reducing or giving up alcohol also plays an important role. In addition, enough fluids (water or tea) should be drunk, 1.5 liters are a daily guide value.
Read more on the subject at: Diet for gout
In addition, drug therapy for the high urea level can be sought. So-called uricostatics (best known allopurinol) are used in particular. In an acute gout attack, pain relievers such as ibuprofen and, if necessary, glucocorticoids are often used at the beginning.
Read more on the subject at: Therapy of gout
Therapy for concomitant diseases plays another important component. Above all, kidney-friendly procedures should be used, as the kidneys play the decisive role in urea excretion. Special care should be taken with the use of diuretics (water tablets); these can both improve and worsen the excretion of urea, which is why the substances should be handled with care.
Concomitant diseases such as increased blood pressure are often treated with drugs commonly used in the kidneys and must therefore be carefully controlled. Here too, blood pressure medication that is gentle on the kidneys, such as sartans, should be used.
Read more on the subject at: Therapy of high blood pressure
How do I eat correctly when there is an increase in urea?
The increase in urea is mostly due to a certain diet, which can be found especially in the western industrialized nations. In addition to meat consumption, the consumption of too much alcohol and drinks that contain fructose (fruit sugar) also play an important role. Correct nutrition when there is an increase in urea is therefore primarily aimed at these risk factors.
So liquids should ideally be in the form of water and unsweetened tea. Ideally, drinks containing fructose and alcohol are avoided completely. In addition, foods containing purine (especially meat such as liver) should be avoided. A completely low-protein diet, however, is not recommended. Since the increase in urea is generally related to overeating and an overconsumption of food and energy, a low-calorie diet that aims at achieving a normal weight is generally recommended. Above all, reducing the consumption of high-sugar drinks and foods helps. Instead, you should focus on complex carbohydrates (whole grain products) and a lot of fiber (grains, nuts, vegetables).
Read more on the subject at: Diet for gout
What can the long-term consequences be?
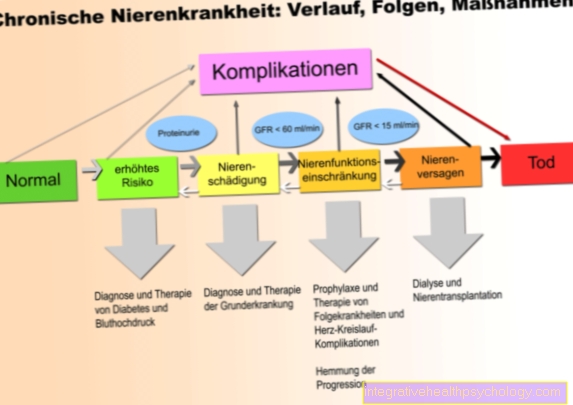
The long-term consequences of the increased urea in the blood are particularly evident in the kidneys, which are usually already damaged. The high urea value causes the substance to be deposited, especially in the kidneys. This leads to kidney stones, which in turn cause the urine to back up in the kidneys and acutely damage the tissue there. This can lead to serious complications up to life-threatening acute kidney failure.
Chronic inflammation can also arise from the uric acid deposits, which usually results in chronic progressive kidney failure, in which the kidneys are no longer able to produce enough urine to detoxify the body. In addition, the development of many metabolic diseases is favored. These include, for example, diabetes mellitus (diabetes) and the metabolic syndrome, which is made up of obesity, poor blood lipid values, diabetes mellitus and high blood pressure.
Increased blood pressure that occurs alone can also be caused by the kidney dysfunction. Metabolic syndrome, diabetes mellitus, and increased blood pressure are, in turn, risk factors for serious cardiovascular diseases.
What is the urea creatinine quotient?
Urea and creatinine are two substances that are excreted by the kidneys. Both substances can build up in the body if the kidney no longer functions properly. The ratio between the two substances can be determined via the urea-creatinine quotient. If the quotient remains roughly the same, this indicates that both substances are accumulated equally in the body. In this case, kidney dysfunction can be assumed, as the two important substances are no longer excreted.
Read more on the subject at: Kidney disease
If, on the other hand, only the urea increases while the creatinine remains the same, this also increases the urea-creatinine quotient. This suggests that increased urea production in the body is responsible for the high levels of urea in the blood. Depending on the underlying cause, different therapeutic approaches can be selected, which is why differentiating the origin of the high urea plays an important role in everyday clinical practice.