Hepatitis B.
Synonyms in the broadest sense
Hepatitis B virus infection, liver inflammation, liver parenchyma inflammation, acute and chronic viral hepatitis B, hepatitis B virus (HBV), infectious jaundice of virus type B.
Definition of hepatitis B.
The ones from Hepatitis B virus Inflammation of the liver is notifiable and is the most common cause of Viral hepatitis.
In about 90% of those infected, the disease heals without consequences. In the remaining 10% the infection becomes chronic and in approx. 1% of those with chronic hepatitis B it develops Cirrhosis of the liver and or Hepatocellular carcinoma (liver cancer, (Hepatocellular carcinoma, HCC) as a result of permanent inflammation.
The therapy of a chronic hepatitis B is through so-called Virus statics possible, but not always successful. Thus, the preventive vaccination the most important and safest measure to avoid a hepatitis B infection and to decimate the virus carrier as a constant source of infection.

Frequencies
In Germany 55% of all viral hepatitis are caused by HBV (hepatitis B virus) and the infection rate of the population is 0.2%. 300 to 420 million people worldwide are chronically infected with HBV, which corresponds to approx. 5 to 7% of the total world population.
The number of people infected and thus potential carriers of hepatitis B is estimated at around 600,000 in Germany. Every year around 50 to 60,000 new cases are added. Around 2000 infected people die each year as a result of hepatitis B.
Every year, an average of 0.5% of all patients with chronic hepatitis B develop liver cell cancer.
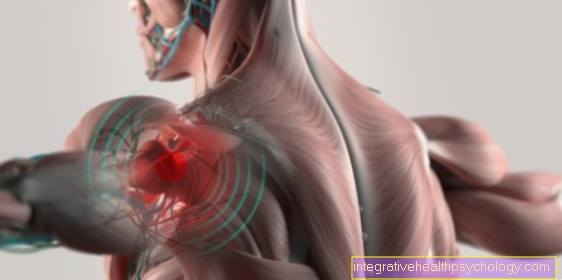
Symptoms of hepatitis
The symptoms of patients who have become infected with hepatitis B vary widely.
About 1/3 of the sick patients never develop symptoms (asymptomatic) and the disease often goes undetected.
About 1/3 of patients develop about 60-120 days after infection (incubation period) general, unspecific symptoms of illness such as headache, tiredness, fatigue, loss of appetite, weight loss, fever, joint and muscle pain and a slight feeling of pressure in the right upper abdomen. This course is called "anicteric " because there is no yellowing of the skin or eyes (jaundice).
About 1/3 of the patients suffering from hepatitis B develop after the above General symptoms include jaundice with yellowing of the whites of the eyes and skin, discoloration of the stool and dark urine (beer urine). This so-called "icteric“The progression begins after about 3-10 days, reaches its peak after about 1-2 weeks and usually disappears again after 2-4 weeks.
How quickly the acute hepatitis B infection heals and how severe the progression is depends, in addition to the general state of health, primarily on the age of the patient. An acute hepatitis B infection in adults heals completely in 90% of cases. In contrast, a hepatitis B infection in children usually leads to much worse courses and only heals completely in 10% of the sick. In 90% of the sick children, an acute hepatitis B infection turns into a chronic one (the virus can be detected in the blood for> 6 months).
Chronic hepatitis B is characterized by a favorable development of connective tissue remodeling of the liver tissue (liver fibrosis) and a shrunken liver (liver cirrhosis), which leads to an increased risk of liver cancer. With a chronic hepatitis B infection, the liver function can be impaired more and more and, however, only in a few patients goes into liver failure.
Read a lot more information under our topic: Symptoms of hepatitis B
Jaundice as a symptom of hepatitis B.
Jaundice is a typical symptom of hepatitis B disease, but only occurs in about 1/3 of infected patients. It usually follows the first stage, which is dominated by flu-like symptoms. Yellowing of the whole skin or just the sclera (the whites of the eyes) may occur. This yellowing is called jaundice. It lasts for a few weeks and then completely disappears.
Read more on the subject at: Jaundice
Pathogen and transmission
Pathogen and transmission:
The hepatitis B pathogen belongs to the Hepadnaviridae family.
The structure of the virus particle is of great importance for the diagnosis and the course of the infection. The hepatitis B virus consists of several antigenic components. Antigen effective means that the human body recognizes these structures as foreign and can form specific antibodies against them (Read more about this under: Immune system).
The structure and the virus components are:
- Superficial shell => HBs antigen ("s" for surface)
- HBV circular DNA core
- DNA polymerase (DNA amplification enzyme)
- Hepatitis B core antigen => HBc antigen ("core" like core)
- Hepatitis B envelope antigen => HBe antigen ("envelope" like envelope)
Learn more about the Build up of viruses
The infected person excretes the virus in almost all body fluids, such as blood, saliva, urine, semen, vaginal mucus, tears, cerebrospinal fluid (liquor), and in breast milk. These potential sources of infection lead to parenteral (through the gastrointestinal tract), perinatal (between the 28th week of pregnancy and the end of the first week of life) and communicable infections. The most common route of transmission worldwide is from the infected mother to the child (perinatal).
Nowadays this route of infection has been reduced by prophylactic measures in the "western world". In contrast, other transmission routes predominate, from which various risk groups are particularly affected. These include patients requiring transfusion (recipients of blood and blood products), patients requiring dialysis, medical staff, people with frequent and unprotected sexual intercourse (promiscuity) and IV. Drug addicts. It is estimated that more than half of the infections are transmitted in Germany. The infectivity (infectivity) of the virus is extremely high, it even exceeds the infectivity of HIV. As little as 1 µl of blood can serve as a source of infection.
An important feature of the hepatitis B virus is the fact that HBV multiplies its “genes” (DNA, genome) with the help of a special enzyme, reverse transcriptase, and can incorporate them into the DNA of healthy liver cells (hepatocytes). The HBV is therefore closely related to the actual retroviruses (e.g.: HIV).
Read more on the subject at: Causes of hepatitis B and transmission of hepatitis B.
How long is the incubation period?
The incubation period for hepatitis B is between 45 and 180 days. The average time span from infection to onset of symptoms is around 60 to 120 days. In about 1/3 of the cases, however, the disease is asymptomatic, so that no incubation period can be specified here.
Note: hepatitis B virus
This means that after an infection, despite recovery, the hepatitis B virus cannot be eliminated from the organism. Rather, a certain state of rest arises.
In extremely rare cases, e.g. the body is in a severe immune deficiency (immunosuppression), the infection can flare up again. Such an immunodeficient condition exists when strong immunosuppressive drugs are administered after organ transplants, after chemotherapy or in the case of a late-stage HIV infection.
Special case: hepatitis D virus infection
The hepatitis D virus can only become infectious with the help of hepatitis B. The hepatitis D virus (HDV) has a defect and can only multiply with the help of the hepatitis B virus surface antigen (HBs-Ag). The hepatitis B virus infection (HBV) is made much more difficult by the additional second virus. It is possible to be infected with HBV and HDV simultaneously, but HDV can also be grafted onto HBV. The vaccination against the hepatitis B virus always protects against the hepatitis D virus.
Further information is available from: Hepatitis D virus infection
diagnosis
In the patient consultation (anamnesis), the pioneering symptoms and causes can be identified or other causes can be excluded. In this way, specific questions regarding vaccinations against hepatitis B, previous transfusions or i.v. Drug addiction evidence reveals. In the case of acute hepatitis, physical examination often reveals painful pressure in the right upper abdomen and palpable enlargement of the liver.
The acute infection with the hepatitis B virus is detected by the detection of immunoglobulin M in the blood, which is directed against the antigen of the nuclear envelope (“core”) (IgM anti-HBc). In the case of hepatitis B infection, 100% of this immunoglobulin is detectable at the onset of the disease. IgM is an immunoglobulin that is the earliest antibody produced in the course of an immune response. This serves to activate the complement system associated with the immune defense. In the later course of the disease, the IgM is exchanged for the immunoglobulin G (IgG), which is produced by the B lymphocytes or plasma cells and remains in the body for a lifetime. IgG is either a sign of past hepatitis B or a chronic course of hepatitis.
You might also be interested in: Hepatitis B test
What is the hepatitis B titer / serology?
The term hepatitis B serology is understood to mean laboratory tests that are used to assess whether an (acute or chronic) hepatitis B infection is present and what the vaccination status is. There are several different hepatitis B virus components that can be detected in the blood. The components directly associated with the virus include the HBs antigen (hepatitis B-S antigen) and the HBe antigen (hepatitis B-E antigen). In addition, serology is used to detect antibodies that have been formed against components of the virus and circulate in the blood. These include anti-HBs, anti-HBe and anti-HBc. Depending on which of these antigens or antibodies are positive or negative, this allows different conclusions about a hepatitis B infection.
If, for example, HBs antigen is detected in the blood, this is evidence that an infection with hepatitis B is present. This is an acute infection as virus components still circulate in the blood. If anti-HBc and anti-HBs are positive, but all other values are negative, this indicates an infection that has taken place but is no longer active, i.e. clinically healed.
One of the values, the anti-HBs value, is used to test the vaccination status.If the anti-HBs value is positive and all other values are negative, this shows that a vaccination against hepatitis B has taken place. When this vaccination took place cannot be determined from these values. While in hepatitis B serology the blood is qualitatively examined for various hepatitis B markers, a quantitative measurement of the anti-HBs vaccine marker is made in the titer determination. If this value is above 100 IU / l, this indicates that the vaccination protection is (still) sufficient; a booster of the vaccination is not necessary. If the value is below 100, adequate vaccination protection is not guaranteed. The determination of the titer is important because there are no consistent results with the hepatitis B vaccination as to whether and when a booster vaccination is necessary after the primary vaccination. Therefore, the level of the anti-HBs value is used to decide whether a refreshment is necessary or not.
What is HBs?
The hepatitis virus is surrounded by a shell. Surface proteins are embedded in this shell. Derived from the English word for surface, they are known as HBs antigen. HBs is therefore part of the hepatitis B virus. If HBs is detected in the blood, this is an indication of an acute infection with hepatitis B.
What is a hepatitis B antigen?
There are several hepatitis B antigens. These are different components of the hepatitis B virus against which the human body develops antibodies when infected with the virus. The HBs antigen is a surface protein that occurs in the virus envelope. The HBc antigen is a protein found in the virus core. The c stands for the English word for core. As the virus replicates in the human body, another antigen is released, the HBe antigen. E stands for excretory. The hepatitis B antigens are therefore virus components that can be detected in the blood and are markers for an infection.
Active infection
The IgM-Anti-HBc (see above) applies in connection with the positive detection of the virus surface antigen ("surface") (HBs antigen), which, however, remains negative in 10% despite the presence of hepatitis B, as proof of active infection.
The HBe antigen is also regularly detectable, but only for a very short time. The typical pattern of an infection shows itself in a disappearance of the antigens (HBs-Ag and HBe-Ag) and an appearance of the antibodies against these antigens (anti-HBs and anti-HBe), which as an expression of the lifelong immunity can be detected in the blood forever stay. This phenomenon is called seroconversion and mostly shows up with a bland course of the disease.
In some cases it makes sense to determine the virus DNA (HBV-DNA), for example to assess how active a chronic infection is or how effective an antiviral therapy that has just been carried out is. A lot of DNA indicates active hepatitis, little DNA indicates dormant hepatitis.
Individual constellations of the various markers and their meaning:
Highly infectious patient:
- Anti-HBc: +
- Anti-HBs: -
- Anti-HBe: -
- HBs antigen: +
- HBe antigen: +
- HBV-DNA: ++
Low infectious patient:
- Anti-HBc: +
- Anti-HBs: -
- Anti-HBe: +
- HBs antigen: +
- HBe antigen: -
- HBV DNA: +
After vaccination:
- Anti-HBc: -
- Anti-HBs: +
- Anti-HBe: -
- HBs antigen: -
- HBe antigen: -
- HBV DNA: -
Healed infection:
- Anti-HBc: +
- Anti-HBs: +
- Anti-HBe: - / +
- HBs antigen: -
- HBe antigen: -
- HBV DNA: -
Sonography
During an ultrasound examination, the abdomen (acute abdomen) and its organs are visualized with the help of ultrasound waves. The transducer emits ultrasound waves that are absorbed or reflected by the various tissues it encounters. The transducer receives the reflected waves, which are converted into electrical impulses and displayed on a screen in different shades of gray.
In acute symptomatic hepatitis B, the liver may become enlarged (see also: swollen liver) and appear a little less hypoechoic (i.e. darker) due to a build-up of fluid in the liver (edema).
Chronic hepatitis B usually shows up with atypical changes that resemble an adipose-like texture. This means that the liver appears enlarged, it is more echogenic (that is, lighter) and appears smoother and rounded edges. Read more on this topic at: Fatty liver
If the chronic hepatitis persists for a long time, the signs of cirrhosis of the liver also appear. This shows up depending on the stage of cirrhosis
differently pronounced changes. The caliber of the hepatic vessels decreases in the process of the disease. As the disease progresses, the liver shrinks and in the late stages it can sometimes be as little as 10 cm. It then also appears very light, apparently only consists of nodules and the edge of the liver looks uneven and bumpy.
Sonography is not used to make a diagnosis because it cannot differentiate between the various causes of hepatitis, but rather helps to assess the extent of the disease.
Liver puncture / liver biopsy
A liver puncture allows liver tissue to be obtained, which the pathologist can then examine finely (histologically) with a microscope.
There are several ways in which liver tissue can be obtained.
The simplest type is a liver blind puncture, in which, as the name suggests, the liver is punctured “blindly” with a hollow needle. In this way a cylinder of tissue is obtained. With a little practice, this method can be carried out relatively easily and without major aids and is particularly suitable for diffuse liver diseases, e.g. hepatitis or cirrhosis of the liver, which affects the entire liver, must be diagnosed.
The targeted puncture of the liver is supported with the help of an imaging procedure such as sonography or computed tomography. The needle is inserted into the liver, so to speak, under visual control, so that a specific section of the liver can be punctured. The targeted puncture is always indicated in diseases that affect a specific section of the liver, for example in the case of unclear masses (e.g. tumors / metastases, etc.). A punch biopsy is not infrequently used for such localized findings because more tissue can be obtained with it. Both types of puncture are performed under local anesthesia.
Read more on the subject at: Liver biopsy
therapy
Depending on whether it is a acute or one chronic infection deals with the hepatitis B virus, treatment options vary.
Since an acute hepatitis B infection usually heals itself very well, there is usually no special virus-killing (antiviral) Treatment of distress. With very severe ones (brilliant) In the course of an acute hepatitis B infection, which can be accompanied by a decrease in liver function, the disease should be treated with so-called hepatitis B virus DNA inhibitors (HBV DNA inhibitors), which is the reproduction of the hepatitis B genome (DNA) prevent being treated. Also so-called Nucleoside analogs (Lamivudine, Enteacvir, Tenofovir), which also intervene at the level of the virus genetic makeup, can be used.
In any case, it is advisable to keep bed rest and to eat high-carbohydrate and low-fat foods, as well as avoid alcohol to relieve and regenerate the liver.
In the case of a chronic course of a hepatitis B infection (lasting> 6 months), the doubling / multiplication rate of the hepatitis B virus in the blood should first (Virus replication in serum / viral load), the inflammation values, the liver values (Serum transaminases), as well as the content of connective tissue within the liver due to the inflammation (Fibrosis) be observed in order to then be treated with the appropriate virus-inhibiting (antiviral) Start treatment.
In addition to the so-called interferon alpha / pegylated interferon alpha, which inhibits the replication of the hepatitis B virus, so-called nucleoside or nucleotide analogues, i.e. drugs that inhibit the replication of the virus at the gene level, are used as drug therapy.
The treatment of chronic hepatitis B with the above Virus-inhibiting (antiviral) drugs also involve some risks such as the development of many of the side effects associated with these drugs. These include flu-like symptoms, severe weight loss or a drop in the number of blood platelets (thrombocytes), which can then lead to bleeding in the further course.
So-called resistances can also develop. This means that the drug can no longer work properly and therapy may need to be stopped.
If liver function fails completely in the course of chronic hepatitis B infection, a liver transplant must be considered, as the liver is irreparably damaged.
Read more on the subject at: Therapy for hepatitis B
Vaccination, vaccine and booster
In order to prevent infection with a hepatitis B virus, the Standing Vaccination Commission (STIKO) recommends multiple active vaccinations against the hepatitis B virus.
The vaccine consists of a protein (HbsAG), which is genetically produced from brewer's yeast and enriched with aluminum compounds in order to actively fight the virus through one's own body (Immune response) to improve. In addition, the vaccination contains some stabilizing components (Antibiotics, formaldehyde or phenoxyethanol).
The vaccination is usually done in the muscle (intramuscular) of the upper arm (Deltoid) or in children in the thigh muscle. The body is immunized because the vaccine contains a substance that resembles a surface structure of the hepatitis B virus (HBs antigen) is very similar. As a result, the body learns to recognize this structure (and also to recognize it in the event of a real infection) and to act against it. This happens through the formation of trapping particles (antibody), which can bind to the corresponding surface structure. Armed with this knowledge of the surface structure and the associated trapping particles, the body can then successfully fight off hepatitis B infections in the future.
The standard vaccination should be 3 vaccinations for all children (Primary immunizations) after birth (week 0), at the age of one month and 6-12 months after the first vaccination. The protection against the hepatitis B virus begins about 2-6 weeks after the 3rd vaccination and lasts for about 10 years. After 10 years it is recommended to determine the number of defense molecules (anti-HBs) in the blood and, depending on the value, to carry out a booster vaccination (with a vaccination titer <100 I.U.).
In addition, adults who have an increased risk of being infected with the hepatitis B virus for work or not for work (e.g. health workers) should ensure that there is a sufficient proportion of virus-fighting defense molecules in their blood (Virus titre) and possibly have a booster vaccination. Likewise, immunocompromised people (e.g. dialysis patients) should have regular blood tests (titre controls) carried out and, in the event of an anti-HBs level <100 IU / l, should be given a booster vaccination.
If there is a possible infection e.g. due to a needlestick injury or mucosal contact with someone infected with hepatitis B, the Standing Vaccination Commission (STIKO) recommends a so-called Post exposure prophylaxis. This should be done as quickly as possible (<6 hours after contact) in the form of a so-called active and passive simultaneous vaccination. This means that both antibodies (antibody), which fight the virus immediately but do not form a memory (passive vaccination), as well as virus components (Antigens) for the formation of the body's own defense molecules (active vaccination) at the same time (simultaneously) be vaccinated in different places (e.g. different upper arms).
Likewise, infants born to hepatitis B infected mothers should receive post-exposure prophylaxis within 12 hours of birth.
Side effects that can occur as a result of a hepatitis B vaccination include temporary skin reactions (redness, pain, swelling, swelling of the lymph nodes) in the area of the vaccination site, allergic reactions, gastrointestinal complaints, headache and body aches as well as fever. With stronger vaccination side effects such as allergic reactions, a doctor should be consulted, who can assess the severity of the reaction and plan further action.
Pregnant women and nursing mothers must not be vaccinated because of developmental disorders that may occur. In addition, vaccination in people who are intolerant to components of the vaccine must be carefully weighed and the consequences of vaccination observed.
Also read on this topic:
- Twinrix®
and - Vaccination against hepatitis B
Can you get hepatitis B despite a vaccination?
Basically, with a sufficient HBs antigen titer after 3-fold vaccination as part of the basic immunization, the risk of infection is reduced to a minimum. It should be noted, however, that not all people respond equally well to the hepatitis B vaccine. There are patients who generate no or only a very low immune response; they are referred to as non-responders or low-responders. Such patients need more vaccinations than usual to ensure adequate protection. However, these people are not always filtered out through a blood test to check the success of the vaccination (titer determination). In this case, there is a risk that these people will develop hepatitis B despite the formal adequate vaccination. The Standing Vaccination Commission (STIKO) of the Robert Koch Institute therefore recommends checking the success of the vaccination by determining the titre after 4-8 weeks for all indication groups (patients with a weakened immune system, occupationally exposed persons, contact persons, trips to certain countries).
infection
Infection with the hepatitis B virus (HBV) usually occurs through blood contact or other body fluids (urine, saliva, tears, seminal fluid, breast milk). The hepatitis B viruses usually enter the body through very small injuries to the skin and mucous membranes.
In the early stages of an infection, a tiny amount of blood is often enough to transmit the virus from an infected person to a non-infected person. The risk of infection through other body fluids is much lower.
In this country, 40-70% of all cases are transmitted through sexual contact, with homosexually active men or prostitutes (frequently changing sexual partners) being particularly affected. Unprotected sexual intercourse with someone infected with hepatitis B is a high risk factor for such an infection.
Furthermore, the use of contaminated tattoo needles or syringes (e.g. in the drug mileu) holds particular risks of contracting a hepatitis B infection.
The risk of infection via blood or blood products is despite the improved testing for hepatitis B viruses (Hbs antigen testing / HBV DNA testing / anti-Hbc testing) still present before a blood donation or blood transfusion, but extremely low in countries with a very good hygienic standard - such as Germany.
The situation is different in nations with lower hygiene standards; here the risk of getting an infection in this way (via blood supplies) is much higher.
Another path of infection that should not be neglected is injury to persons employed in the healthcare sector (doctors, nurses, cleaning staff, etc.) with potentially infected material. In general, medical or dental staff are exposed to a significantly increased risk of becoming infected through needle stick injuries or comparable processes. Since (also in Germany) hepatitis B is a disease that affects a relatively large number of people (sometimes without even knowing it), special attention must be paid to a possible infection with hepatitis B after a needle stick injury or a comparable incident. Therefore, it is advisable for people working in the health sector to ensure adequate protection and, if necessary, to have a booster vaccination.
Read more on the subject at: Transmission of hepatitis B
How contagious is hepatitis B?
Hepatitis B is a contagious and sexually transmitted disease. The infection takes place from person to person. How contagious an infected person is depends on specific serological factors.Both newly infected and certain chronically ill people can transmit the pathogen. The pathogens are present in blood, semen, vaginal secretions, menstrual blood, tears, saliva and breast milk, with the concentration in the blood being by far the highest.
The risk of infection usually already exists before symptoms appear. The risk of infection depends largely on how many pathogens are in the blood and how the infection occurs. Most commonly, hepatitis B is transmitted through sexual contact. People with intravenous drug use who exchange syringes are also considered to be a high-risk group. But hepatitis B also plays a role in healthcare. Therefore, everyone in the healthcare sector should get vaccinated against hepatitis B. Hepatitis B can also be transmitted through improper tattooing or piercing or in community facilities if the hygiene measures are not followed. It is important that hepatitis B can also be transmitted from pregnant mothers to their unborn children. The transmission occurs during the birth process. Therefore, newborn babies born to at-risk mothers must receive prophylactic vaccination immediately after birth.
Can you spread hepatitis through kissing?
The virus that causes hepatitis B occurs in large numbers in the blood of freshly infected or certain chronically infected people. But they are also present in smaller quantities in saliva. The amount of pathogen here is 1000 to 10,000 times less than in the blood. So far, there is no firm evidence that hepatitis B can be transmitted through kissing. With closer sexual contacts, however, it is essential to ensure protected sexual intercourse, hepatitis B is one of the sexually transmitted diseases.
Is there a notification requirement?
There is an obligation to report hepatitis B. Accordingly, a report must be made to the health department in the event of suspected illness, illness or death due to hepatitis B. Likewise, the direct and indirect virus detection if it indicates an acute infection. The person concerned must be reported to the health department by name.
What is the course of a hepatitis B illness?
The hepatitis B disease has an incubation period of 6 weeks to 6 months. In about 2/3 of the patients there are flu-like symptoms which last for a few days. In about half of these patients, the skin also turns yellow. The acute infection usually subsides completely after 3-6 weeks. In up to 10% of infected patients, however, the course is chronic. Chronic hepatitis often goes unnoticed for a long time and is noticed by chance in a laboratory examination due to increased liver values. The risk of liver cirrhosis is 2-10% a year. If patients develop cirrhosis of the liver, the prognosis is often determined by its course. In the case of advanced liver cirrhosis (stage Child C), the 2-year survival rate is only around 40%. In addition, 2-7% of hepatitis B patients with liver cirrhosis develop hepatocellular carcinoma each year, which also leads to a reduction in life expectancy.
How long does it take to heal?
Acute hepatitis is not always symptomatic. If it is symptomatic, the duration of the acute stage varies between 3 and 6 weeks. The early phase (prodromal stage) with flu-like symptoms lasts for about 3-10 days, then the yellowing (jaundice) of the skin comes on which can persist for another 2-4 weeks and usually slowly regresses within this period. In 90% of cases, healing occurs spontaneously after a few weeks. In about 10% of the cases, however, there is a chronic course. This chronic form of hepatitis B has not yet been completely curable.
What are the consequences of a hepatitis B infection?
About 2/3 of hepatitis B infections are symptomatic. One to six months after infection, flu-like symptoms with fatigue, body aches, nausea, vomiting, diarrhea and fever occur. A few days later, the typical yellow coloration (jaundice) of the skin and eyes occurs in about 1/3 of the cases. The urine turns dark. An uncomplicated infection heals after a few weeks. There are seldom severe courses that end fatally. In about 1/3 of the cases the disease is asymptomatic, so it is not noticed by the person concerned. In about 90% of the cases the hepatitis B disease heals without consequences.
The main reason why it is so dangerous is that it can also take a chronic course. This is the case for 5-10% of those infected. The rate of chronification decreases with age. In newborns it is extremely high at around 90%. This underlines the need for adequate care and advice for patients with hepatitis B during pregnancy. The greatest risk of chronic hepatitis B lies in the development of cirrhosis of the liver (shrunken liver). Cirrhosis of the liver is a serious and incurable disease with a reduced life expectancy. In addition, the presence of liver cirrhosis increases the risk of developing liver cancer (hepatocellular carcinoma, HCC). If cirrhosis of the liver is present in patients with chronic hepatitis B, the 5-year chance of developing liver cancer is 10-17%. Patients with chronic hepatitis B are about 100 times more likely to develop hepatocellular carcinoma than healthy individuals. Both advanced liver cirrhosis and liver cancer are diseases that drastically reduce life expectancy.
How often do cases become chronic and why?
Up to 10% of people who become infected with hepatitis B develop a chronic course. The first phase of the acute infection often goes unnoticed. It has not yet been sufficiently clarified why certain people develop a chronic course. What is certain, however, is that the risk of chronification is higher the more one is at the initial infection. In infected newborns, around 90% of the diseases are chronic. In young children, the risk of chronic illness is still around 50%.
Can a hepatitis B infection be fatal?
Acute hepatitis, which occurs shortly after infection with the pathogen, is fatal in very few cases. In 0.5-1% of the cases, however, severe courses with fatal liver failure were described. Chronic hepatitis B, on the other hand, is associated with a reduced life expectancy in many cases. The patients can be symptom-free for years, even though they suffer from the chronic infection. If cirrhosis of the liver or even liver cell carcinoma develops, the disease will in most cases be fatal over a shorter or longer course.
If you have hepatitis B, can you breastfeed?
The literature on this subject is not entirely uniform. A mother with hepatitis B has a significantly higher risk of infection for the child during the birth process, depending on the viral load. Therefore, newborns born to mothers who have HBs antigen in their blood are usually vaccinated against hepatitis B with 2 vaccines immediately after birth. Two more vaccinations will follow in the next months of life to complete the basic immunization. The most widespread opinion is that this first vaccination (active and passive immunization) already protects the newborn from infection with hepatitis B through breast milk and that there are generally fewer pathogens in breast milk than in the blood. However, there are also voices that advise against breastfeeding in mothers with hepatitis B and positive HBs antigen in the blood. In general, this topic should be discussed with the treating gynecologist on a case-by-case basis.



















.jpg)



