Breast cancer screening
When should I start breast cancer screening?
Breast cancer is still the most common cancer in women. Regular screening is important in order to detect cancer in its early stages.
It is recommended to palpate the breast yourself once a month from the first menstrual period. Attention should be paid to newly emerging lumps and hardening.
Furthermore, the breast should be examined by a gynecologist once a year. The gynecologist can also do an ultrasound (sonography) of the breast.
Mammography screening (breast cancer screening) is recommended for all women between the ages of 50 and 69 once a year.
The costs for this examination are covered by the health insurance. These recommendations apply to women who have no genetic mutations or who have a family history of breast cancer.
Women with a genetic or family history are recommended to have a six-monthly palpation and ultrasound examination of the breast. This should be done from the age of 25 or 5 years before the age of onset of the affected family member.
Furthermore, these women are recommended to have an MRI of the breast every year from the age of 25 and an annual mammogram from the age of 30.

Independent palpation examination
Since breast cancer is currently the most common cancer in women, it is important to react early to changes and abnormalities in the breast tissue.
Breast cancer discovered at an early stage has a high chance of cure, which is why preventive medical examinations are particularly important.
Women over the age of 20 in particular should regularly have a preventive examination carried out by a gynecologist and also scan their breasts themselves monthly.
The exact instructions can be found at: How can you feel breast cancer?
Every woman over the age of 20 should check her breast for any changes once a month, preferably in the days after her menstrual period. For this it is advisable to proceed according to a fixed scheme:
First, stand in front of the mirror with your arms hanging loosely and look at your breasts individually and in the Side comparison on.
Look for changes in the skin, indentations, swellings, and changes in the shape of the breasts or nipples.Raise your arms above your head. Changes in the breast tissue can lead to the affected areas pulling inwards. In this position, too, look at both breasts, also from the side. Pay attention to such recovery of the skin or the nipples.
Squeeze your nipples together between two fingers. Make sure you do that liquid emerges from the nipple and if so, what color and consistency it is.
A leakage of fluid from the nipple does not necessarily have to be due to a pathological change, but it should be clarified and observed.Then feel with the flat hand remove the breast tissue with circular movements and clockwise.
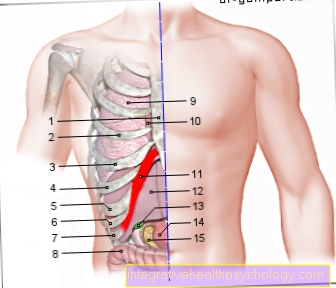
Use your left hand for the right breast and vice versa. Pay attention to possible Tenderness or Sensitivity to touch, as well as on node or Indurations in breast tissue.Now feel all four quadrants of the breast one by one. Pay attention to hardening, knots or pain. You can repeat this again in a lying position.
Finally, feel yours too Armpits on abnormalities, as in this area Lymph nodes which are the first wards the cancer spreads. Look for hardened lumps and swellings.
Most of the malignant changes in breast tissue are discovered by women themselves. Therefore, the self-examination should be carried out regularly!
You can find more information about this on our website Detecting Breast Cancer.
Prevention at the gynecologist

As part of the preventive medical check-up at the gynecologist, the doctor will also inspect the breast there and feel it for changes.
Some doctors also offer an ultrasound examination, or a special ultrasound examination called elastography.
In addition, from the age of 50, free mammography screening is offered every two years.
Basically, the more regularly you have the preventive care carried out, the better the chances of a cure if the result is positive.
- Ultrasound (Sonography)
If the doctor or the woman has felt a suspicious hardening in the breast tissue, an ultrasound examination can explain the type of hardening.
This examination is particularly preferred for young women because, in contrast to the established mammography examination, it does not involve any radiation exposure.
To do this, the doctor places a transducer with some ultrasound gel on the chest. Changes in the tissue reflect the sound waves, which are then picked up again by the transducer and converted into an image in a computer and displayed.
Benign changes, usually so-called cysts, appear smoothly bordered, uniformly black and homogeneous on ultrasound.
Fibroadenomas, benign tumors made up of nodular connective tissue from the breast, are more common in young women.
They are harmless and do not have to be removed as long as they do not cause any further problems.
In the ultrasound, they usually appear as a sharply defined, relatively homogeneous structure. If necessary, a tissue sample (biopsy) can be removed.
A malignant change in the breast tissue usually appears in the ultrasound as a blurred, uneven structure that radiates diffusely into the surrounding tissue.
To definitively confirm breast cancer, a biopsy must be taken, which is then examined microscopically.
- Elastography
Elastography is a special ultrasound examination that is designed to detect malignant tumors.
In doing so, one makes use of the property of malicious changes that they are often difficult to move and compress, as they largely consist of firm connective tissue.
The doctor applies light external pressure to the chest with the transducer. The device then records the extent to which the underlying tissue can be compressed by the pressure.
Normal tissue and benign changes are very elastic, malignant changes can hardly be compressed, so that the tissue layers shift against each other.
The elastography device records this tissue displacement and can thus provide information on pathological changes in the breast tissue. A biopsy is also required here for a definitive diagnosis.
How safe is ultrasound in preventive care?
The ultrasound (sonography) of the breast is a supplementary examination option in breast cancer screening.
Nevertheless, the breast ultrasound is a good and safe method to detect changes in the breast.
It is not suitable for early cancer detection because the changes are too small to be detected by the ultrasound. Breast ultrasound is most accurate in women with dense breast tissue. Mammography is still the safest and most accurate method. However, the ultrasound is used in preventive care to assess the lymph nodes in the armpit area. In addition, unlike mammography, the ultrasound examination does not require radiation.
- Mammography
Mammography is a very important tool in the early detection of breast cancer.
This is why it is reimbursed by statutory health insurance for women from the age of 50 every two years. Mammography is an X-ray examination, i.e. it is associated with moderate radiation exposure.
Therefore, the procedure is reluctant to use in young women. In addition, the assessment of the images is more difficult in young women, since in these the breast tissue is naturally denser and possible breast cancer foci can therefore be more difficult to detect.
However, for older women, mammography is the method of choice. X-rays with a strength of 25-35 keV (Kiloelectron volt).
The breast is recorded in two planes. This only takes a few minutes. During the examination, it is compressed between a Plexiglas plate and the object table of the device. Many women find this uncomfortable. As a rule, however, the examination should not cause excessive pain.
The attending physician can then recognize suspicious changes and microcalcifications in the images. Microcalcifications are small calcifications that are often formed by degenerate cells.
If such a finding is detected during the mammography, a tissue sample is usually taken afterwards to check whether it is breast cancer.
However, there is also criticism of mammography, as it can often lead to false positive results. This makes women unnecessarily insecure and confronts them with a stressful diagnosis that ultimately does not apply at all.
This happens all the more often the younger the woman is. Therefore, mammography is not recommended as a method for early cancer detection for women under 50 years of age.
Read more on this topic at: Mammography
MRI of the chest
In special cases, breast cancer screening can also be done using magnetic resonance imaging.
As a rule, however, this service is not reimbursed by the statutory health insurance companies.
The image of the breast is generated in the MRI using magnetic fields, so there is no radiation exposure.
However, at 30 minutes, the examination takes significantly longer than the mammography.
In 20% of the cases, false positive findings can also be obtained in the MRI of the breast, i.e. a suspicion of a tumor is expressed even though it is only a benign tissue abnormality.
Read more on this topic at: MRI of the chest
What is the cost of breast cancer screening?
Breast cancer screening is free.
From the age of 30, this includes a conversation with the gynecologist and palpation of the breast. If a change is noticed during this examination, further examinations will be initiated.
These examinations are then also free of charge for the patient.
Between the 50th and 69th A mammogram is also included every two years. If the patient wants a breast ultrasound, although it is not necessary, then the patient has to bear the costs herself.
The ultrasound is then offered by the gynecologist as an IGeL service. The costs are between 35 and 80 euros.
Does the health insurance company pay for the provision?
All statutory health insurance companies cover the cost of the breast cancer screening program.
The following investigations are included.
For women over the age of 30, a conversation with the gynecologist, palpation of the breast and the surrounding lymph nodes is included. It also teaches how patients can examine their breasts at home.
For women between the ages of 50 and 69, the mammography (X-ray examination of the breast) is covered by the health insurance every two years.
Some health insurance companies also cover the costs of further examinations. The offer differs from health insurance company to health insurance company and can be requested personally if necessary.
How often should I have breast cancer screening?
For early detection of breast cancer, it is recommended that you see your gynecologist once a year.
This applies from the age of 20.
Patients who have a genetic mutation or are known to have breast cancer in their families should have six-monthly screening.
Furthermore, the gynecologist should be consulted as soon as possible whenever there is a new change in the breast.
Is breast cancer screening also possible with implants?
Breast cancer screening is also possible with implants.
It is also possible to take part in the mammography screening. Since the breast is pressed together between two plates during a mammography, this can be a bit uncomfortable.
In so far only rare cases, however, the implant can be damaged.
An ultrasound or an MRI (magnetic resonance imaging) of the breast can also be performed without any problems. These examinations are then used as an alternative or in addition, if mammography cannot be used and only to a limited extent.
Preventive measures
Many women fear that they will develop breast cancer and wonder how they can prevent it from developing.
Some risk factors cannot simply be eliminated, such as a genetic predisposition. This can be determined by means of a genetic test.
The genes that play a role in the development of breast cancer are primarily BRCA1 and BRCA2.
They are inherited in families and increase the risk of developing breast cancer. However, they are only found in a few women.
Even women who received radiation in the chest area at a young age, for example because of Hodgkin lymphoma (a Cancer), develop breast cancer more often as a result.
Nowadays, when irradiating young women, particular care is taken to protect the breast tissue, but it is sometimes unavoidable.
An increased incidence of breast cancer has also been observed in women who had their first menstrual period early and their last menstrual period late. As a result, they are exposed to cycle-related hormone fluctuations for a long time, which can increase the risk of developing breast cancer.
However, there are also factors that can be actively influenced by every woman and that have a positive effect on health and cancer prevention.
It is particularly important that obesity is reduced. Too much fat in the body increases the level of female sex hormones (Estrogens), which can ultimately promote the development of breast cancer.
A balanced diet and plenty of exercise can have a protective effect in this regard. Also, alcohol should be drunk as little as possible, as more frequent alcohol consumption has a negative effect on the risk of breast cancer.
There are different opinions about the influence of smoking on the risk of breast cancer. So far it has not been proven that smoking increases the risk of breast cancer, nor that it has no influence on it. However, smoking is unhealthy and should be avoided if possible.
When a woman has a child, she should breastfeed it whenever possible. This has a positive effect on the risk of breast cancer. During the menopause and afterwards, hormone preparations should be avoided.
These increase the risk of breast cancer in some cases significantly and are therefore not recommended.
Possible symptoms of the carcinoma
A malignant breast tumor usually does not cause symptoms that suggest cancer. As a result, screening methods such as self-examination are extremely important for the early detection of a breast tumor.
Often a coarse knot felt in the chest that does not cause pain or other symptoms. Especially with the so-called Mastopathy (benign change in the glandular tissue of the breast), several lumps can be felt in some cases. The size and nature of a palpable lump in the breast can be so different that the type of lump can usually not be inferred from the tactile findings alone. Also Chest pain are not uncommon symptoms of a breast tumor. They are often caused by pent up fluid, which leads to feelings of tension and sensitivity to touch due to pressure.
In some cases one falls Inequality or asymmetry of the breasts regarding their size.
A breast tumor can be noticeable Skin retractions become. This symptom mainly occurs when the breast tumor spreads into the subcutaneous fatty tissue. In addition, sometimes a so-called Orange peel phenomenon (Peau d'orange), in which the skin over the breast tumor takes on the appearance of an orange peel.
Another symptom of a breast tumor can be a Fluid secretion from one or both nipples be (pathological Nipple secretion). There are also numerous causes for such a nipple secretion, ranging from many benign breast tumors to, in rarer cases, breast cancer and must first be clarified by a doctor. With bilateral secretion from the mammary glands, there is usually one hormonal disorder causally, for example through a pathologically increased production of the hormone Prolactinwhich stimulates the production of milk in the breast. However, a large number of drugs (especially drugs used in psychiatry) can cause nipple secretion.
Other topics that might interest you
- Follow-up care after breast cancer
- Breast cancer surgery
- Breast Cancer Cure Chances
- Breast cancer metastasis
- The breast cancer gene
- Lymph node involvement in breast cancer
- Breast cancer symptoms
- Breast cancer signs
- Health care
- Genetic test