Therapy of gastrointestinal bleeding
Definition gastrointestinal bleeding
A Gastrointestinal bleeding is a bleeding of the gastrointestinal tract that is visible to the outside. Blood is either vomited up or passed with the stool.Based on the appearance of the blood, conclusions can be drawn about the source of the bleeding.
Therapy gastrointestinal bleeding
In the foreground of therapy Gastrointestinal bleeding The first step is the stabilization of the circulatory system, as the loss of volume can lead to the risk of acute shock symptoms.
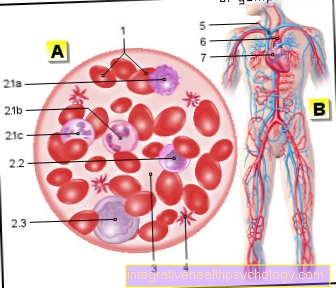
This will be foreign blood transfused or administered plasma expanders. The latter are also known as plasma substitutes and can be given as endogenous protein solutions or as artificially produced, modified starch solutions (so-called dextrans).

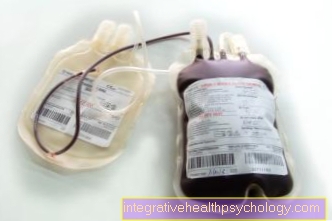
On the synthetic, also called colloid The designated solutions are used if the blood loss does not exceed 20% and no intolerance reactions are to be expected.
The name "colloid solution" indicates the volume-increasing mechanism of action of these substances: Due to the high protein content, a high level of suction, known as "colloid osmotic pressure", is built up in the blood vessels, which leads to the influx of fluid from the surrounding tissue into the vessels.
If the patient's circulation is stable, before e.g. surgical intervention, extensive diagnostics (see above) are carried out in order to find the intensity and exact origin of the bleeding source. Surgical treatment is not necessary for known esophageal varices (varicose veins of the esophagus):
These are preferably treated non-surgically by sealing bleeding vessels with rubber bands.
In this treatment method introduced by Goff and Stiegmann, also known as "ligature", the varices (varicose veins) are sucked in under endoscopic view and tied at the base with rubber band clips.
The method of choice today, however, is the so-called. Sclerotherapy (from sclerosing = desolate). By injecting a sclerosing agent, one of which is the polidocanol containing many unsaturated fatty acids, an artificial inflammation is caused in the vessel, the tissue swells and the vessel is permanently closed.
An initial hemostasis can thus be achieved. The same method of overmoulding vessels is also used in the treatment of varicose veins.
The mortality of the Esophageal variceal bleeding can be most effectively reduced by sclerotherapy:
The parameter, also known medically as the mortality rate, for evaluating the effectiveness of medical measures, drops from around 50 to 70% to 20 to 30% when the bleeding varices are sclerosed compared to conventional surgical therapy.
Nevertheless, potentially fatal complications can occur here too: The wall of the esophagus can tear when sucking (medical: rupture of the Oesophagus), parts of the walls of the muscle tube may die off (medical: necrosis) or bleeding, deeper injuries to the mucous membrane (ulcerations) may develop.
However, the justification for this intervention, which is associated with complications in around 10% of patients, is a comparatively great therapeutic benefit in the case of an overall very threatening disease, the mortality risk of which is many times higher without or with other treatment methods (around a third of patients die from the first Bleeding; see above).
The rate of recurrence of esophageal varices should also not be underestimated, i.e. The proportion of relapses: Even after treatment, varices (varicose veins) recur in 70% of patients.
The outcome of sclerotherapy and rubber band ligation may be improved by inserting a balloon called a Linton-Nachlas probe, which compresses the vessels in the stomach or. esophagus can bring about primary hemostasis.
If none of the above measures are successful, the esophageal variceal bleeding must be treated surgically, e.g. opening on Rib cage (medical: transthoracic) the esophagus is severed and the bleeding veins removed (this procedure, which is rarely used and is used as a last resort, is called "blocking operation").
Immediate surgery is necessary for spurting arterial bleeding (classified as Forrest 1a, see above) and for heavily bleeding defects in the posterior wall of the stomach due to the proximity to large arteries.
Often used are the electric and the Laser coagulation and the placement of metal clips (so-called hemoclips) to achieve initial hemostasis.
If there is a venous oozing hemorrhage classified as 1b according to Forrest, the chance is 80% that the bleeding will stop by itself.
Otherwise, the already mentioned methods of laser coagulation (laser sclerotherapy) and sclerotherapy are used here as well.
If this is not possible, the (statistically somewhat less successful) electrical coagulation (sclerotherapy) with a so-called electro-hydro-thermal probe) can be carried out.
In all cases, to support primary (direct) hemostasis, the additional administration of hemostatic drugs is an example Secretin and which inhibits the production of hormones in many glands of the body, Somatostatin called, tried.
Medicines to prevent acid production reduce the frequency of early recurrence of bleeding (so-called H 2 receptor antagonists, the "H" stands for the messenger substance histamine, which promotes gastric acid production) H2 receptor antagonist thus blocks the effect of histamine. Alternatively, the proton pump inhibitors, which are widely used today, are used to inhibit gastric acid production Omeprazole or Pantoprazole used.
In addition, usually a treatment to eliminate existing or to prevent the formation of Gastric ulcer carried out: The germ that has been proven to be the main culprit today Helicobacter pylori can be successfully eliminated with a two-week combination therapy with different antibiotics.)
You can find more information on this topic at: Gastric ulcer
In the case of lower gastrointestinal bleeding, e.g. by bleeding Meckel's diverticulum, these must be surgically removed.
For the treatment of the as Angiodysplasia Various treatment methods are available for the designated vascular malformations:
These can either also be removed surgically, electrically coagulated (sclerosed) or closed by arterial embolization (through clot formation in the vessel).
The principle of the last-mentioned method consists in the administration of liquid plastics or plastic beads into the vessel by means of a catheter in order to bring about its complete closure.
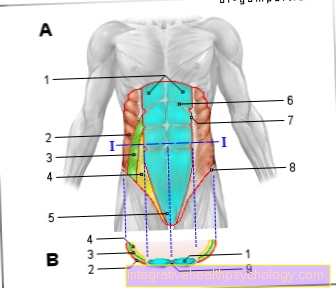
Classification according to Forrest

The examination with the endoscope (tube camera) enables the gastrointestinal bleeding to be classified into three groups, according to which further treatment is based.
The basis of the so-called is the activity of the bleeding:
- Forrest type 1
Active bleeding: Forrest type 1a is a spurting arterial bleeding Forrest type 1b is a venous oozing - Forrest type 2
bleeding that has already taken place- Forrest type 2a: the previously bleeding vessel is visible endoscopically within the injured area
- Forrest type 2b: there is an injury to the mucous membrane covered with clotted blood
- Forrest type 2c: the endoscopy shows an injury that is covered with blood clotted with hydrochloric acid - i.e. hematin)
- Forrest type 3
Injuries to the gastric or intestinal mucosa, the severity of which is not sufficient for classification in one of the above categories and from which no bleeding can (yet) be proven.
Complication and prognosis
Most often, complications are caused by the underlying disease (e.g. Gastric ulcer (see above) or a Stomach cancer).
The bleeding itself can also endanger the patient's life through circulatory shock.
In diseases of the liver there is a risk of decompensation due to the heavy loss of blood, i.e. the damaged liver can be hers function can no longer be maintained and there is a restriction in the synthesis capacity (lack of production of coagulants) with the typical signs of liver failure (e.g. bleeding due to reduced production of blood coagulation factors, "coma hepaticum", i.e. restrictions of brain function due to insufficient detoxification of harmful metabolic products, etc.).
Threat to life !!!
Overall, the risk of gastrointestinal bleeding is (Gastrointestinal bleeding) to die - despite therapy - approx. 10%.
More than 1000 people die in Germany from the consequences of bleeding caused by the group of NSAIDs (notsteroidal A.ntirheumatics, these include e.g. Diclofenac / Voltaren ®, Ibuprofen, indomethacin).