Fungal diseases
introduction
Fungal diseases belong to the infectious diseases and, in addition to bacterial and viral infections, represent a third large group of infectious diseases. The physician uses the term mycosis (Greek: mykes - the mushroom). Of course, not all of the many thousands of mushroom species that we know are dangerous for humans, but around 180 species can trigger diseases that are relevant to humans.
From a medical point of view, a rough classification of mushrooms into thread fungi (Dermatophytes), Mushrooms (Yeasts) and mold sense. The pathogen group of fungi differs in some important features from other pathogens such as bacteria or viruses, so that diagnostics and therapy options must be tailored to different fungal diseases.

The appearance of fungal diseases is subject to a wide spectrum. The most common fungal diseases are superficial and can be found on the skin or nails. They are called Tinea designated. This includes, for example, the annoying but harmless athlete's foot. In addition to these superficial mycoses, there are also systemic infections affecting the whole body and internal organs. These can be life-threatening, but occur almost exclusively in seriously ill and debilitated people on the basis of other underlying diseases.
Please also read our article on this Mushrooms.
Symptoms
The exact expression of the symptoms depends on the pathogen and clinical picture. common symptom of superficial fungal diseases are Skin changes. They mostly make up as round, but also diffuse reddening in spots noticeable. The skin begins to dandruff. Depending on the severity, a yellowish-white secretion to the fore. In addition, those affected complain a sometimes serious one itchingwho the distribution of the fungus favored.
They fall in hairy areas hair out, Mucous membranes can white coverings demonstrate. Deeper fungal diseases destroy the skin. It is about systemic mycoses, symptoms of serious illnesses appear such as fever, Shortness of breath, unconsciousness up to death.
root cause

Fungal diseases are caused by a number of different circumstances. What they all have in common is that the fungus must get into the body or skin in some form and be able to multiply there. The transmission usually takes place through direct contact from person to person, it can also happen indirectly.
The classic example of this is the athlete's foot that you get in the swimming pool. The fungi, or its spores, get on the skin and can nest there in the smallest folds or cracks and multiply. If the pathogen comes into contact with a blood vessel, systemic infections can develop. After a while, the typical symptoms of fungal diseases appear.
There are a number of risk factors that favor the development of a superficial fungal disease. This includes all circumstances that impair the skin's barrier function or disrupt the normal functioning of the immune system. Typically diabetes mellitus or peripheral arterial occlusive disease (paVk) called. In the course of diabetes, sensitivity disorders develop so that small lesions on the foot may not be noticed. Due to the reduced blood flow in the context of the PAV, the skin is no longer able to repair small damage to the skin immediately, so that fungi can penetrate more easily.
Personal hygiene is also an important factor in the development of fungal diseases. Poor hygiene can promote fungal diseases, on the other hand, fungal diseases of the skin are just as common in people with excessive hygienic behavior. The skin naturally has a natural protective coating that creates a slightly acidic environment. If this is attacked by constant washing, this makes it easier for the pathogens to penetrate the skin.
Fungal infections are sometimes transmitted through the air when a person inhales coughed up spores. An example of this is aspergillosis, which however does not occur in healthy people. The most severe fungal diseases develop in people with a weakened immune system. Here the body can no longer fight the infection, so that deep tissues and organs are affected.
Diagnosis
The diagnosis determines the type of therapy. In the beginning, the appearance gives Redness, Scaling and Spread important information in the direction of fungal diseases. To identify the pathogen, be Samples of skin, Hair or secretion which can then be examined under the microscope or grown on certain nutrient media. In this way, a specific remedy for the fungus can be selected. Further investigations may be included systemic mycoses necessary.
Athlete's foot and nail fungus
From Athlete's foot, lat. Tinea pedis, one speaks when a fungus is in the Space between the toes, spreads on the sole or the back of the foot. A Nail fungus, Tinea unguium, affects toenails, but can spread further over time. You belong to the most common fungal diseases and in most cases they are troublesome but harmless.
causes
These fungal diseases are usually caused by Thread fungi causing that over direct or indirect Transfer to the skin. Especially in public places like Swimming pools or Saunaswhere people are mostly barefoot is the infection risk the biggest. Here the ground can flakes of skin that have fallen off and the like to be covered with the fungus and get onto the skin of the next patient. About small Skin cracks the fungus penetrates the skin and can grow there. Risk factors like diabetes, Obesity and lack of hygiene awareness promote the development of athlete's foot.
Symptoms
To the classic Signs of athlete's foot, as they occur in many fungal diseases, count distinct itchingwhich increases over time, and reddened skin. If the disease is left untreated, the skin begins to flake and partially form small vesicles. Symptoms develop slowly at first, but then become impairment relatively quickly. The nail fungus is only noticeable on the nail for a long time. It changes color yellow-brownish and begins brittle and cracked to become. Also can White Stripes become visible. The thickness the nail substance slowly increases. In the course ignited the adjacent Nail bed and reaching over to the rest of the foot is possible.
diagnosis
Diagnosing these types of fungal diseases is relatively straightforward. On the one hand, you have the symptoms typical of fungal diseases such as Reddening of the skin, itching and damage from skin or nail. On the other side is that Proof of fungus to disposal. A skin or nail sample can be examined under the microscope, and a sample of the affected area is also taken and left in one laboratory cultivate so that one can determine the exact pathogen. The accuracy of the diagnosis largely determines the success of treatment in fungal diseases.
therapy
The therapy of fungal diseases, including that Treating athlete's foot or nail fungus, is done with Antifungal drugsthat work specifically against fungi. These are called externally or internally Tablets applied. Against athlete's foot, one is sufficient in most cases superficial treatment With Anoint, Creams or Sprays From the several times a day be applied to the affected areas.
Active ingredients contained are e.g. Terbinafine, Miconazole or Bifonazolethat work well against thread fungi. The treatment lasts depending on the course 10 days to several weeks. Oral antifungal drugs must be prescribed if the fungus has penetrated deeper layers of the skin. Nail fungus can be treated with special Nail polishes to treat. This may be helped by an ointment that softens the nail deeper layers to arrive, added. You seldom have to work systemically Taking medication to treat. The treatment of nail fungus lasts 3 to 6 months, as the nail is only healthy again grow back got to.
Genital fungus
A genital fungus is a form of fungal disease that is restricted to the penis or vagina. Women are more often affected than men.
root cause
In most cases, the pathogen causing genital fungus in men and women is Candida albicans, a yeast that is particularly good on mucous membranes.
The cause in women is usually a disturbed equilibrium of the vaginal environment, which is not acidic enough to keep the pathogens that occur in healthy people in check.
Stress, previous inflammations or infections, as well as pregnancy and the pill increase the risk of developing fungal infections in the genital area. Frequent washing with aggressive agents also damages the vaginal flora.
In men, disturbed skin flora, which is also influenced by drugs such as antibiotics or a weakened immune system, is a risk factor. Unprotected sexual intercourse increases the risk especially if the sexual partners often change, as direct transmission can take place here.
Symptoms
Symptoms are severe itching, burning and reddish, possibly scaly skin changes, often accompanied by white-yellowish secretions.
diagnosis
Due to the typical skin symptoms and information provided by the patient, one type of fungal disease is easy to think of. This is confirmed by a smear or a sample of skin or mucus under the microscope.
therapy
The therapy consists in the administration of antimycotics, which are used against many fungal diseases. As an ointment or cream, they must be used consistently for a few days. The symptoms then disappear after 1-2 weeks, in which sexual intercourse should be avoided.
Fungal diseases on the body and head
Fungal diseases can also occur in the rest of the body, especially between skin folds. The hairy scalp is also often the site of a fungal infection, but far less often than on the foot or toenail.
causes
These fungal diseases are also mostly caused by Thread fungilimited to infestation of the skin, hair and nails. Because of her special metabolism they can't Mucous membranes infested. The cause of an infection is transmission the mushrooms over infested objects, Humans or animals. So can Combs or dress, Bathroom areas and sick people can be a direct source of infection. The mushrooms invade in the tiniest cracks in the skin one and spread.People with additional risk factors are more susceptible to infection than others. These include diabetic and patients with Circulatory disorders or general immunodeficiency. Also elderly are more prone to fungal infections than younger ones. Incorrect hygiene measures can make it easier for the fungus to lodge in the skin.
Symptoms
The symptoms of this form of fungal disease are mostly typical Skin changes. The skin shows local, round redness on, in the further course it comes to the formation of white scales. In the center of the redness, the skin is usually lighter and of one red wall surround. There is also a clear one itching at the affected area. On hairy skin hair falls out or become damaged, the doctor speaks of the phenomenon of the mown meadow.
diagnosis
The typical one leads to the diagnosis visible findings. If the patient also reports itching, the diagnosis is made. Furthermore, as with all fungal diseases Skin or hair samples which are further examined under the microscope and in the laboratory. In this way, the exact type of fungus can be identified and targeted therapy initiated.
therapy
Therapy consists in the application of antifungal agents and depends on the extent of the complaints. Simple superficial fungal diseases are used Anoint or Creams, the Terbinafine or Miconazole included, treated locally. In severe cases, systemic oral administration of medication is necessary. A fungal attack of the head is against it always local and systemic treated. Can against the itching Ointments containing cortisone be prescribed. The therapy of fungal diseases is tedious and requires patience, but works in most cases.
Fungal infections in the mouth
Fungal infections of the mouth are infections of the oral cavity and throat area, which in most cases is caused by a type of fungus called Candida albicans.
This is a yeast that is present in the mouth and throat of many healthy people, but does not cause an infection. In people who are ill or have a very weak immune system, the yeast causes infections of the oral mucous membranes. This manifests itself in the form of severely reddened and inflamed mucous membranes on which a whitish, removable coating forms.
Read more on this topic at: How contagious are yeasts?
In addition to a strong burning sensation in the mouth and taste disorders, bad breath often occurs.
This condition is also known as oral thrush. Oral thrush in babies is relatively common.
Babies often become infected with an unknown vaginal yeast infection of the mother during birth. To treat the fungal disease, antifungal agents (please refer: Agents against fungal diseases), which can be used in the form of gel, rinses or lozenges.
Adequate oral hygiene should be observed to improve healing and to prevent infection.
Fungal infections of the mouth can also get further into the intestines. Please also read the articles:
- Yeast in the intestine
- Yeast in the mouth
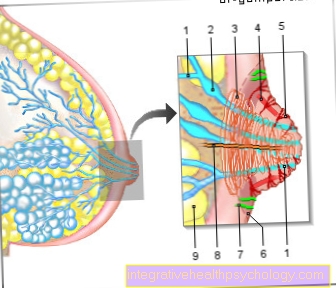
Fungal diseases of the skin
The different types of fungal diseases in the skin area are referred to in medical terminology as the Dermatomycoses summarized.
The infectious fungi are transmitted through human body contact or through objects contaminated with the fungi in everyday life.
The fungi that in most cases cause a fungal disease of the skin include Molds, Yeasts and so-called Dermatophytes.
Depending on the type of fungus and the affected area of skin on which it settles, a distinction is made between different types of Skin fungus. The most common fungal disease of the skin is athlete's foot, which is caused by dermatophytes and mainly affects the skin between the toes.
Other forms represent fungal diseases on hairy areas of the skin and on the head, in the groin region and on the hands. A fungal disease of the skin is characterized by a strong, new appearance itching from that with a redness and Scaling the affected area of skin.
Since you have most of the symptoms of a Skin fungus cannot clearly distinguish it from an allergic reaction or skin irritation, seek advice from a dermatologist. Evidence of the infectious pathogen should be provided in order to adapt the therapy precisely to the type of fungus present. Antimycotics are used therapeutically in the form of ointments that attack and kill the fungi and also have a caring component for the affected areas of the skin.
Systemic fungal diseases
This most severe type of fungal disease is rare, but it is a serious disease and requires intensive treatment.
causes
Fungal diseases affecting the whole body occur almost exclusively in patients who have a severely weakened immune system. Diseases such as AIDS or leukemia can lead to this. The immune system is also weakened as a side effect of cancer therapy with cytostatics. In addition, organ transplant recipients have an increased risk of developing systemic fungal diseases, as the immune system is suppressed by medication in order to prevent organ rejection.
Symptoms
The symptoms here are rather unspecific and depend heavily on the organ involvement of the fungus. Systemic mycosis often begins slowly. In the course of this, there may be shortness of breath, cardiac arrhythmias, nausea, vomiting and general fatigue. Often there are also visible reactions on the skin.
diagnosis
The diagnosis is made in addition to the anamnesis, a blood sample and a physical examination by taking a sample of the affected regions. This enables the exact pathogen to be identified.
therapy
Therapy is usually carried out on an inpatient basis using high-dose antimycotics. Venous administration is usually required. In addition, symptom control is of great importance.
therapy

The so-called play the decisive pillars of therapy for fungal diseases Antifungal drugs, a group of medicines that only works against fungi. In doing so, the special structure and metabolism of the mushrooms are used. One mechanism is that Inhibition of cell wall synthesisso that the fungus cannot grow, other substances settle in the cell wall of the fungi and destroy them.
Antifungal drugs are few side effects, since the attacked structures do not exist in the human organism. They are given in the form of Anoint, Creams, Sprays or as nail polishto be able to work locally. Heavier gradients, especially the systemic fungal diseases, require oral therapy in Tablet form or parenteral as an infusion. Supportive measures against fungal diseases are Hygiene measures such as changing clothes or bed linen frequently and reducing the risk factors mentioned above.
In the following, the most common fungal diseases are examined in more detail in terms of cause, diagnosis, symptoms and therapy.
forecast
The prognosis for fungal diseases is in most cases extremely positive. Although it can often take some time for the symptoms to go away completely, permanent damage is rarely to be expected in the case of nail or athlete's foot or other superficial fungal diseases. However, therapy should be initiated quickly to prevent it from spreading to deeper tissues.
The prognosis for systemic fungal disease is rather poor. Since the immune system is damaged, it is difficult for the body to fight the fungus. The prognosis of course depends on the patient and the associated manifestation of the mycosis.
prophylaxis
Simple measures often help to avoid fungal infections. A good one, but not an exaggeration hygiene, plays an important role. You should also be on manicured nails respect, think highly of. Shoes and socks should not be worn all day around the Let your foot breathe. Help in the swimming pool Flip-flopsto prevent athlete's foot.
In addition, it always makes sense to minimize your risk factors. This includes a well-adjusted Diabetes mellitus and healthy eating. Against Genital fungus you protect yourself effectively with Condoms and not changing sex partners too often. Despite all measures, however, fungal diseases cannot always be avoided. One systemic mycosis it is difficult to prevent, because that weakened immune system the reason for the severe infection is. It makes sense here to avoid contact with people who suffer from a fungal disease. Good therapy for the underlying disease is essential here.