embolism
definition
The term “embolism” describes the medical phenomenon that transported material is transported via the blood vessel system to another point in the body and causes a vascular blockage there.
The entrained material can, for example, detach itself from an arteriosclerotic plaque (vascular calcification) or consist of blood clots that have formed in the left atrium.
There is then only limited blood flow behind the vascular occlusion and the tissue there is damaged.

Causes of an Embolism
There are many causes of an embolism.
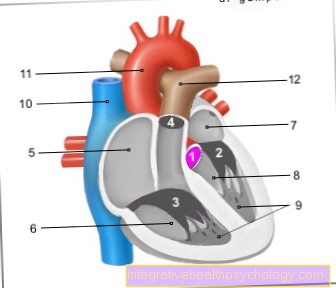
However, 90 percent of embolisms come from the heart and arise, for example, in the case of atrial fibrillation in the left atrium or in the ventricles if the heart has been damaged by a previous myocardial infarction.
It is also possible that the embolus forms on the heart valves, for example if a heart valve malfunctions (Vitium) or if the innermost layer of the heart wall is infected (Endocarditis).
In about 10 percent of cases, the cause lies in the arterial vascular system: Almost always, it detaches itself from a point that has vascular calcification (arteriosclerosis) is affected, a piece of this calcifying material is removed and becomes an embolus.
In rarer cases, the cause is a so-called "paradoxical embolism": through a hole in the wall of the heart sheath (open foramen oval), which some people have without knowing about it, an embolus that has detached itself from a venous thrombosis can enter the arterial system and trigger an embolism there.
Other causes include cholesterol embolism, in which cholesterol deposited in the arterial walls is detached, an embolism from tumor tissue in cancer, or air or fat embolism (see below).
thrombosis
A thrombosis is the development of a blood clot in the vascular system. Most often, thrombosis develops in venous vessels, mostly in the deep leg veins.
Causes are changes in the vascular wall, slow blood flow and blood disorders. However, thrombosis is also possible in the arterial blood vessel system.
It differs from an embolism in that, with thrombosis, a blood clot gradually forms at the point of the blood vessel that is later affected by the vascular occlusion. (In embolism, the material that closes the vessel comes from another part of the body).
In most cases, arterial thrombosis is caused by arteriosclerosis (vascular calcification) or by inflammatory changes in the arterial walls. Less common causes are disorders of the blood or blood clotting. The arterial thrombosis also occurs as a consequence of an embolism and thus enlarges the occluded vessel section both in front of and behind the embolus.
Read more on the topic: Thrombosis and Xarelto®
Signs of embolism
The signs of an embolism vary depending on the location of the embolism. In half of the cases, pulmonary embolism follows deep vein thrombosis (DVT).
In emboli that occlude an artery in the arm or leg, the following six signs are typical of the affected limb:
- Sudden, very intense pain
- paleness
- Loss of feeling
- Inability to move or decreased
- Missing pulse
- shock
These six signs are very specific to limb arterial embolism and are likely to suggest this diagnosis.
In pulmonary embolism, shortness of breath, rapid breathing, chest pain, and an increased heart rate are typical.
Other signs include symptoms of a leg vein thrombosis, chest pain, and blueing of the lips, head and neck. In severe cases it leads to unconsciousness and cardiovascular arrest.
When a stroke is triggered by a brain embolism, neurological deficits occur suddenly. Depending on the affected brain region, visual disturbances, speech disturbances, unilateral motor and sensory deficits, swallowing disorders and amnesia are possible.
An embolism of the mesenteric artery, which supplies most of the intestine with blood, results in severe abdominal pain at the beginning.
Read more on the subject at:
- Deep vein thrombosis (DVT)
- Causes of deep vein thrombosis
Different forms of embolism
Air embolism
In air embolism, the embolus (as the name suggests) consists of air. An air embolus typically occurs when an intravenous infusion or medication is given.
Air in the infusion system or in the syringe gets into the vein and is transported through the venous blood vessel system. Usually, the maximum amount of air that occurs is smaller, but this can be absorbed (taken in) by the blood and is therefore not a cause for concern.
If there is approx. 70 ml of air in the blood vessel system, all branches of the pulmonary arteries contract, so the air triggers a pulmonary embolism as an air embolism. The causes of so much air in the blood vessels are injuries, accidental intravenous administration (e.g. of an empty syringe) or surgery on the chest and / or heart.
Fat embolism
In fat embolism, the embolus (as the name suggests) consists of fat. Typically, a fat embolus arises in the context of fractures of long tubular bones: The bone marrow contains a lot of fat and can get into the blood vessels and be carried away as an embolus because the fat accumulates in the blood.
Fat embolism can also occur as a rare complication of bone surgery, crushing of soft tissue, or burns.
Typically, the fat is carried into the pulmonary arteries via the blood vessel system, where it triggers a pulmonary embolism. If parts of the fat embolus are carried into the blood vessels of the brain, a stroke is possible.
In addition, fat in the blood vessels disrupts the blood clotting system, small skin bleeding (Petechiae) can occur or severe coagulation disorders like the Consumption Coagulopathy are possible.
Read more on this topic at: Fat embolism
Pulmonary embolism
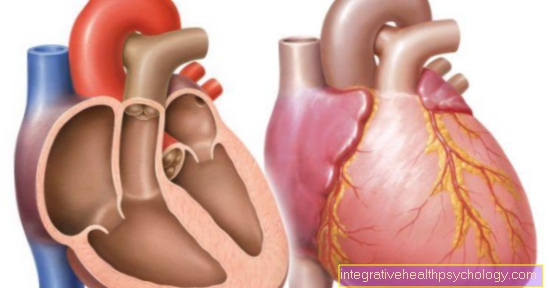
In pulmonary embolism, the embolus typically comes from the deep leg veins in which a thrombosis has formed (especially when sitting for long periods, e.g. on long-haul flights).
The embolus then detaches itself from the thrombus material in the leg vein, is brought to the heart via the venous system and finally ends up in one of the four pulmonary arteries or their branches.
In rarer cases, the embolic material can also come from the right heart or superior vena cava. The pulmonary arteries carry deoxygenated blood from the heart to the lungs, where it is enriched with oxygen and then transported back to the heart via the pulmonary veins.
If a pulmonary artery is "blocked" by the embolus, less blood can be supplied with oxygen, which is noticeable through shortness of breath and rapid breathing. In addition, the patients complain of chest pain and an increased heart rate.
In severe cases, there is cyanosis in the head and neck area (blue discoloration of the skin), in very severe cases, unconsciousness and possibly cardiovascular arrest.
If the pulmonary embolism is very small, i.e. only a small branch of the pulmonary arteries is blocked, there are no symptoms. The diagnosis of pulmonary embolism is made by a CT examination with contrast agent, and various laboratory values are also determined, for example, to rule out a heart attack (which would present itself with very similar symptoms).
In the acute phase, minor pulmonary wrinkles are treated with heparin, a blood-thinning drug, as well as with oxygen and painkillers. Larger pulmonary embolisms are treated with fibrinolysis (a drug designed to dissolve the embolus) or, in absolute emergencies, with surgery.
You might also be interested in: How do I recognize a pulmonary embolism? and Xarelto®
What is a cholesterol embolism?
A cholesterol embolism - not to be confused with a fat embolism - results from the closure of a vessel with cholesterol crystals.
This happens in people whose vessels are riddled with plaques containing cholesterol (arteriosclerosis), and in whom such plaques dissolve and get stuck downstream in the vessel.
In most cases, a cholesterol plaque dissolves due to medical measures that manipulate the vascular wall (e.g. cardiac catheter, CVC).
Read more on the subject below: Cholesterol
What is a cement embolism?
The rare cement embolism (also called “Palacos embolism” after the name of the most common cement) occurs when one or more vessels are closed with bone cement during orthopedic operations.
In these operations, bones are usually opened to anchor prostheses and then closed again with cement. In the process, small pieces of cement are probably washed into the bloodstream, which constricts in the pulmonary vessels and traps the pieces of cement like a filter.
During the operation, this is usually noticed by the patient's heartbeat and breathing getting faster. So far it is unclear to what extent hypersensitivity reactions and simultaneous fat embolism still play a role.
The most common types of emboli
- The most common source of embolism is deep vein thrombosis.
- Then the fat embolism is relevant, which is washed into the bloodstream during operations on the bones,
- followed by cholesterol and zeme embolisms.
stroke
A stroke occurs in around 85% of cases due to the occlusion of a cerebral artery or its branches and is then referred to as "ischemic stroke".
About a fifth of these cases are caused by an arterial embolus that has developed in the heart: In atrial fibrillation, the atria contract only in an uncoordinated manner. A large part of the blood is therefore not passed on to the ventricles, but rather circulates in the atrium, can clump and form an embolus.
However, a venous thrombus can also be the cause of a stroke. In particular if the foramen ovale of the heart is not closed, a thrombus from the venous blood system can be flushed into the body's circulation without the filter station in the lungs and thus quickly into the brain. Most people do not notice this defect in the heart, as it usually causes no to mild symptoms.
Another common cause (60%) of ischemic stroke is arterio-arterial embolism. The affected patients have atherosclerotic changes e.g. in the main or carotid artery, parts of which become detached and carried as an embolus in the arterial system until they get stuck in a cerebral artery.
The result of the cerebral artery occlusion is an acute neurological deficit: the capabilities that are controlled by the brain area that is supplied by the now closed blood vessel are only limited or not possible at all.
Based on the failure symptoms, conclusions can be drawn about the occluded artery before the examination using CT or MRI. Depending on the affected region, visual disorders, speech disorders, unilateral motor and sensory deficits, swallowing disorders and amnesia (impaired memory) are possible.
Read more on the topic: Stroke - these are the signs
Consequences of an embolism
An embolism closes a vessel, the part of the vessel located behind the embolus is no longer supplied with blood and the associated tissue is no longer supplied with blood.
How severely the tissue is damaged depends on the type of tissue affected, the duration of the vascular occlusion and the extent of the collaterals (means how well the tissue is still supplied with blood by other vessels). In the worst case, the tissue dies.
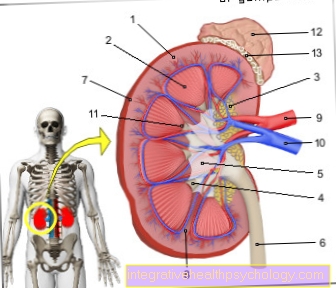
The consequences of an embolism in the leg or arm can be: compartment syndrome (increased pressure in the extremity with damage to the surrounding tissue and nerves) and reperfusion trauma with rhabdomyolysis (dissolution of the muscle fibers). This leads to an acidic metabolism (metabolic acidosis) and electrolyte disturbances and there is a risk of acute kidney failure.
The consequences of a cerebral embolism or a stroke are also serious. The brain tissue can only survive for four to a maximum of ten minutes without a blood supply. In the event of a stroke, brain tissue dies and the capabilities that are controlled by the affected brain area are only possible to a limited extent or not at all.
Since vital organs are often affected, an embolism can also lead to death if left untreated.
It therefore requires rapid diagnosis and treatment. Depending on the cause of the embolism, affected patients have to take anticoagulants (anticoagulants) and / or wear compression stockings for a while or for life.
Read more on the subject at:
- Compartment syndrome
- metabolic syndrome
Embolism in the leg
In the case of an embolism in the leg, a blood vessel in the leg is closed by an embolus, doctors speak of an "acute arterial occlusion". 70% of acute arterial occlusions in the leg are triggered by an embolus that originates in the heart, about 10% are caused by an arterio-arterial embolism (embolus detaches from atherosclerotically altered arterial wall, is transported into the leg and clogs a vessel there ).
Due to the vascular occlusion, the leg is poorly or not at all supplied with blood in the section behind it, the symptoms of the embolism in the leg can be explained by the insufficient supply of oxygen. The typical symptoms and signs are: pain, missing pulses in the section of the leg behind, paleness, sensory abnormalities and / or numbness, motor weakness up to paralysis and affected patients may show symptoms of circulatory shock.
In the case of an embolism in the leg, it is important that the diagnosis is made quickly and that treatment is started quickly in order to restore blood circulation. In addition to a physical examination, a Doppler ultrasound examination is performed, which can depict the flow within blood vessels.
In cases where there is residual blood flow, lysis therapy can be initiated (the embolus is dissolved by medication); in more severe cases, the blood vessel must be surgically recanalized (thrombectomy, embolectomy). After the treatment, the patient's blood clotting is slowed down with suitable medication.
Embolism in the eye
In the case of embolism in the eye, the embolus usually comes from the carotid artery or from the left atrium. This embolus closes the A. centralis retinae, the central artery of the retina, which leads to blindness of the affected eye after only 30 seconds due to the lack of oxygen.
There is no pain. The retina can survive for about 60 to 90 minutes without blood flow, after which it is irreversibly damaged. In the examination by the ophthalmologist, the loss of vision, the loss of the pupillary reflex and, on the ophthalmoscope, a whitish-greyish discoloration of the retina are noticed.
Therapy options are poor, attempts are made to dissolve the embolus by massaging the eyeball and / or using drugs that inhibit blood clotting. Unfortunately, there is usually no improvement, but the eyesight of the affected eye is lost. Spontaneous improvement is only possible if the central artery is not completely blocked.
Find out more about the topic here: The embolism of the eye.