Colon cancer
Synonyms
- Intestinal tumor
- Colon cancer
- Colon tumor
- Colon cancer
- Colon adenocarcinoma
- Rectal cancer
- Sigmoid cancer
- Rectum approx
English: colon cancer
Medical: Colorectal carcinoma
definition
This common type of cancer affects about 6% of the population and is the second most common type of cancer in both women and men. Colon cancer is a malignant, uncontrollably growing tumor that arises from the cells of the lining of the colon.
The main causes of colon cancer are eating habits. In most cases, colon cancer causes symptoms late, which are rather unspecific.
Since the tumor grows slowly compared to other types of cancer, it gives those affected enough time to diagnose it with good preventive care and thus to be able to combat it at an early stage.

Note
All information given here is only of a general nature, tumor therapy always belongs in the hands of an experienced oncologist (tumor specialist)!
Epidemiology
The incidence peak of colon cancer is beyond the age of 50, with men falling ill more often than women (approx. 60:40). In Germany around 49 out of 100,000 people fall ill every year and the risk of falling ill increases steadily with age.
Colon cancer affects 6% of the population and around 2.5-3% of the population dies from this cancer.
You might also be interested in: Is Colon Cancer Hereditary? or Lynch Syndrome
Symptoms
Like many other types of cancer, colon cancer is silent for a relatively long time. This long absence of symptoms makes many types of cancer so dangerous, as they could often be treated well in the early stages, but only lead to symptoms and become noticeable in later stages.
Symptoms that could indicate colon cancer include changes in bowel habits. This could, for example, be a sudden, frequent occurrence of constipation (Constipation) or diarrhea (Diarrhea) or show the alternation of both.
Another possible symptom is the admixture of blood with the stool. Furthermore, an increasing decrease in performance, physical weakness, weight loss and - usually only in the late stages - pain can be an indication of the presence of colon cancer. However, none of the symptoms mentioned is specific to colon cancer. There are no reliable early symptoms, which is what makes early diagnosis without the use of a colonoscopy so difficult.
Read more on the topic:
- Colon cancer symptoms
- Blood in your stool and stomach pain
Signs
As for many other types of cancer, there are no early symptoms for colon cancer. That is exactly what makes them so dangerous. Because most types of cancer are relatively easy to treat, especially in the early stages.
What makes them so tricky is that they are often noticed so late that they are already at an advanced stage, which can also be treated, but has a poorer prognosis.
So there are no specific signs that reveal colon cancer. There are only symptoms that can be interpreted as an indication of colon cancer. This includes, for example, the admixture of blood to the stool.
Changes in bowel habits can also be an indication. For example, as sudden frequent constipation (Constipations) or diarrhea (Diarrhea) or a change of both.Another symptom that can generally be an indication of the presence of a tumor is an increasing decrease in performance and an unwanted weight loss.
Read more on the topic: How do you recognize colon cancer?
Diarrhea / constipation
Irregular bowel movements, such as alternating constipation and diarrhea, are a common symptom of colon cancer. This occurs because the tumor narrows the intestinal space and stool passage is no longer guaranteed. The sufferer experiences this through constipation and a feeling of gas. The bacteria in the intestine multiply uncontrollably at this point and thereby liquefy the stool. The bacteria dissolve it so that it becomes so fluid that it can pass through the intestinal area as diarrhea.
Back pain
Back pain in colon cancer can be interpreted as “metastases” until the opposite is proven, meaning that the colon cancer has spread. The spinal bodies are the preferred place for colon cancer cells to settle once they enter the bloodstream. At this point, the chances of recovery are very poor. If more than one organ is affected by the scattered foci, one speaks of a palliative situation in which healing is no longer possible.
Find out more about the topic: Back pain as a symptom of colon cancer
Colon cancer pain
Pain is not an early symptom of colon cancer, nor is it a symptom specific to colon cancer. If colon cancer is present, pain in the abdomen can occur, but this usually only occurs in later stages of the tumor.
Other possible symptoms include blood in your stool, changes in bowel habits such as sudden constipation (Constipation) or diarrhea (Diarrhea) or a change from both as well as reduced performance and weight loss. However, none of these symptoms are specific to colon cancer, and they all often only occur at an advanced stage of the tumor.
Read more on the topic: Colon cancer pain and Pain in the rectum
diagnosis
Basically, this is the basis of any clinical diagnosis Conversation with the patient (anamnese), in which numerous things are learned. The questions vary depending on the complaints.
For example, if you suspect colon cancer, your doctor might ask about the following:
- Stool changes
- Blood to the chair
- Pain
- Loss of performance and fatigue
- unwanted Weight loss
- relatives with colon cancer
- the presence of Risk factors how Smoke and one-sided diet and previous illnesses
Furthermore, a Blood collection to check the laboratory values. Colon cancer shows with the usual laboratory parameters no specific changes, but it can, for example, become a Anemia (anemia) come as part of the disease.
Next comes the essential one digital rectal examinationSo the doctor puts his finger into the anal canal to feel for possible abnormalities. About 10% of all carcinomas of the Intestines and Rectum are so palpable that this examination is essential, even if it is usually not very pleasant for the patient.
The next step in the investigation is usually the Colonoscopy (Colonoscopy) at the whole Large intestine is observed by means of a tube inserted rectally with a camera and can be examined for tumorous changes. The examination usually takes place in Short anesthesia instead of.
Because colon cancer almost always consists of something called Adenomas (Mucosal swelling) and the risk of developing adenomas in particular from the age of 50 increases significantly, takes over Health insurance from 55 years of age the cost of two control colonoscopies every 10 years to look for such adenomas.
If an adenoma is found, this will be done during the colonoscopy removed by means of a small loop and afterwards examined histologically to be able to determine whether this is already a preliminary stage or even a manifest colon cancer and, if this is the case, whether during the ablation all suspicious parts removed could become. It turns out in the colonoscopy that one carcinoma (most common form of colon cancer) is available, further investigations will follow. Which includes Ultrasonic (Sonography) and Computed Tomography (CT) of the upper abdomen and a X-ray image of the rib cage (thorax) around Metastases to determine or exclude. Furthermore, so-called Tumor markers determined in the blood. In particular, they are used after therapy Course of treatment to be able to judge.
Rapid test
There are several methods that can be used to test for colon cancer relatively quickly. First and foremost the digital rectal examination, with which approx. 15% of the tumors can already be felt (for this, the examiner inserts a lubricant-coated index finger into the patient's anus).
There are two chemical tests that can be used to detect blood in your stool. However, they cannot determine whether this is due to a tumor or another source of bleeding. At most, they give an indication of the need for further investigation. These two tests are called the iFOBT and the Guaiac Test (also known as Haemoccult). The iFOBT has now proven to be more precise and clearer.
Read more on the topic: These colon cancer tests exist, and they are so reliable!
Tumor markers
Tumor markers are certain proteins in the blood that are generally found in everyone, but are significantly increased in certain cancers. They never serve as an absolute confirmation of the diagnosis in the case of suspected cancer, but rather only help the practitioner to monitor the progress. After the first cancer, you can use regular checks to indicate a relapse (a recurrence of the cancer).
The so-called CEA (Carcinoembryional Antigen) is particularly groundbreaking for colon cancer, as well as CA 19-9 and CA 50. The more well-known enzyme value of LDH (lactate dehydrogenase) can be increased in rapidly growing tumors because it stands for cell breakdown.
For more information, see: Tumor markers
Types of tumors and their distribution in the large intestine
90% of colon carcinomas arise from the glands of the thick mucous membrane. They are then called adenocarcinomas.
In 5-10% of cases, the tumors form a particularly large amount of mucus, so that they are then called mucinous adenocarcinomas.
In 1% of cases, a so-called signet ring carcinoma is diagnosed, which looks like a signet ring under the microscope due to an accumulation of mucus in the cell and therefore bears this name. The localization of the carcinomas (malignant cancer) is divided according to the frequency as follows:
- 60% in the rectum ("rectum"; Please also read our article on this Rectal cancer)
- 20% in the sigmoid colon (section of the large intestine in the left lower abdomen)
- 10% in the cecum (caecum; sac-like initial part of the large intestine)
- 10% in the rest of the large intestine (colon).
causes
The risk of colon cancer (colon cancer) increases steadily with age. An increase in the incidence rate is particularly evident from the age of 50.
Colorectal adenomas are benign Mucosal growths (polyps), which from a certain size (> 1cm) have the tendency to develop cancer (degeneration).
There are various histological forms of differentiation between polyps:
The tubular adenoma has that lowest risk and the villous adenoma that greatest risk to degeneration. The mixed tubullo-villous adenoma carries a medium risk of degenerating into a malignant cancer (carcinoma).
Origin and development of colon cancer:
Healthy colon

View from the point of view of a colonoscopy
- Intestinal lumen / intestinal opening
- Intestinal lining
- Haustren = small “normal” sinks in the area of the large intestine
Colon polyp

View from the point of view of a colonoscopy
- Colon polyp
Colon polyps can represent the preliminary stage of colon cancer.
Colon cancer

View from the point of view of a colonoscopy
- Colon cancer
The colon cancer extends into the intestinal tube and threatens to close it completely
Eating habits are also increasingly being held responsible for the development of tumors. Fatty and meat-rich food, especially the consumption of red meat (pork, beef, etc.) is a risk factor.
Read about how best to eat if you are sick: Diet in cancer
It is believed that the low-fiber diet leads to a longer intestinal passage and that various carcinogenic substances in the food have a greater harmful effect on the mucous membrane due to the longer contact time.
Eating fish, on the other hand, reduces the risk of cancer. Excessive calorie intake, obesity and lack of exercise, as well as nicotine and alcohol consumption, are among the cancer-promoting factors.
After many years of ulcerative colitis (chronic inflammatory bowel disease), the constant inflammation of the intestinal mucosa increases the risk of colon cancer by a factor of five.
In the case of the other chronic inflammatory bowel disease, Crohn's disease, the risk of developing colon cancer is only slightly increased.
Further information on this topic can also be found at: Crohn's disease
In rare cases, colon cancer can be inherited. In familial polyposis coli (FAP), the loss of a gene results in hundreds to thousands of polyps in the large intestine, which very often degenerate over time.
Approx. 1% of colon cancers are caused by the FAP. This genetic disease can lead to colon cancer at a young age, so that, depending on the findings, a prophylactic total colon removal (colectomy) is recommended at a very young age.
Read more on the topic: Colon cancer and removal of the colon
Hereditary non-polypous colorectal carcinoma (HNPCC) is not only the cause of colon carcinoma, but also of other tumors such as ovarian cancer, breast cancer, and uterine cancer. This disease can develop colon cancer before the age of 45, which does not arise from polyps. These carcinomas are responsible for about 5-10% of colon cancer.
Further information on this topic can also be found at:
- Ovarian cancer
- Breast cancer
In the case of inherited colon cancer, relatives should be given genetic counseling and intensive cancer screening should take place.
Some other rare syndromes are also associated with an increased risk of colon cancer, like this
- Gardner Syndrome
- Peutz-Jeghers Syndrome, Turcot Syndrome and
- the juvenile familial polyposis.
Read more on the subject at: What are the causes of colon cancer?
Risk factors for colon cancer
Colon cancer is the third most common cancer in men and the second most common cancer in women (in Germany). People over 40 have a significantly higher risk than younger people. Overweight people and people who consume alcohol and cigarettes also have a significantly higher risk. With regard to nutrition, it has long been known that foods rich in fiber and vegetables have a protective effect and foods rich in meat and fat increase the risk.
In addition to the genetic factors, risk connections to other diseases have been found: glandular tumors (colorectal adenomas), chronic inflammatory diseases (Crohn's disease, ulcerative colitis), type II diabetes mellitus and other malignant diseases such as breast, stomach and ovarian cancer.
Tumor spread (metastasis)

Different forms of metastasis can be described:
- Tumor spread via the lymphatic system (lymphogenic metastasis)
The lymph vessels drain the Lymph fluid (Intercellular fluid) from all parts of our body and thus also from colon cancer.
If the tumor gains a connection to a lymphatic vessel as a result of its growth, it can happen that some tumor cells become detached from the tumor cell cluster and are carried away with the lymph flow.
There are numerous lymph nodes in the course of a lymphatic vessel. In them is the seat of the immune defense, which has the task of catching and fighting germs (bacteria). The tumor cells settle in the nearest lymph nodes and multiply again.
This is how a Lymph node metastasis. Colon cancer particularly affects lymph nodes that lie in the course of an artery supplying the intestine, so that it is advisable to remove the blood vessels and lymph nodes during the operation.
- Tumor spread through the bloodstream (hematogenous metastasis)
If the tumor becomes attached to a blood vessel as it grows, cells here too can tear themselves loose and spread throughout the body via the bloodstream.
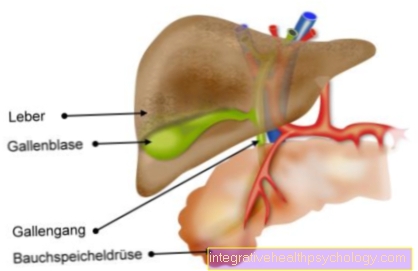
As the first station, the blood flows through the Liver (liver metastases)where the carcinoma cells can settle and form daughter ulcers (distant metastases). Deep-seated rectal carcinomas also have connection to vessels that bypass the liver through the inferior vena cava (Vena cava) lead to the heart.
The next organ in which tumor cells can settle and form distant metastases is then the Lung (lung metastases). In the further course of the disease, cells can become detached from the liver metastases and spread further into the lungs.
- Tumor spread through local growth (Per continuitatem)
The tumor can grow into other neighboring organs as it spreads. For example, rectal cancer in particular can be found in:- the bladder (Vesica)
- the uterus (Uterus)
- the ovaries (ovaries)
- the prostate
- into other loops of the large and small intestines
grow into (infiltrate).
Metastases
Almost every tumor can spread to other regions via the blood and lymphatic system. This leads to the fact that tumor cells settle in a place away from the seat of the actual tumor. This process is known as metastasis.
Colon cancer can also spread in a number of ways. It can metastasize to various lymph node regions via the lymphatic system or lead to tumor cell settlements via the bloodstream, especially in the liver and lungs.
Therefore, when making the diagnosis of colon cancer, an X-ray of the thorax to detect any lung metastases and an ultrasound or computer tomography of the upper abdomen to detect any liver metastases must always be carried out. Depending on whether it is a single (isolated) metastasis or numerous (multiple) metastases, removal can be sought or only a palliative (not healing-oriented but mainly symptom-relieving) therapy is used.
Staging
The diagnosis (see diagnosis and therapy of colon cancer) determines the tumor stage, which is decisive for further therapy planning.
However, an exact assessment of the tumor stage is often only possible after the operation, when the tumor has been removed and the surgical specimen (resected material) and the lymph nodes have been examined (histologically) using a microscope.
- Stage 0:
This is a so-called carcinoma in situ, in which only the top layer of the mucous membrane (mucosa) shows cancer cell changes. - Stage I:
At this stage, the tumor also affects the second layer of the mucous membrane (tela submucosa) Ia and the muscle layer (tunica muscularis) Ib. - Stage II:
The tumor has reached the last layer of the intestinal wall (subserosa). No lymph nodes are affected. - Stage III:
The cancer cells have infiltrated the lymph nodes. - Stage IV:
Daughter tumors (metastases) have formed in other parts of the body.
Also read:
- Stages of colon cancer and their prognosis
- The course of colon cancer
- End-stage colon cancer
Blood counts in colon cancer
Colon cancer is a disease that cannot be detected in the blood per se. There are some non-specific blood values that could be changed. For example, the non-specific inflammation value CRP or the laboratory value, which stands for cell breakdown, the lactate dehydrogenase LDH. In the case of chronic bleeding from the tumor, signs of anemia could be detectable (anemia of chronic disease): drop in hemoglobin, decreased erythrocyte count and iron values. Tumor markers can be measured to observe the progression of whether the cancer is regressing or coming back, especially the CEA (carcino-embryonic antigen).
Read more on the topic: Can you detect colon cancer in the blood?
forecast
The prognosis of colon cancer depends heavily on the tumor stage. In stage I (according to UICC) the 5-year survival rate is around 95%, in stage II up to 90%, in stage III up to 65% and in stage IV around 5%.
Read more on the subject at: Is Colon Cancer Curable?
Life expectancy
In principle, with every cancer disease, it is not curable, but treatable and that with sometimes more and sometimes less success. Colon cancer is one of the cancers that can be treated very well in the early stages, so that no spread (metastasis) or recurrence of the cancer (relapse) are to be expected. Even then, one should not speak of a cure, but rather correctly of a "very good prognosis". The prognosis is a doctor's prediction about the further course of the disease. These are always empirical estimates and statistical probabilities.
For the assessment, the present cancer is assigned to the defined TNM stages. It examines how far the tumor has grown (T), whether lymph nodes are affected (N) and whether it has spread (M). In general, the fewer infected lymph nodes and foci, the better the prognosis. The size of the tumor is actually rather irrelevant; the layers of the intestine that it has broken through are more important. In terms of therapy options, the complete surgical removal of the tumor is therefore of the greatest importance.
Furthermore, radiation and chemotherapy are important treatment measures. For example, a smaller tumor that did not affect the lymph nodes or otherwise spread, that has spread to the muscular layer of the intestine (T2), has 5-year survival rates over 90% (stage I). From the point in time when more than two foci are in organs other than the intestine, the probability is less than 5%, regardless of the size of the tumor or the number of affected lymph nodes. The prognoses range between this “best” and “worst case” depending on the precise diagnosis. After the initial treatment of colon cancer, follow-up care is of particular importance because, like general preventive care, it tries to discover tumors in small and therefore operable stages.
Read more on the subject at: Life expectancy in colon cancer
therapy
Colon cancer is divided into stages. Therapy then depends on which stage the tumor belongs to.
Colon cancer therapy almost always involves surgical removal of the tumor or at least the largest possible portion. Depending on the location of the tumor, there are numerous different types of resection (ways of removing the tumor). A distinction is made between a resection of the left, right or middle part of the large intestine and removal of the sigmoid colon.
Tumors in the rectum area can be removed in a continence-preserving or non-continence-preserving manner. This depends on their position in relation to the anal sphincter muscle (sphincter).
Depending on the type of resection, the subsequent reconstruction procedures also differ. When removing the left, right or middle part of the colon, the parts of the bowel are usually joined together before and after the resection (Anastomosis). In the case of resections in the rectum, the reconstructions are sometimes more complicated. In addition to the affected section of the intestine, the associated lymph nodes are also removed, as the tumor may have spread here.
Depending on the tumor stage, chemotherapy and radiation (Radiotherapy) before and / or after surgical resection. In the case of colon cancer, which is primarily no longer categorized as curatively treatable (in which a cure is not expected), removal of tumor parts can be useful, among other things, in order to allow food to pass through the intestines as far as possible and also to reduce symptoms such as pain . In palliative therapy (i.e. a therapy that, due to the tumor stage, does not aim to cure but primarily to alleviate symptoms), chemotherapy and newer therapeutic methods such as antibody therapy are used. Read more on the subject at: Chemotherapy for colon cancer
Follow-up care after the treatment of colon cancer must - especially at the beginning - be carried out at close intervals as the tumor can recur (Relapse) occurs approximately 70% in the first two years after resection. Follow-up examinations include ultrasound of the liver, colonoscopy, chest x-ray and laboratory to determine tumor markers. The tumor markers usually drop significantly after a successful resection, so a marked increase can be an indication of a relapse.
Read more on the subject at: Antibody Therapy (Anka)
Artificial exit
An artificial anus is also called anus praeter, stoma or enterostoma in technical terms. Its purpose is to divert stool directly through the abdominal wall and not, as in healthy people, through the rectum and anus. For this purpose, the (mostly) large intestine is detached from its holding structures in the abdomen and sewn to the abdominal skin in an operation. Then it is incised and opened so that the intestinal contents can drain into an external bag. The bag can then be emptied or changed into the toilet by the patient himself.
An artificial anus can be a permanent or temporary solution to a bowel passage problem. A permanent ostomy occurs, for example, if the sphincter had to be removed in the case of deep-seated colon cancer. A temporary stoma is used when a continence-preserving therapy for colon cancer is desired (e.g. by means of radiation). The artificial anus is also used for other intestinal diseases (e.g. chronic inflammatory bowel diseases such as Crohn's disease or ulcerative colitis).
Read more on the subject at: Anus praeter- the artificial anus
Colon cancer screening

The health insurances cover two screening colonoscopies every 10 years for men and women from the age of 55. In view of the fact that the incidence (occurrence) of colon cancer increases significantly from the age of 50, a preventive colonoscopy should be viewed critically at the age of 55.
In the preventive colonoscopy, the entire large intestine is observed using a tube to which a camera is attached. To do this, the tube is inserted from the rectum. The patient must have drunk several liters of a laxative solution the day before so that the bowel is as empty, clean and easily visible as possible.
During the examination, the patient is usually sedated and a short anesthetic is used. If noticeable protrusions of the mucous membrane (Adenomas) are found, these are usually removed during the examination using a small loop. You will then be processed histologically to determine whether it is a preform or an already manifest form of colon cancer and whether the adenoma has been removed with sufficient distance so that there is no longer any diseased tissue in the affected section of the intestine.
If the screening colonoscopy was normal, another one can be used after 10 years. If an adenoma has been removed, the time until the next mirroring depends on whether the adenoma could be resected with a sufficient safety margin. The next colonoscopy follows after 3 months (complete resection of all diseased tissue not certain) or 3 years (complete resection of the andenome).
Read more on the topic: Colon cancer screening
How common is colon cancer hereditary?
Exact percentages of how high your own risk of developing colon cancer is cannot actually be calculated per se. However, you can use the general risk factors to estimate your risk and, in comparison to your own age group, classify whether you have a higher or lower risk. Among the genetic risk factors, as with all cancers, it goes without saying that it is a disadvantage if a first- or second-degree relative is already ill.
It is also important to check the presence of two notable syndromes: familial polyposis syndrome (FAP) and HNPCC syndrome (hereditary non-polyposis colon cancer). The latter is the most common hereditary form of colon cancer and accounts for 5% of all colon cancers. Three quarters of those affected with this genetic abnormality (mutation) get colon cancer. The less common FAP, on the other hand, has a 100 percent chance of developing colon cancer. If you have frequent colon cancer cases, you should find out about genetic testing to find out whether it is possibly a genetic disease.
Read more on the topic: Is Colon Cancer Hereditary?
Further information
Further information on colorectal cancer can be found at the link:
- Colon cancer symptoms
- Colon cancer metastases
- Diagnosis and therapy of colon cancer
- Colon cancer screening
- Colon cancer pain
- Detect colon cancer
- Metastases
- Appendix cancer
Other interesting topics are:
- Minimally Invasive Surgery
- Inguinal hernia
- Excessive sweating
- Diverticulitis
- Crohn's disease
- Throat cancer
- Remove colon
- Tumor in the abdomen - that is part of it!
- Water in the stomach
- Genetic test
All topics that have been published on the field of internal medicine can be found at:
- Internal medicine A-Z








.jpg)