Liver abscess
introduction
In the case of liver abscesses, a distinction is made between a primary and a secondary course. The primary course of the liver abscess is caused by bacterial colonization via the gall bladder and bile ducts. The cause are either gallstones or parasites. Secondary forms of the liver abscess usually begin after operations or accidents, but also as a result of chronic tonsillitis, endocarditis, umbilical vein sepsis, late effects of diverticulitis, appendicitis, Crohn's disease and ulcerative colitis. The pathogens of a liver abscess are E.coli, Enterococci, Klebsiella or Bacteroides. Most often the right lobe of the liver is affected by an abscess, the left far less often. 60% have single abscesses, 40% have several smaller abscesses.
For more information on the subject of liver abscess, see the main article Abscess.

Letil line in a liver abscess
There is a guideline for the therapy of an amoebic liver abscess which lists how the diagnosis and treatment of this disease can be carried out adequately. The doctor can use the guideline as a guide, but is not obliged to follow it.
The amoebic liver abscess is caused by a pathogen called "Entamoeba histolytica". The abscess can develop into a life-threatening clinical picture as it can cause serious complications (for example, breakthrough into the free abdominal cavity). Well thought-out diagnostics and therapy are therefore crucial for the patient's recovery. Overall, every patient with a liver abscess must be treated as an inpatient in the hospital.
Diagnostics according to the guideline:
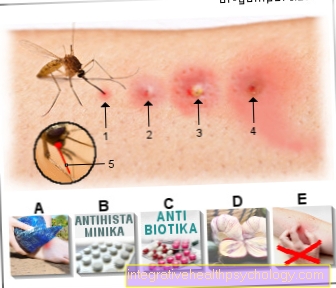
Every patient who has been in the tropics or subtropics in the last few years before the onset of the disease and who now suffers from fever, chest / abdominal pain and increased inflammation should be examined for a liver abscess.
The same applies to any patient with a fever after a stay in the tropics or subtropics who are tested for other tropical diseases (for example Malaria) are negative. The diagnosis is made on the basis of the patient's clinical symptoms, their inflammation levels and finally the detection of a mass in the liver on ultrasound. The diagnosis is confirmed by the detection of certain antibodies in the blood that are directed against the pathogen Entamoeba histolytica Act.
Computed tomography (CT) or magnetic resonance imaging (MRI of the liver) to assess the abscess in the liver. In this case you would do an MRI of the liver. A puncture of the abscess for direct detection of the pathogen is not always necessary.
Read more on the subject under: MRI of the liver
Therapy according to the guideline:
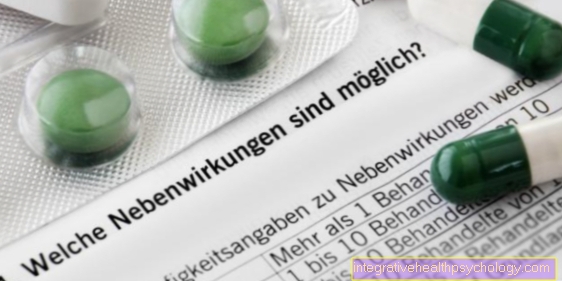
Drug therapy with metronidazole is recommended for the treatment of amebic liver abscess. This is an antibiotic that works well against the pathogen. It should first be given through the vein. In order to reach any remaining pathogens in the intestine, therapy with another drug, paromomycin, is advisable. Since other pathogens, for example bacterial pathogens, may also come into question before the final diagnosis, further antibiotics should first be given that also cover these other pathogens. Ceftriaxone, for example, is suitable for this purpose.
Monitoring according to guideline:
The patient's condition should be monitored during therapy. This includes regular blood counts, ultrasound control of the abscess, as well as stool samples in which no pathogen should be detectable after therapy with paromomycin. The general clinical condition of the patient should also improve noticeably soon after starting therapy.
Causes of a Liver Abscess
In most cases, liver abscesses do not occur alone, but are the result of inflammation in another organ. These liver abscesses are called secondary liver abscesses. One reason for this can be an inflammation of the bile duct (cholangitis), which spreads to the liver and then leads to an abscess there. Another way pathogens can get into the liver and lead to an abscess is through the bloodstream. Pathogens are mostly bacteria, but fungi and parasites are also possible. In primary liver abscesses, the cause lies directly in the liver. Parasites, such as the fox tapeworm or the dog tapeworm, attack the liver directly and lead to abscesses there. However, these are transmitted from animals and are rarely the cause. Another pathogen is the amoeba Entamoeba histolytica. It leads to amebiasis, which is only common in the subtropics and tropics. In some forms of the disease, the liver can be affected. In addition, inflammation from the gallbladder or bile duct can spread to the liver and form liver abscesses there. This is the most common cause. Injury to the liver from an accident is also a possible cause.
Read more about the topic here: Diagnosis of gallbladder inflammation
Liver abscess after biliary surgery
Due to the tightness of the gallbladder to the liver, it can easily be injured. This injury can become inflamed and lead to the formation of an abscess. However, an infection after biliary surgery is also possible through other causes, which leads to liver abscesses. Another possibility is e.g. B. a leaky bile duct after the operation, because the bile duct was injured, a bile duct fistula (an extra duct into the abdominal cavity) forms after the operation or the blind end of the bile duct was not tightly closed.
Symptoms of a liver abscess
Chills and fever, increased inflammation in the laboratory, tenderness in the right abdomen. Nausea, vomiting, and diarrhea can also occur. In some cases, the skin turns yellow (Jaundice) and anemia (anemia).
Therapy for a liver abscess

Since the liver abscess can be triggered by different pathogens, the therapeutic measures differ depending on the type of abscess. Accordingly, therapy can only be planned once it is clear what triggered it. Differentiating, however, is not always easy. The combination of the patient's clinical symptoms, examination findings from sonography (ultrasound) and possibly an additional computed tomography, however, usually points in one direction.
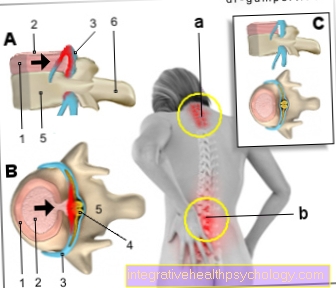
In some cases it can be assumed that it is a pyogenic (purulent) abscess caused by bacteria that have spread to the liver via the portal vein (vessels that lead to the liver), for example as part of appendicitis ( Appendicitis) or inflammation of the bile ducts (cholangitis). Then the following therapy scheme is followed: The abscess is punctured and drained. To do this, it is first determined with the help of an ultrasound of the liver at which point a puncture makes sense. This point is then marked on the skin. This is usually followed by a syringe with a local anesthetic (local anesthetic) to make the actual puncture as painless as possible. After a short period of exposure to the anesthetic, the skin (percutaneous) a fine needle is inserted to puncture the liver abscess. The contents of the abscess are then sucked out, so to speak (aspirated and drained). At the same time, antibiotic therapy is started - usually over several weeks - to eliminate the pathogen.
If the percutaneous puncture of the liver abscess is unsuccessful, a small operation is indicated in which a tube is inserted into the abscess cavity, which ensures that its contents can drain continuously. This is known as drainage. The antibiotic therapy should - if the pathogen is not already known and can be treated specifically - against aerobic and anaerobic bacteria Act.
The most common pathogens causing a pyogenic liver abscess are Escherichia coli (E. coli) or bacteria from the group of Klebsiae. A combination of an antibiotic from the group of cephalosporins (e.g. cefotaxime) or acylaminopenicillins (e.g. mezlocillin) in combination with metronidazole is often used for antibiotic treatment.
A second form of liver abscess is caused by amoeba (Entamoeba histolytica) triggered. As a rule, there is no puncture and drainage of the abscess, but only antibiotic treatment with metronidazole for about ten days. Regardless of the type of abscess, the patient should continue to be observed after starting therapy. Persistence of symptoms such as repeatedly (intermittently) occurring fever, malaise, and right-sided upper abdominal pain suggest that the therapy is not working. Sonographic controls can also give a rough indication of whether the therapy is helping, as can repeated blood samples for laboratory control.
The therapy of the liver abscess depends on the particular pathogen that triggered the disease. In general, the disease is initially treated conservatively, i.e. with medication. Surgical removal of the abscess is only resorted to when conservative measures are insufficient.
Read more on this topic at: Abscess treatment
Conservative therapy
Liver abscesses caused by Amoeba are classically with the antibiotic Metronidazole treated. Therapy is initially carried out via the vein of the patient. The dosage is included 3x10mg per day and kilogram of body weight of the patient and extends over 10 days. The maximum dose is included 3x800mg per day.
However, since metronidazole does not work sufficiently against the pathogens that are ultimately still in the intestine, the antibiotic is then used Paromomycin treated. The dosage is included 3x500mg per day for 9-10 days. Liver abscesses caused by other pathogens, for example Enterobacteria, are also treated with antibiotics. Metronidazole is also often effective here, in addition it can Ceftriaxone can be used.
In addition to the medication, the abscess cavity can also dotted become. In the case of amoebic abscesses this is only done in exceptional cases, and regularly in the case of bacterial abscesses. This is done by the liver abscess pierced through the skin and emptied through a hose and rinsed.
Operative therapy
Are the conservative measures not enoughIn order to get the disease under control, one needs an operative one Redevelopment of the abscess should be considered. This is also done more often when there are multiple foci of abscesses. The abscesses can either be removed individually as part of an operation, but one can also be Partial liver resection to be required. The affected part of the liver is completely removed. This is usually not a problem after the operation, as the liver - if there is sufficient residual tissue - can grow back to their original size.
diagnosis
In addition to the health survey on stays in the tropics (Parasites) or the presence of Gallstones The physical examination can confirm a suspected liver abscess. This is what otherwise cannot be felt liver palpable on physical examination (hepatomegaly) and painful knocking and tenderness. A Ultrasonic mostly reproduces a liver abscess quite reliably (so-called inhomogeneous foci). Furthermore, a fine needle aspiration can be performed for tissue collection and examination. An elevated diaphragm on an abdominal x-ray can sometimes be indicative of an enlarged liver due to one or more liver abscesses. A fine needle puncture can also CT can be carried out in a controlled manner.
Ultrasound for a liver abscess
Ultrasound is the standard examination if a liver abscess is suspected. However, the ultrasound is not always sufficient for a reliable diagnosis, which is why a CT must then be requested. On ultrasound, the liver abscess is darker than the rest of the tissue. Changes caused by parasites can also be detected with ultrasound.
CT for a liver abscess
As a rule, the ultrasound is the standard examination for making a diagnosis. However, if the ultrasound findings are not conclusive, a CT examination is requested. The CT is performed with the administration of contrast agent, since the liver abscess has a characteristic contrast agent absorption at the edge. Another feature is that the abscess is distinguished from the rest of the liver tissue by its darker appearance on the CT image. In this way, a reliable diagnosis can be made with the CT. With some parasites, the CT still shows parasite-specific characteristics, such as B. Cysts in dog tapeworm.
Puncture for a liver abscess
A liver puncture for tissue removal and examination does not play a role in the diagnosis of the liver abscess. But they are important in identifying the pathogen. It is unnecessary in the case of a liver abscess caused by parasites or amoeba. If bacteria are the cause of the liver abscess, the puncture makes sense. In this way the bacterium can be identified and a specifically effective antibiotic can be taken. However, a puncture also comes with a few risks.
Liver abscess prognosis
The mortality rate from multiple liver abscesses is 30%. As a complication, there is the risk of septic spread of the abscess pathogen (parasite or bacteria) if the abscess is perforated. In addition, impairment of liver function with potentially life-threatening consequences.
Streptococci
In most cases, bacteria are responsible for the liver abscess. The most common pathogens are the ecolibacterium (Eschericha coli) and the Klebsiella. These live naturally in the intestines. The streptococci are less often identified as the causative agent of a liver abscess. They occur naturally in the mouth.