Diabetes mellitus
Synonyms in a broader sense
Sugar, diabetes, adult diabetes, type I, type II, gestational diabetes
Literal translation: „honey flow“
English: diabetes
Definition of diabetes mellitus
Diabetes mellitus, popularly only called diabetes (Diabetes) is a chronic metabolic disease that can be traced back to an absolute or relative insulin deficiency.

The hallmark of this disease is permanent Excessive blood sugar levels (hyperglycaemia) and urine sugar. The cause is the inadequate effect of the hormone insulin to the Liver cells, muscle cells and Fat cells of the human body.
The disease diabetes mellitus is one of the most important diseases in the Internal medicine.
Diabetes mellitus is divided into type 1 and type 2 diabetes.
Type 1 diabetes mellitus

The beta cells of the pancreas are destroyed in type 1 diabetes mellitus and therefore inoperable, i.e. they no longer produce insulin.
The cell death, usually the number of cells is reduced to less than 10% of the actual cell stock, is caused by an autoimmune disease and leads to an absolute insulin deficiency.
Type 1 diabetes mellitus can occur at any age, but especially in children and adolescents, and makes up 5-7% of the total number of diabetics.
In 90% of the cases, the patients have certain genetic characteristics that give reason to believe that there is a hereditary predisposition to diabetes.
In 75% of the cases, three different islet cell autoantibodies (IAA, GADA, IA-A) can be detected in the patient's blood. These antibodies, which are produced by the body itself but are directed against the body's own structures (autoimmune disease), suggest sugar disease / diabetes. If two or all three islet cell antibodies are already present at the age of two, the child must be expected to become ill before the age of 10.
In the broadest sense, this is also a rheumatic disease such as rheumatoid arthritis
The age at which type 1 diabetes mellitus predominantly occurs ranges from 15 to 24 years of age. The patients are usually of normal weight and do not have a stable metabolic situation.
The onset of the disease, due to the absolute insulin deficiency, occurs quickly, when over 80% of the islet cells have been destroyed.
The first manifestation of the disease often occurs in stressful situations.
If a parent of a child has type 1 diabetes mellitus, there is a 2.5 - 5% risk that the child will also have diabetes. If, on the other hand, both parents are affected by the disease, the risk of the children getting the same is 20%.
Therapy of diabetes with insulin is absolutely necessary in type 1 diabetes, since the body's own production fails and the hormone is replaced, i.e. must be supplied from the outside.
More about type 1 diabetes mellitus
Type 2 diabetes mellitus

Patients with type 2 diabetes mellitus, also known as adult diabetes, have a relative lack of insulin.
There are two reasons for a disorder of the sugar metabolism: The insulin release (secretion) of the pancreas is disturbed or the effect that the insulin has on the organs is reduced. This is called insulin resistance, which is based on receptor defects (receptor = superficial recipient characteristic of the cell through which information, e.g. through a hormone, gets into the cell interior), or a disturbed signal transmission in the cell.
Most of the diseases of type 2 diabetes mellitus develop due to the metabolic syndrome (also called affluence disease):
Many diabetes patients often have the following 4 risk factors:
- Overweight with the majority of body fat on the stomach
- increased levels of fat and cholesterol in the blood (hyperlipidaemia / hypercholesterolaemia)
- High blood pressure (arterial hypertension)
- Glucose tolerance disorder (diabetes)
Malnutrition with obesity and lack of exercise are decisive factors in the development of type 2 diabetes mellitus. Overeating causes high insulin levels in the blood, as insulin is necessary to transport the glucose into the cells, where sugar is used and energy is generated. Read also Diabetes and Diet.
These high levels cause the cells to become less sensitive to insulin and the insulin receptors on the cells to decrease in number. As a result, the insulin effect is weakened. If the high food supply persists over a longer period of time, an ever larger amount of insulin is necessary to utilize the dietary carbohydrates due to less sensitive cells.
There is a relative insulin deficiency, i.e. the amount of insulin that is available is not enough to cover the sugar utilization and lower the blood sugar level. During this phase of the disease, “sugar tablets” (oral antidiabetic agents) can still be used.
After such years of stress on the insulin-producing cells, the insulin production can be exhausted and finally, due to an absolute insulin deficiency, insulin-dependent diabetes can occur, i.e. insulin must be supplied from outside. Oral antidiabetic drugs alone are no longer sufficiently effective in this phase of the disease.
The vicious circle of the increased need for insulin can be broken through sporting activity and a change in diet, because under these conditions the insulin level falls and thus the insulin sensitivity of the cells increases again.
Patients with type 2 diabetes mellitus are often overweight and mostly older than 40 years. The onset of the disease, which occurs slowly and insidiously, is often only noticed after a while, usually when high blood and urine sugar levels are found in a routine examination or long-term effects of diabetes (Diabetes) occur and lead to the diagnosis (e.g. polyneuropathy, diabetic nephropathy / retinopathy, etc.).
There are causal genetic components in this form of diabetes as well. The risk of developing type 2 diabetes mellitus is up to 50% for children who have one parent who is sick.
Therapy with insulin is not absolutely necessary, but it must be started when the insulin reserves are exhausted and a change in diet alone and treatment with oral antidiabetic drugs are no longer effective.
More about type 2 diabetes mellitus
Other forms of diabetes
- Maturity-onset Diabetes of the Young (MODY)
In this form of diabetes, there are genetic defects in the islet cell. The insulin release is restricted. In contrast to type 1 diabetics, when MODY no autoantibodies are detected in the patient's blood. There are 6 different subgroups of the type of diabetes, which are characterized by the defective gene.
This type of disease is present in around 1% of diabetics.
- chronic pancreatitis
Chronic inflammation of the pancreas (Pancreatitis) can cause diabetes.
More about this topic can be found: Inflammation of the pancreas
- Hormonal imbalances
Disorders of the hormonal balance in the form of e.g. one Glucagon producing tumor (glucagonoma) or hyperfunction of the thyroid (Hyperthyroidism) may be due to diabetes)
- Viral diseases
Viral diseases are related to the development of diabetes, e.g. a Rubella infection of the infant in the pregnancy or directly after the Birth.
- Gestational diabetes
Gestational diabetes is present when there is an increased blood sugar level for the first time during pregnancy. This form of diabetes occurs in 0.5-3% of pregnant women and is the most common metabolic disorder in the Pregnancy. After birth In the child, the mother's diabetes usually regresses, but there is a high risk of a later onset of type 2 diabetic disease.
It is possible that maternal diabetes may cause the child to grow tall (macrosomia) or that deformities may occur, and the infant mortality rate increases.
When a treatment with Diets alone is not enough, pregnant women can use a intensified insulin therapy or an insulin pump are supplied. Oral anti-diabetic drugs may not be administered because of their teratogenic effects. Therefore, diabetics with type 2 diabetes must be switched to insulin during pregnancy.
Every woman carries out a 50 gram glucose screening test as part of her preventive check-ups during pregnancy, so that gestational diabetes can be detected early and complications for the child and mother can be avoided.
Causes and development of diabetes mellitus
The decisive hormone in the regulation of blood sugar levels is insulin. Much of that ingested through food carbohydrates contains glucose (sugar). This sugar is an important supplier of energy for the human body and is transferred into the blood via the gastrointestinal tract after it has been absorbed. From here, under the action of insulin, it enters the cells:
The Pancreas (Pancreas) releases insulin into the bloodstream after a high-carbohydrate meal to enable the sugar to be used. The hormone makes the cell walls permeable to sugar, so that the cells are adequately supplied with nutrients and the sugar level in the blood drops. Thus, insulin is an important control factor for the mobilization and storage of glucose (sugar).
Insulin is also used for fat and protein metabolism anabolic hormone a meaning because it causes the building of Adipose tissuei.e. of energy storage for the body, as well as the formation of protein and the Sugar storage substance glycogen in the liver and in Muscle tissue.
The cells in the pancreas that produce insulin are called Beta cells, islet cells or Langerhans'sche Islands after its discoverer Paul Langerhans.
Symptoms / how do I recognize diabetes?
The first signs of diabetes are frequent urination and severe thirst, and can often lead to unexplained weight loss and persistent tiredness and fatigue. In babies and children, it is usually type 1 diabetes that occurs and manifests itself, among other things, through frequent urination and very strong thirst, as well as tiredness and fatigue. Diabetes can develop during pregnancy, but this does not show itself through the typical signs.
Read more on the topic: How do I recognize diabetes?
Read more on the topic: Diabetes in Children
Frequency (epidemiology)
Diabetes mellitus Occurrence in the population
7-8% of the adult German population have diabetes mellitus, of which 95% of these people at one Type 2 diabetes are sick.
course
For the course of diabetes it is crucial that a careful blood sugar control is guaranteed for life, because this is the only way to prevent long-term damage.
The disease is particularly stressful for the blood vessels, which is why a heart attack (myocardial infarction), a coronary artery disease (coronary heart disease (CHD), angina pectoris) or a stroke (apoplexy) can occur due to vasoconstriction or vascular occlusions in the arm and leg arteries (PAD) can lead to a limitation of the patient's mobility.
Disturbances in the kidney supply (diabetic nephropathy) or the blood flow to the retina of the eye (diabetic retinopathy) are further possible consequences of diabetes. Diabetes-related damage to the distant body nerves leads to the clinical picture of diabetic polyneuropathy.
You might also be interested in this article: Macular edema
In order to avoid or delay potential organ damage, various diagnostic measures are carried out to monitor the progress of diabetes. This includes regular blood sugar checks by the family doctor and independent self-control by the patient.
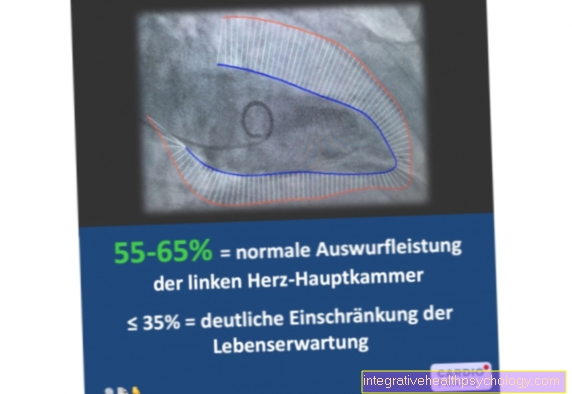
A very reliable and extensive diagnostic tool is the HbA1c determination. The HbA1c value indicates the percentage of glycosylated hemoglobin in the total hemoglobin (red blood pigment). The normal value for healthy people is 4 - 6.2%, for diabetes therapy a value below 7% is aimed for, optimally it is below 6.5%.
Glycosylated red blood pigment is produced when glucose, which cannot be transported into the cells due to the lack of insulin, attaches to the red blood cells. The extent of this build-up reflects the blood sugar control over the past 6-8 weeks. In this respect, the HbA1c value can also be referred to as the sugar memory.
The test for microalbuminuria (explanation see “Complications”) is carried out once a year for every diabetic. Here, the urine is examined for the smallest amount of protein in a urine examination, as this indicates damage to the kidneys by diabetes at an early and treatable stage.
Regular visits to the family doctor (family doctor or doctor for internal medicine = internist) and ophthalmological checks (ophthalmology) to assess the course of the disease are recommended for diabetes patients in view of the possible long-term consequences (e.g. blindness, heart attack).
prophylaxis
There are no preventive measures to avoid type 1 diabetes.
Type 2 diabetes, however, can be prevented if the biggest risk factor is that Obesity, is eliminated early. To do this are healthy and balanced nutrition as well as regular sport activity necessary. It is important that these measures are carried out permanently and not become a compulsion.
Exercise is beneficial for preventing diabetes, as less insulin is released during physical exercise. The cells need less insulin to take up glucose (sugar), so that the risk of insulin resistance and excess insulin release as with type 2 is low.
forecast
The forecast for the diabetic, the extent of the vascular damage is decisively determined. Almost 80% of the causes of death in people with diabetes can be traced back to vascular diseases.
In order to keep the risk of diabetic vascular damage as low as possible, the diabetic should consistently and permanently aim for a normal high blood sugar level. Here are the blood sugar self-controls as well as the medical therapy with oral antidiabetic drugs or insulin important aspects.
Of the Type 1 diabetic often suffers damage to the small vessels after a long period of illness. These changes in the vessels of the kidneys are particularly critical: The main cause of death in these patients are chronic damage to the kidney.
At the Type 2 diabetic on the other hand, the course of the disease is decisively influenced by the damage to the large body vessels. Heart attack (myocardial infarction) or stroke (Apoplexy) are common causes of death.
The prognosis of type 2 diabetics can, since Overweight (Obesity) a common cause of illness is significantly (significantly) improved by timely weight reduction with appropriate diet and physical activity.