The function of the liver
Synonyms
Medical: hepar
Liver lobes, liver cells, liver cancer, liver cirrhosis, fatty liver
English: liver
definition
The liver is the central metabolic organ in humans. Their tasks include the food-dependent storage, conversion and release of sugars and fats, the breakdown and elimination of endogenous and medicinal toxins, the formation of most blood proteins and bile, and numerous other tasks.
Function of the liver
Metabolic performance of the liver cells
The liver performs many metabolic functions. The main services are listed below.
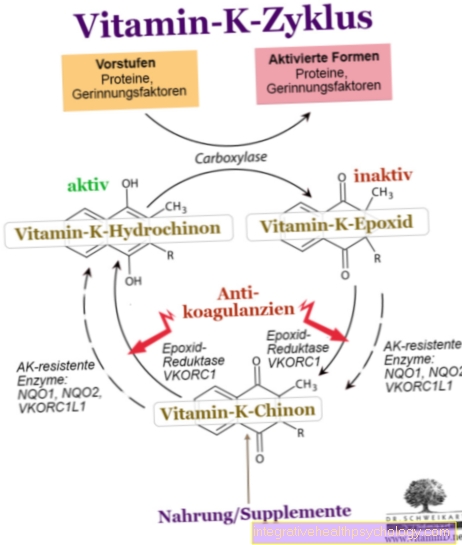
Production of blood proteins
There is a multitude of proteins (plasma proteins) in the blood, each of which has a very specific function. Except for one class of blood proteins, namely the antibodies (gamma globulins) of the immune system (defense system), all the others are produced by the liver and released into the blood.
These include the Egg whites for the Blood clotting (clotting factors), for the Defense system (Complement system), for transport and many other functions. With the help of a special examination of these proteins, called electrophoresis, you can see something about the production capacity of the liver.
As part of an acute inflammation in the body, the liver can change its production a little. It then increasingly forms the so-called acute phase proteins (C-reactive protein (CRP value), Haptoglobin, and others) that help fight inflammation.
They also lead to an increase in Erythrocyte sedimentation rate (ESR), a simple test as part of medical diagnostics.
Production of hormones
The liver make some Hormones. It is involved in the body's own production of Vitamin D3. This is a hormone that is necessary for the regulation of the Calcium balance.
Furthermore, it educates IGF-1, a hormone that accelerates growth and muscle building and even as part of sports doping (Doping, anabolic steroids) is used. Another important hormone (more precisely, a precursor) is angiotensinogen.
This is directly involved in the regulation of blood pressure and fluid balance. Be against this hormone high blood pressure Prescribed drugs called ACE inhibitors.
Carbohydrate metabolism
The carbohydrate metabolism is also known colloquially as the sugar metabolism. Some cells in the body, especially the red blood cells and the nerve cells, are on the continuous supply with Blood sugar Since humans take in their food at intervals with their few daily meals, they need a system with which they can store the increased concentrations of nutrients after eating and release them again between meals if necessary. This is essentially the job of the liver.
After eating, the liver is fed by the hormone insulin stimulated the increased concentration of blood sugar in particular Form (glycogen) save. In total, up to 10% of the total weight of the liver, i.e. approx. 150 g, can be stored in this form as sugar in the liver. If the blood sugar starts to drop between meals, the liver starts up under the influence of the hormone Glucagon, the breakdown of stored sugar.
This is released into the blood in the service of the body. However, without food, the liver's sugar stores only last for less than a day. Therefore, the liver can also produce sugar from proteins. The proteins are primarily obtained through the breakdown of protein in muscle cells.
Some rare, always genetic diseases affect this function of the liver. Individual proteins (enzymes) that are necessary for the release of sugar into the blood are missing. In these cases the patient can eat normally and fill his stores. But at the moment when the body relies on the release of sugar into the blood, the defect becomes noticeable and the patient hypoglycens. The therapy is careful diet with regular, small meals.
Fat metabolism
The liver is also for that Metabolism (processing) of fats essential for survival. Fats that the body can use are not soluble in the blood. The liver therefore produces special fat transporters, the lipoproteins.
If the liver has enough nutrients and energy available, it is able to produce fats (fatty acids) from sugars and proteins. These are specially packaged (in VLDL lipoproteins) and then transported with the blood towards the fatty tissue. In adipose tissue, the fats are then stored in the fat cells. If there is now a lack of energy, the fats in the fat cells are broken down again and transported back to the liver, where they are used to generate energy.
Storage of substances
The liver is able to store numerous vital substances and to release them again when necessary.These include the Vitamins A, B12, D, E and folic acid as well as the metals Iron and copper. Diseases are described for both metals in which, due to a genetic defect, the pathological storage of these metals occurs and which can thus lead to liver damage or even liver cirrhosis (Wilson's disease, hemosiderosis).
Detoxification (biotransformation)
The liver is the body's organ that is particularly capable of breaking down toxins. Like a sewage treatment plant, all substances in food have to pass through the liver before they enter the general bloodstream. But not only nutrients, the body's own metabolic products can also become toxic. They are also converted into less toxic substances in the liver.
alcohol, which is a strong cell poison, is almost exclusively broken down in the liver (detoxification). The alcohol is chemically modified via special proteins (enzymes) in such a way that it is no longer harmful but, on the contrary, useful. At the end of the alcohol breakdown, a substance is created that supplies energy directly.
Before you get this fact wrong, you have to consider even more: The liver does not manage to break down all the alcohol on the first passage; thus the poison reaches all cells of the body via the bloodstream.
Furthermore, alcohol is also toxic to the liver cells themselves; liver cells die off here. In addition, the breakdown of alcohol produces so much energy that the liver can no longer keep up with consuming it. It then stores the energy in the form of fat. If too much of this fat builds up, it creates one Fatty liver (steatosis hepatis); the preliminary stage of cirrhosis of the liver.
For Medication The same principle applies: When they flow through the liver, the substances are chemically changed so much by special proteins that they lose their effect (first-pass effect). In drug therapy, this effect is always taken into account when choosing the dosage. This can be so severe that some drugs cannot be given in tablet form. In rare cases, however, these processes produce more toxic substances.
An important example is the combination of alcohol and Paracetamol (Painkiller)which can lead to the formation of a carcinogenic substance.
A detoxification reaction of the liver that is particularly important for a medical diagnosis is the remodeling of Bilirubin. Bilirubin is produced wherever red blood cells are broken down or perish. In both cases, this toxic bilirubin, known as unconjugated or indirect, binds to a special protein in the blood called albumin.
When this complex of protein and bilirubin finally reaches the liver, this bilirubin is detached from its transport protein and converted in the liver cells so that it becomes non-toxic. After its remodeling, it is called direct or conjugated. The doctor can use the ratio of direct and indirect bilirubin to determine where damage may be present.
Another important detoxification reaction of the liver is the formation of urea. Urea contains ammonia, a substance from the protein metabolism that in its natural form is brain harms, in its connection as urea, however, is non-toxic. In this way, the body can simply excrete the previously toxic ammonia in the urine (hence the name).
Bile
The liver is the producer of the bile (up to 1 liter / day). Bile is a mixed liquid made up of fat (cholesterol), Bile acids, bile pigments, bile salts and other substances. It serves both to excrete substances that are no longer required, possibly toxic, and to support the digestion of high-fat food. Cholesterol is the main component of bile. Although it can be produced by the body, it cannot be broken down again, which is why it is necessary to excrete it. Cholesterol can either be excreted as bile acid (the majority) coupled to various amino acids (building blocks of proteins), or as cholesterol itself.
Bile pigments are mainly the breakdown substances of the red blood cells. They are processed again by the liver.
The bile is released when it is eaten Gallbladder saved.
The liver mainly contains substances that can be dissolved little or not at all in water, but in fat (lipophilic substances). This can be explained by the fact that only water-soluble substances can get into the urine.
The body uses this increased occurrence of fat-soluble substances in the bile Digestion of high fat food. The gallbladder is connected to the small intestine via the bile duct. in the Small intestine the bile mixes with the digestive substances of the pancreas (Pancreas) and the food pulp. The bile dissolves (emulsifies) the fatty parts of the food in order to enable the digestive proteins of the pancreas to work.
Formation of lipoproteins
Lipoproteins belong to the blood proteins. All but one of them are produced in the liver. and act as transporters for fatty acids and cholesterol in the blood, which due to their chemical nature could not otherwise be found in the blood. There are four different classes of lipoproteins: chylomicrons (the exception that is not made in the liver), VLDL, LDL and HDL:
Chylomicrons are formed in the intestine. Their job is to transport the fats freshly taken in from food via the lymphatic system into the blood and then into the consuming tissues. Adipose tissue and muscles. There are special proteins (lipoprotein lipase) that split the fats into their individual components and thus enable them to be absorbed by the target cells. The remains of the fat transporter are processed in the liver.
The VLDL are made in the liver. Their task is to transport the fatty acids newly produced in the liver when there is excess energy into the body. Analogous to the chylomicrons, they too are broken down by proteins near their target cells and the fatty acids are absorbed into the cells.
LDL: These famous lipoproteins are especially Cholesterol transporters. They bring cholesterol from food and the liver to the rest of the body's cells. They are famous as "Bad" cholesterol because they cause the formation of Hardening of the arteries (Arteriosclerosis). The LDL is taken up as a whole in the target cells and only broken down in the cell.
HDL: This also as "Good" cholesterol known lipoprotein has the task of collecting cholesterol in the body and transporting it to the liver in order to excrete it in the bile. Therefore, a high concentration of HDL can dispose of excess cholesterol and thus the development of arteriosclerosis inhibit.