Inflammation of the spinal cord
introduction
An inflammation of the spinal cord (medical: myelitis) can have different causes and effects. The disease is one of the neurological diseases of immunological, allergic or idiopathic cause. Overall, it is a relatively rare neurological disease.
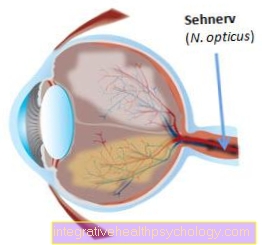
The spinal cord, together with the brain, is part of what is known as the central nervous system.

The spinal cord is responsible for forwarding all information that comes from the different parts of the body to the right places in the brain and, conversely, for correctly transmitting information that goes from the brain to the rest of the body. For this reason, inflammation in the spinal cord can cause a variety of symptoms, which depend on the location of the infection and which also vary greatly in course.
A classification of the different types of inflammation of the spinal cord is made on the one hand according to the type of inflammation and on the other - if it is an infectious myelitis - according to the different pathogens that are responsible for the inflammation. A disease can be described as inflammation of the spinal cord if it occurs either as part of an infectious disease, an allergic reaction, a neurological disease or also in isolation.
There are basically two different types of spinal cord inflammation:
- If the entire spinal cord is diffusely affected, it is called transverse myelitis
- If there are several foci that affect different sections of the spinal cord, this is called disseminated myelitis.
Spinal cord inflammation can develop acutely within a few hours or days as well as subacute (within a few weeks) and chronic (after 6 weeks).
Symptoms
The symptoms of spinal cord inflammation can be very diverse. The individual severity of the respective symptoms is mainly determined by the type of inflammation and the progression of the disease. The main difference in the respective symptoms is determined by the type of disease. So it depends on whether the person concerned is affected by a paraplegic or disseminated spinal cord inflammation. Since spinal cord inflammation is an inflammation of the central nervous system, functions are also affected that may not appear to be related to the spinal cord at first glance. The reason for this is that a number of processes in the body are regulated by nerves that run through the spinal cord. Inflammation in this area therefore often leads to deficits in regions that are possibly far from the spinal cord.
Overall, symptoms of the inflammation occur within 24 hours in most people.
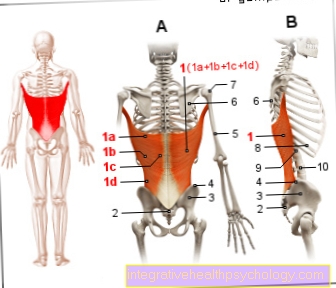
In transverse myelitis, the individual symptoms basically depend on the level of the spinal cord at which the inflammation is present. Symptoms frequently observed in spinal cord inflammation of the paraplegic myelitis type are muscle weakness or paralysis, sensory disturbances, depression, general weakness and disorders of the function of the bladder or rectum. Parasitic sensations or numbness in the legs and a pronounced feeling of weakness are also particularly common.
Similar symptoms occur in so-called disseminated spinal cord inflammation. The difference lies in the holistically affected spinal cord in the presence of disseminated inflammation. The symptoms can also be very serious and include severe paralysis, headache and neck pain, visual disturbances, epileptic seizures or vomiting.
The problem with the typical symptoms of spinal cord inflammation is that other diseases affecting the spinal cord, so-called myelopathies, also cause very similar symptoms and are therefore very difficult to differentiate from spinal cord inflammation by a clinical examination.
It is also worth mentioning that mostly flu-like symptoms can be closely related to the occurrence of the spinal cord inflammation. About 30% of those affected report weakness, fever, and body aches shortly before the diagnosis of spinal cord inflammation.
Are there any long-term consequences?
Depending on the type and cause, various long-term consequences can arise, and the location of the inflammation in the spinal cord is also decisive. In principle, all acute symptoms such as paralysis, pain or abnormal sensations can also become chronic, especially if the disease is not treated or cannot be adequately treated.
Nerve pain, in particular, is very agonizing for those affected when it becomes chronic, as normal painkillers do not respond and it can be difficult to find a suitable drug. If necessary, a pain therapist must also be called in here.
Physiotherapy and occupational therapy are also recommended for paralysis and abnormal sensations. Depending on the type and severity of the paralysis, this can of course lead to the inability to walk.
If long-term damage persists, it is often a great burden for those affected, so depression is another possible consequence.
Find out what's happening at Nerve pain is to be observed!
Diagnosis of inflammation in the spinal cord
Although acute inflammation of the spinal cord usually causes severe symptoms, it is difficult to make a purely clinical diagnosis by talking to the patient and by physical examination. This is because a number of neurological disorders affecting the central nervous system produce very similar symptoms.
Magnetic resonance imaging (MRI) is usually performed to get an overview of the disease and to be able to rule out certain diagnoses, such as a tumor of the spinal cord that causes similar symptoms.
MRI is an important diagnostic tool for inflammation of the spinal cord. It is an imaging process that, in contrast to X-rays and computed tomography, does not involve any radiation exposure. It can very well represent so-called “soft tissue”, i.e. organ structures, fats, spinal cord and inflammatory processes, but less bone structures. In order to achieve a better contrast of the image, contrast media can be used, which can either be injected, drunk or administered rectally via an enema.
The reason for the respective symptoms can now be searched for in the resulting images. Spinal cord inflammation, like other diseases of the spinal cord, has characteristic abnormalities that a radiologist can document in the MRI images if necessary.
If the doctor already has a specific suspected diagnosis, the MRI can be carried out directly in a special form. If the diagnosis of multiple sclerosis is suspected, a special MRI will be performed for V.a. multiple sclerosis.
However, the individual cause of the occurrence of the inflammation cannot be determined using the imaging tests. Certain laboratory values usually provide information about the reasons for the inflammation. With the help of a so-called lumbar puncture, a liquid (liquor) can be removed from the spinal cord and then examined. Certain changes in the CSF make it possible to determine whether an infection is present and whether it is more of a viral or bacterial origin.
Blood values can also be helpful in making an individual diagnosis, as this can rule out certain previous illnesses and specifically examine certain autoimmune diseases.
In many cases, however, it is not possible for the treating physician to identify the cause of the existing inflammation. In these cases a so-called idiopathic Spinal cord inflammation assumed (for no apparent reason).
For more information, read also: MRI of the back and MRI of the spine
causes
The causes of spinal cord inflammation can be very different. Most often, the inflammation occurs due to a specific infection. Infections with some viruses, but also bacteria, can be the reason for the development of such an inflammation. Some examples of viral pathogens that can cause inflammation of the spinal cord are: hepatitis C, HIV, herpes simplex or influenza. Inflammation of the spinal cord can also occur after certain vaccinations (e.g. smallpox vaccination).
Bacteria can also cause inflammation when the spinal cord is infected.
It is also believed that certain autoimmune diseases can be responsible for the occurrence of spinal cord inflammation. The reason for this is that instead of fighting off pathogens, the body's autoimmune cells turn against the body's own cells and cause inflammation there. Autoimmune diseases such as sarcoidosis, systemic lupus erythematosus (SLE), the so-called Sjogren's symptom or multiple sclerosis (MS) can be responsible for the occurrence of spinal cord inflammation. In the case of multiple sclerosis, it is also discussed that the occurrence of disseminated spinal cord inflammation can be an initial manifestation, i.e. the first sign of an emerging MS.
idiopathic inflammation of the spinal cord
The occurrence of idiopathic spinal cord inflammation, which cause the symptoms mentioned for no apparent reason, is also possible. Idiopathic means that no apparent reason can be established why such inflammation is occurring. This is the case if no cause can be found diagnostically which makes a plausible explanation for the inflammation appear.
Overall, it must be mentioned that the cause of a large part of the inflammation of the spinal cord remains unexplained even after the symptoms have subsided.
Spinal cord inflammation after vaccination?
Vaccinations are one of the greatest achievements of modern medicine and have already saved countless lives, so it is generally advisable to have the vaccinations recommended by the STIKO (permanent vaccination commission) carried out! After a vaccination there may be a so-called vaccination reaction with symptoms such as aching limbs and a slight fever, which disappear again after a short time. This is safe and even a good sign as it indicates the immune system's response to the vaccine. In extremely rare cases, some vaccinations can cause serious illnesses, an example of which is acute demyelinating encephalomyelitis, or ADEM for short. It is not yet certain how and whether ADEM is related to vaccinations, but it occurred now and then after vaccinations, but much more often after infections. ADEM is an autoimmune disease in which the myelin sheaths in the nerve cells of the brain and spinal cord are attacked and destroyed, which can lead to severe neurological damage. ADEM is often compared to MS, but in contrast to this, it always takes place with only one attack. Overall, the prognosis is good; in most cases the symptoms regress completely, but rarely permanent impairments can occur.
Inflammation from bacteria
Spinal cord inflammation is rarely caused by bacteria. It has not yet been finally clarified whether the bacteria themselves cause the inflammation in the spinal cord or whether the bacteria cause an autoimmune reaction in the immune system. This means that in addition to the pathogens, the cells of the immune system also falsely fight the spinal cord and thus cause the inflammation.
Bacterial pathogens that are known for such inflammations are the tuberculosis pathogens, Borrelia but also so-called mycoplasmas. These must be treated with special antibiotic therapies.
The earlier the infection is detected, the sooner a quick healing can be expected.
Virus inflammation
Viruses represent a second possibility of an infectious cause of the inflammation of the spinal cord. Viral pathogens are much more frequently responsible for this disease than bacteria. The typical viruses that are often behind it range from childhood viruses such as measles and mumps, to very common pathogens such as Herpes or Eppstein-Barr viruses, to rabies and HIV pathogens.
The subsequent therapy must be made dependent on the respective virus. Some of the viruses can be controlled, but there is no cure. These include the herpes viruses and HIV. Measles or the hepatitis virus, on the other hand, can often be completely eliminated by the body. Antiviral drugs can also help to accelerate healing and alleviate symptoms.
Inflammation of the spinal cord and MS
Multiple Sclerosis (MS) is a chronic inflammatory disease in which the nerve fiber sheaths of the central nervous system (brain and spinal cord) are progressively destroyed.
If such foci of inflammation occur in the spinal cord without the MS diagnosis being already known, they may well look like a separate spinal cord inflammation (Myelitis) impress and initially be misinterpreted.
According to this, symptoms of isolated myelitis can either be the early symptoms of a first flare-up of MS, but they can just as well represent a separate idiopathic spinal cord inflammation that is unrelated to multiple sclerosis.
CSF diagnostics are decisive for the diagnosis (oligoclonal bands) and additional, inflammatory foci in the brain tissue, which speaks for a multiple sclerosis flare-up.
Read more on the topic: Multiple sclerosis diagnosis
therapy
If spinal cord inflammation is diagnosed, therapy should be started immediately. Especially so-called corticosteroids, i.e. drugs that are anti-inflammatory, are the focus of therapy for acute spinal cord inflammation.
Depending on the cause of the inflammation of the spinal cord, other medications are added. For example, if there is a confirmed infectious cause, anti-viral drugs or antibiotics can be used in the case of a bacterial infection.
Another possibility, which is mainly used for inflammation in which it is suspected that an autoimmune reaction is responsible for the disease, is the so-called plasma exchange (plasmapheresis).
In this procedure, the blood plasma is separated from the remaining blood and fresh donor plasma is added. This procedure aims to filter out the defective cells of the immune system and thus treats the resulting inflammation.
Treat inflammation in the spinal cord with cortisone
The use of cortisone is advisable for almost all types of spinal cord inflammation. Glucocorticoids (e.g. cortisone) are actually the treatment of choice because spinal cord inflammation (Myelitis) is either due to an overactivity of the body's immune system, which is directed against the spinal cord, or a viral or bacterial infection.
The cortisone strongly inhibits the inflammation and suppresses the body's own immune system at the locally applied point (Immunosuppressive effect). It controls the cell metabolism of the inflammatory cells and in this way inhibits the inflammatory process.
In contrast to other anti-inflammatory drugs, cortisone works very quickly and very strongly. For example, if the inflammation is allergic, an intravenous application can have an effect in a few minutes.
The application with cortisone only has to be weighed up in the case of infectious causes of the spinal cord inflammation. If the inflammation is caused by an immediate pathogen-related infection, cortisone treatment can slow down healing, as the immune system loses the ability to fight the pathogen itself. In these cases, antibacterial or antiviral drugs are more preferable.
The glucocorticoids can either be administered intravenously, i.e. via the vein (often in severe acute cases) or orally as tablets.
In principle, cortisone treatment must not be forgotten that it is symptomatic therapy. The cortisone does not attack the root cause of the inflammation, it just suppresses it. In the case of inflammation without an apparent cause, cortisone can also heal the inflammation in the long term for unknown reasons
forecast
There is no general assessment of whether the inflammation of the spinal cord is curable. The different causes result in different treatment strategies and thus different chances of recovery.
A pathogen-related genesis of spinal cord inflammation usually has a good prognosis. With antibacterial and antiviral drugs, a cure and fight against the pathogen can be sought. The spinal cord inflammation also usually goes away after the causative agent has been eliminated.
Idiopathic inflammation can also be cured in a large number of cases.
Autoimmune diseases, however, represent a protracted course of the disease for many sufferers. With the help of cortisone and many other therapeutic options, the disease can usually be well controlled, and phases can even be completely asymptomatic. However, a complete cure of the disease is only possible in the rarest of cases.
How dangerous can that be?
In principle, you always have to look at the spinal cord inflammation where the inflammation is. The deeper it sits, the fewer failures are to be expected, usually these are not life-threatening, but great stresses can still arise in everyday life. The disease can become really dangerous when it comes to the involvement of the brain stem or other brain structures. In this case, one speaks of encephalomyelitis, as it occurs, for example, in the context of acute demyelinating encephalomyelitis (ADEM).
Duration
The duration of a spinal cord inflammation cannot be answered across the board. It depends on the underlying disease and the start of therapy. An early start of therapy can have a positive influence on the duration and minimize complications.
If inflammation of the spinal cord was triggered by a disease such as multiple sclerosis or lupus erythematosus, it can become chronic and cause symptoms again. In most cases, patients feel better after about three months. Most patients are symptom-free within a year, although there can be courses in which the healing process can take up to two years.
Duration of healing
No general statement can be made for the duration of healing. It can develop differently depending on the disease. In some cases, the healing process may fail - instead, the inflammation may become chronic and cause recurring symptoms. This is particularly the case with autoimmune diseases. These are diseases such as multiple sclerosis, lupus erythematosus or sarcoid. Adequate therapy can reduce the symptoms.
However, if the inflammation of the spinal cord is infectious, healing can occur after a few months. Most patients are symptom-free within a year. However, there are also cases in which the healing process is delayed.
What is chronic spinal cord inflammation?
The majority of myelitis is acute in one episode (monophasic) and can be brought under control with so-called immunomodulatory measures that influence the immune system. However, chronic spinal cord inflammation can also occur, especially if it is caused by severe autoimmune diseases. The term “chronic” in medicine initially only means “lasting over a long period of time” and is defined differently for different diseases. There is no clear limit for myelitis, but if it lasts more than 6 months one can certainly speak of chronic inflammation. Such patients in particular need extensive therapy, including neurological rehabilitation, in order to treat the neurological problems that have arisen.
What are the long-term consequences?
The long-term consequences of myelitis vary considerably from person to person - they depend on the underlying disease and the location of the inflammation.
If the inflammation is infectious, it can heal without consequences if therapy is started in good time. If this is not the case, various failure phenomena can result. These can manifest themselves in the form of sensory disorders or motor malfunctions. Usually the strength is reduced and the muscles tire very quickly. This can result in restrictions in everyday life, so that one is dependent on help.
Long-term consequences can also arise in the context of an autoimmune disease. The likelihood of failure symptoms is even increased with these diseases, as there is still no cure. The affected patients are usually treated symptomatically and immunosuppressants are prescribed so that the body's own immune cells do not further damage other cells in the body.
The symptoms of failure depend largely on the location of the inflammation. An inflammation that occurs in the cervical spine leads to more pronounced deficits than an inflammation in the lumbar spine. Parasitic sensations can occur. This means that touching cannot be perceived or a tingling sensation arises. The sensation of temperature or pain can also be disturbed. Motor disorders can also occur. Muscle strength is reduced and the affected muscle area tires more quickly. The reflexes can also be changed - they are usually increased.
prophylaxis
There is no prophylaxis that can be taken against the occurrence of spinal cord inflammation. Avoiding certain risk areas or behavior is generally recommended. In this way, an infection, which under certain circumstances would cause inflammation of the spinal cord, can be prevented.
An inflammation of the spinal cord, which is due to a past vaccination occurs is very rare these days and should in no way serve as a reasonnot to have a vaccination carried out.
Inflammation of the skin of the spinal cord
Inflammation of the spinal cord can also be secondary in the context of an earlier inflammation of the skin of the spinal cord (Spinal meningitis) arise when the inflammatory process spreads from the skin of the spinal cord to the spinal cord itself (meningomyelitis).
The inflammation of the skin of the spinal cord is either caused by viruses (most frequently), Bacteria (most dangerous) or other microorganisms such as parasites or fungi as well as non-infectious events (e.g. sarcoidosis, lupus erythematosus, side effects of drugs (NSAIDs, antibiotics), metastasis of a primary carcinoma).
The symptoms of meningitis that precede or co-occur with myelitis are primarily high fever, (head) pain, stiff neck, and possibly a decreased level of consciousness.
In the course of the inflammatory process, which spreads to the spinal cord tissue itself, the typical symptoms of myelitis then appear.
Inflammation in the spinal cord of the cervical spine
Depending on what level of the spinal cord the inflammation occurs at and how intense it occurs, symptoms of myelitis can vary. If the focus of inflammation is predominantly in the area of the spinal cord of the cervical spine, this is known as cervical myelitis. Initially, there may be sensory disturbances, a feeling of weak muscles and pain in the upper extremities (Arms and hands) come.
If damage to the spinal cord tissue occurs predominantly on only one side of the myelitis, so-called half-side symptoms can arise, in which abnormal sensations, reflex changes, paralysis and coordination disorders can occur in only one upper half of the body. In the worst case, severe inflammation with subsequent nerve cell damage to the entire cross-sectional area of the spinal cord of the cervical spine can lead to high cross-sectional symptoms.
Please also read: Symptoms of paraplegia
Inflammation of the spinal cord and brain
Inflammation of the spinal cord (Myelitis), as well as inflammation of the brain tissue (encephalitis), can occur separately, but in some cases both structures can be affected by inflammation at the same time, so that one speaks of so-called encephalomyelitis.
Encephalomyelitis is observed much more frequently in everyday clinical practice than spinal cord or encephalitis alone.
The cause of a combined inflammation is in most cases a spread of the encephalitis pathogen (Viruses, bacteria, parasites, fungi) via the bloodstream to the spinal cord, but an ascending infection / inflammation from the spinal cord to the brain is also possible.
Very rarely, a combined inflammation of the spinal cord and encephalitis can occur as a so-called vaccination damage, even after vaccinations.
Often, however, no clear cause of the encephalomyelitis is found during the diagnosis.
Typical symptoms of encephalomyelitis are high fever, headache, vomiting, speech disorders, neck stiffness, mental disorders (Symptoms of encephalitis) as well as abnormal sensations, back pain, paralysis or even symptoms of high paraplegia occur (Symptoms of myelitis).