Inflammation of the duodenum
General
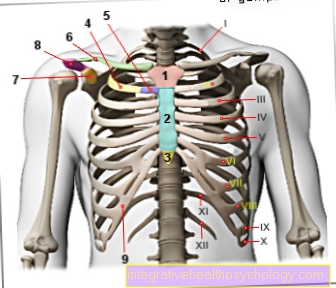
The duodenum is located as part of the five to six meters long intestinal tube directly following the Stomach gatekeeper and forms the first part of the small intestine as a 30 cm long C-shaped curve.
It is roughly level with the Costal arch, the edge of the lowest rib, slightly to the right of the midline. Its immediate neighbors are next to that stomach, to which he joins, nor the liver, the Gallbladder, the right kidney and the pancreas (= Pancreas).

The pancreas releases its digestive secretion through a long passage together with the bile from the gallbladder into the duodenum.
This also gives rise to the task of the duodenum in the Neutralization of gastric hydrochloric acidthat gets into the intestine with food from the stomach, as well as the breakdown of the food components. All of this is done with help basic secretions as well as the bile and the enzymes produced and released by the pancreas.
In medical terminology, the duodenum is called Duodenum designated. Next will be a inflammation in medicine always through the word ending "-it is" marked, from which the technically correct name of an inflammation of the duodenum easily results: The duodenitis.
The reason for naming the duodenum after the twelve fingers is due to its approximate width of 12 fingers. The individual layers of the intestinal wall are subdivided from the inside out into an inner layer of mucous membrane surrounded by 2 views of the muscles and connective tissue. Duodenitis generally affects the inner layer of the lining.
If deeper layers are also affected, one speaks of a ulcer (= Ulcer).
Symptoms
The signs of inflammation can vary widely.
It is not uncommon for it to go unnoticed and is only discovered by chance, if at all. The classic signs of inflammation in the duodenum go with it nausea, Vomit, pressing or stabbing Pain under the costal arch as well Appetite and digestive disorders hand in hand. Occasionally the pain can also show in the back. This makes it difficult to find a diagnosis.
At the Duodenal ulcer these signs mainly occur between meals or on an empty stomach improve through Ingestion, that means the pain subsides after eating. Patients who have a duodenal ulcer due to permanent inflammation should consider signs such as severe stomach pain, bloody or black chair or Vomit always see a doctor immediately as they may be signs of bleeding into the intestines. Duodenitis can rarely be a cause of diarrhea. Of course, diarrhea can occur in parallel with duodenitis for other reasons.
If the duct of the pancreas and gallbladder are also inflamed, inflammation of the pancreas (= pancreatitis) or a backlog of bile can result. The inflammation of the pancreas manifests itself in a distended stomach, belt-shaped pain (= pain that pulls around the abdomen like a belt) as well as nausea and vomiting. The biliary backlog can be recognized from a certain degree by the yellowing of the eyes and later of the entire skin, the so-called jaundice (= jaundice).
You might also be interested in this topic: Duodenal ulcer
causes
Infectionswho have taken harmful drugs, stress or the disease of a neighboring organ are the most common causes of inflammation of the duodenum.
Very rarely can a Crohn's disease, a chronic inflammatory bowel disease, can cause inflammation of the duodenum.
Infections with many different germs can cause inflammation of the duodenum. By far the most common infection is that with the germ Helicobacter pylori. This germ nests in many people Childhood in the stomach.
However, he only makes complaints 10% of those affected.
Through its unique ability ammonia to be able to form it not only leads to in the stomach but also in the small intestine Irritation of the surface mucosa and it can eventually ignite if irritated persistently. If the inflammation exceeds the superficial layer of the mucous membrane, a duodenal ulcer can develop in these cases.
The drugs that irritate the gastric and duodenal mucosa and lead to inflammation are the so-called Non-steroidal pain relievers first of all. Even if most people don't know what the term non-steroidal is, most people know its best-known representatives:
- Acetylsalicylic acid (e.g. Aspirin®, ASS®)
- Ibuprofen (e.g. Nurofen®, Neuralgin®)
- Naproxen (e.g. Dolormin®)
- Diclofenac (e.g. Voltaren®).
They are used as pain relievers rheumatism and other inflammatory joint diseases such as rheumatoid arthritis, the M. Bechterew or also the gout used and often lead to inflammation of the stomach or duodenum surface with prolonged use.
alcohol is a possible triggering factor for both the inflammation of the duodenal lining and for the inflammation of the lining of the stomach. However, this is not yet clear. The fact is, however, that the consumption of alcohol in an already existing inflammation counterproductive affects the development of this. In addition, if you have duodenitis, symptoms such as pain and nausea can worsen after drinking alcohol.
diagnosis
As an examination method is next to roentgen and Ultrasonic nor the Duodenoscopy for the duodenum and other sections of the intestine.
The duodenoscopy is like a Gastroscopy a thin tube in which a camera is built in through the esophagus and the stomach placed in the duodenum via which the mucous membrane can then be examined when projected onto a screen.
A small instrument attached to the tube can be used as part of a duodenoscopy rehearse are taken from the intestinal wall, the examiner should discover suspicious areas on the surface mucosa (= Biopsy).
If a patient suffers from the disease, this is impressive for one swelling the mucous membrane of the uppermost intestinal wall layer or the occurrence of gastric mucosal cells in the duodenum.
Particularly severe forms of inflammation are associated with one Thinning (= atrophy) the mucous membrane to recognize. A Gastric ulcer can be recognized as a sharply demarcated inflammation. In combination with a thin ultrasound device, the intestinal wall can also be scanned by Ultrasonic to be examined.
The complete examination can be carried out while awake or under superficial anesthesia, if desired
therapy

Therapy for inflammation of the duodenum primarily consists of treating the underlying cause.
In the case of inflammation within a Pain reliever treatment these should be replaced immediately with alternative preparations that do not irritate the mucous membrane. Is the cause in an infection with Helicobacter pylori so if left untreated, the inflammation will not go away.
The therapy here then consists in the indirect treatment of the inflammation by ending the colonization with Helicobacter pylori.
This therapy is called Eradication and normally takes about 7-10 days. During this time, a gastric acid blocker (usually a so-called proton pump inhibitor) together with a combination of 2 Antibiotics (usually amoxicillin, clarithromycin, or metronidazole) are being taken. After this time, the germ has been fought successfully in most cases and the mucous membrane of the stomach and duodenum can recover from the inflammation.
For all other inflammations it can often be helpful Gastric acid production because the hydrochloric acid produced in the stomach can also cause enormous damage to the sensitive mucous membrane in the duodenum.
Less hydrochloric acid from the stomach therefore also causes less damage in the duodenum. The reduction in gastric acid production is due to a healthy lifestyle with easily digestible, low-fat, milder Whole food sufficient in mild cases.
Foods that are difficult to digest and high in fat lie in the stomach for a very long time and lead to much more gastric acid production than light products that are quickly in the rest Digestive tract can be digested.
It is better to eat several small meals than a few large ones. If these measures are insufficient, there are also drugs that chemically regulate gastric acid production. In addition to lighter preparations such as the so-called Antacids (= "Against acid") play those already mentioned above Proton pump inhibitors here a prominent role as the most effective gastric acid-reducing drugs.
Also from the field of Natural remedies there is support for treating inflammation in the duodenum. Here are suitable Mustard seeds, such as Plantain juice mixed with honey or mixtures of aloe with sugar water and white wine.
Medication
As already described above, duodenitis is often colonized with the bacterium Helicobacter pylori responsible. If this is the case, drug therapy is often required to eliminate the bacterium. One speaks of an eradication therapy. A combination of three active ingredients is usually used here. These are the acid pump inhibitor omeprazole and two antibiotics.
These are either clarithromycin and metronidazole or clarithromycin and amoxicillin. Painkillers from the group of non-steroidal anti-inflammatory drugs should be avoided in the presence of duodenitis. They are not infrequently the cause of the disease and often lead to a worsening of an existing inflammation. This group of drugs includes, for example Ibuprofen and Diclofenac. Diclofenac in the form of an ointment (for example Voltaren®) is not affected by this, as the substance is not absorbed into the body.
Home remedies
In the case of duodenitis, eating foods that are gentle on the stomach and avoiding the consumption of alcohol, nicotine and coffee help relieve symptoms. Warm, gentle types of tea such as chamomile tea or mint tea can help. There are no specific home remedies for treating duodenitis.
nutrition
In the case of inflammation of the mucous membrane of the duodenum, the same generally applies to the recommended diet as in the case of inflammation of the gastric mucous membrane (gastritis): Food should be consumed as easily as possible. Fatty and spicy dishes are to be avoided. Alcohol should also be avoided in the presence of duodenitis, as this can lead to additional irritation of the mucous membrane. The same applies to coffee and nicotine.
forecast
Depending on the cause of the inflammation of the duodenum, the prognosis is generally quite good.
Causes such as inflammation from irritating drugs or the germ Helicobacter pylori can be treated relatively easily and usually lead to healing and freedom from symptoms within a few days to weeks.
If the cause of the inflammation cannot be clarified, there is a risk that the inflammation will recur and a lifelong gentle diet as well as the permanent intake of a gastric acid blocker will be necessary.
In addition to a healthy diet, the personal risk can also be caused by the Refrain from smoking and alcohol be lowered.
Duration
The duration of duodenitis depends on the cause and the therapy. Often duodenitis - like gastritis - is caused by the colonization of Helicobacter pylori. If this is the cause, drug therapy is usually required. The inflammation then continues until the therapy is successful. In the case of triggers such as stress or noxious substances (for example alcohol, nicotine or certain painkillers), the inflammation often only ends when the triggering factors are switched off. Duodenitis does not always have to be accompanied by symptoms, however, so that the person affected sometimes does not notice how long it has been going on.
prophylaxis
A Inflammation prophylaxis is possible through a healthy and balanced lifestyle, among other things.
The diet should be similar to that of an existing inflammation and consist of easily digestible, low-fat, mild whole foods. The meals should also be divided into several small instead of a few large ones. Smoke and alcohol should be avoided as a stimulus to gastric acid production.
Sensitive patients should take pain medication stomach-sparing preparations To fall back on.
If the risk factors cannot be avoided, prophylactic measures can be taken on medical advice in some cases Gastric acid inhibitors are used to prevent inflammation.
An inflammation with Helicobacter pylori is difficult to prevent, as the infection usually took place years or decades before in childhood. However, if you are definitely affected by a Helicobacter pylori colonization, you should think about preventive treatment of the colonization if you have to take non-steroidal pain relievers or other drugs that damage the small intestinal mucosa in order not to unnecessarily increase the risk of inflammation of the duodenum










.jpg)