Herniated disc of C6 / 7
definition
The herniated disc (also Disc herniation or. Prolapsus nuclei pulposi called) describes the penetration of parts of the intervertebral disc into the spinal canal.
In the process, the ring of fibrous cartilage tears, too Anulus fibrosus disci intervertebralis called, from. Normally, the ring of fibrous cartilage forms the outer edge of the intervertebral disc, where it plays a decisive role in the positioning of the central part of the spine, the so-called gelatinous nucleus (lat .: Nucleus pulposus).This nucleus of jelly “falls” into the spinal canal in which the spinal cord is located when the fibrous ring loses its function and presses off the nerve fibers located there.
Read more about this at: Herniated disc of the cervical spine - what is it?

Illustration of a herniated disc

Disc prolapse -
Nucleus pulposus prolapse
A - herniated disc from the left
B - herniated disc from above
C - Healthy disc
a - neck and chest area
b - lumbar region
- Fiber ring -
Annulus fibrosus - Gelatinous core -
Nucleus pulposus
1st + 2nd intervertebral disc
(Intervertebral disc) -
Discus inter vertebralis - Spinal nerve -
Spinal nerve - Spinal cord -
Medula spinalis - Vertebral bodies -
Corpus vertebrae - Spinous process -
Spinous process
You can find an overview of all Dr-Gumpert images at: medical illustrations
The so-called intervertebral disc protrusion (lat .: protrusio). Here the fibrous ring remains intact and symptoms as severe as in the complete incident are less common.
Overall, the herniated disc is the second most common pain syndrome after headache with a 79% risk of developing a herniated disc once in a lifetime.
causes
The main cause of herniated discs is usually an increasing damage to the intervertebral discs over a long period of time with accompanying degeneration of the fibrous cartilage ring. In contrast to most other components of the human body, hyaline cartilage like the fiber ring is not supplied directly by blood vessels, but by diffusion, i.e. by moving substances through different body layers (or membranes).
If these membranes are damaged for a long time by forces acting on them, the fibrous cartilage, which normally consists of approx. 80% water, is no longer adequately supplied and begins to dry out.
The loss of water reduces the elasticity of the cartilage and increases the likelihood of tearing.
This can be promoted by bad posture, such as office work with long periods of sitting at the desk, but also by genetic causes or incorrect stress.
Overweight and a lack of exercise are also major risk factors.
Read more on the topic: Causes of a herniated disc
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Symptoms
In general, the most typical and leading symptom of a herniated disc is a sudden onset of sharp pain in the region supplied by the affected nerve.
The symptoms of herniated discs therefore depend on the location of the incident.
Depending on the height at which the intervertebral disc protrudes, the respective spinal nerve can be affected, which supplies specific muscles based on strength and specific skin regions based on sensation.
For the nerve root C6 / 7, pain symptoms on the index, middle and ring fingers as well as in the middle of the back of the hand are typical. Alternatively or at the same time, there may be numbness in the areas described.
If there is pain in the neck and arm, one speaks of one in medicine Cervicobrachialgia. In addition to a herniated disc, this can also have other, more trivial causes.
Read more about this at: Cervicobrachialgia
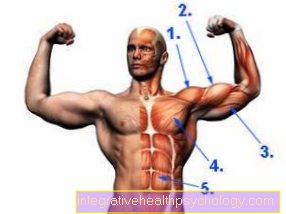
The upper arm muscle Triceps brachii muscle, known colloquially as the triceps, is the key muscle of the C6 / 7 nerve root region. This means that by examining this muscle, the doctor can determine whether there is nerve damage to the C6 / C7 level: In such a case, the triceps muscle would lose strength.
The accompanying pain can also lead to increased blood flow to the affected skin areas.
Read more on the subject at: Symptoms of a herniated disc of the cervical spine
Pain
In addition to the symptoms of paralysis and sensory disorders described above, such as pins and needles or tingling on the skin, the pressure of the herniated disc portion on the sensitive nerve roots leads to sudden, very severe pain.
These pains radiate into the areas supplied by the nerve root.
However, a herniated disc is not the cause of every form of suddenly occurring, radiating pain in the arms or legs.
Tension, degenerative diseases of the spine, masses such as swellings, effusions, etc. can lead to pain that has similar characteristics to the pain caused by a herniated disc.
Read more on the topic: Disc pain
Numbness and tingling
The middle part of the intervertebral disc that has herniated can compress or press the nearest nerve root in the spinal cord.
From these compressed nerve roots arise, however, nerves which on the one hand control the muscles (motor nerve fibers) and on the other hand ensure the sensation of the skin (sensory nerve fibers).
In addition to the symptoms of paralysis that are triggered by the effect on the motor nerve fibers, the compression of the nerve root can also cause sensory abnormalities.
These sensitive abnormal sensations include pain on the one hand and numbness on the other. So-called abnormal sensations such as pins and needles or tingling can also arise.
So numbness and paralysis are strongly in favor of performing a relieving operation.
Read more on the topic: Is numbness an indication of a herniated disc?
Involvement of identification muscles
For almost every nerve root in the spinal cord there is a key muscle that is only or mostly innervated by nerves from this root. If such identification muscles fail, there is an urgent suspicion of an injury at the level of the special nerve root.
The key muscle for segment C6 is the Brachioradialis muscle, which is located on the forearm on the thumb side and allows the wrist to rotate in addition to a slight flexion in the elbow joint. The reflex for testing the brachioradialis muscle is the Radius periosteal reflexthat the doctor can test with a reflex hammer
The identification muscle of segments C7 / 8 is the Triceps brachii muscle, colloquially just called the triceps. The triceps are located on the back of the upper arm and are primarily responsible for stretching the elbow joint. The corresponding reflex is that Triceps reflex.
diagnosis
As with many diseases with nerve involvement, the basis of the diagnosis lies in the physical examination.
Muscle strength and sensitivity in various nerve supply areas are tested here.
However, the final diagnosis of a suspected herniated disc is based on imaging techniques such as MRI, CT or X-ray.
X-rays show the cervical spine in two planes. From the front (also called AP for anterior-posterior) and from the side. Here the intervertebral discs can be assessed and various degenerative diseases of the spine can be excluded.
The diagnosis of choice, however, is MRI, which enables a more precise assessment and examination without exposure to radiation.
A so-called myelography can also be performed to specifically display the spinal cord and the spinal canal. A contrast agent is introduced into the vertebral canal, which means that the spinal cord can be clearly demarcated in subsequent imaging.
Read more on the topic: How can you recognize a herniated disc?
MRI of the cervical spine
Since MRT, i.e. magnetic resonance tomography, is based on the use of magnetic waves and not X-rays, it is the gentlest diagnostic measure, albeit the most expensive and complex.
In contrast to X-rays, MRI not only shows high density body parts such as bones, but also ligaments and other soft tissue organs.
This allows precise information about the type, direction and progress of a herniated disc.
A disadvantage of the MRT recording is the long time the patient remains in the recording device, which is especially important for patients claustrophobia, so with fear of closed spaces, burdened.
If the severity of the anxiety disorder is not too fulminant, this fear can be dampened with tranquilizers for the duration of the diagnosis, or other methods such as open MRI are used.
Read more on the topic: MRI of the cervical spine
therapy
Conservative treatment
The majority of patients with herniated discs are treated conservatively, i.e. without surgery.
A distinction is made between self-limiting (i.e. stopping to a certain extent) and progressive courses.
Conservative therapy is usually the method of choice, particularly in the case of self-limiting courses without symptoms of paralysis.
First of all, a reduction in pain is achieved through rest and drug therapy, which then enables the trunk muscles to be strengthened by a physiotherapist.
Read more about this at: Exercises for a herniated disc and medication for a herniated disc
Heat therapy, massages and electrotherapy can also relieve symptoms, but the effect on the progression of the disease has not been scientifically proven.
The duration of conservative therapy is usually 6 to 8 weeks, if after this period there has been no improvement in symptoms, surgical therapy may be necessary.
Periradicular Therapy (PRT)
Periradicular therapy (PRT) is a radiological pain therapy that is used in patients with chronic pain due to degenerative spinal diseases.
The nerve root is localized by previous imaging using MRI or CT, which is then treated by targeted injection of a mixture of a local anesthetic and a steroid such as cortisone.
The local anesthetic has a pain-numbing effect, the steroid relieves inflammation and has a desensitizing effect. Before the PRT needle pricks, the skin is numbed with a local anesthetic, and after the prick, reimaging is used to determine whether the needle is in the correct area.
Read more about this at: Periradicular Therapy
Operation and duration of the procedure
In the case of herniated discs with severe complications such as paralysis symptoms or in the case of herniated discs in which conservative therapy has not achieved any improvement in symptoms, surgical therapy is indicated.
Approx. 140,000 herniated disc operations are performed annually.
A large number of these operations are not absolutely necessary, but around 10% of the operated patients would suffer permanent long-term damage if they decided against an operation.
There are two different basic forms of disc surgery.
In spinal fusion, i.e. the stiffening of the spinal column, the two vertebral bodies, which are in contact with the degenerated intervertebral disc, are fixed to one another by a screw. In this type of operation, part of the mobility of the spine is lost.
Read more about this at: Spinal fusion of the cervical spine
The other option is to insert an artificial disc, also known as a disc prosthesis. Here the mobility of the spine is largely preserved.
Read more about this at: Intervertebral disc prosthesis of the cervical spine
In the case of herniated discs in the cervical spine, the Spinal fusion the more frequently used form of the surgical technique, as the loss of mobility in the neck area is not as serious as in the lumbar vertebra area.
Most of the time, the operation is performed under general anesthesia.
Where previously an incision up to 30 centimeters long had to be made, nowadays minimally invasive procedures (so-called "keyhole surgery") can be used.
The duration of the operation is 30-60 minutes, but every patient should be admitted to the hospital the day before the operation and examined beforehand and possibly stay in the clinic for a day after the operation for monitoring.
Risks of the operation
The risks of the operation depend on the type of operation, whereby the risks with the minimally invasive operation method are significantly lower than with the open operation.
With both procedures, bleeding, wound infections, swelling and excessive scarring can occur.
These complications can be accompanied by pain. The so-called "Post Discectomy Syndrome“Occur in which the symptoms first improve after the disc surgery, but then reappear more intensely after a while. The risk of post-discectomy syndrome is even lower with interventions on the cervical spine; it is most likely to be triggered with interventions near the sciatic nerve on the buttocks.
Apart from the risks of the operation, the general risks of general anesthesia also apply. Subsequent nausea and tiredness often occur. Serious side effects, such as an anaphylactic reaction to the anesthetic, occur in 1 in 20,000 general anesthetics. Around 1 in 100,000 patients die under general anesthesia.
Read more on the topic: Side effects of general anesthesia
Duration of treatment
As already described, the duration of treatment for herniated discs depends on the type of treatment.
The conservative, i.e. non-operative, treatment takes about 6-8 weeks.
Surgical therapy, including preparation, surgery and aftercare, takes about 3 days. Afterwards, of course, there must be a period of physical rest in order not to disturb the healing of the wound.
Please also read: How long does a herniated disc last?
Sick leave for a herniated disc
Since the herniated disc can be accompanied by severe pain in the acute stage, patients, especially those in a physically demanding job, can be put on sick leave by their doctor on request.
However, recent studies have shown that a long bed rest in the context of a herniated disc is rather detrimental to healing, which is why patients are encouraged to organize their everyday life as actively as possible despite a certificate of incapacity for work.
However, the duration and intensity of treatment vary so widely from case to case that no general statement can be made about the duration of the certificate of incapacity for work.
In addition, there is often the opportunity to work part-time for a certain period of time after being unable to work.
Exercise with or after a herniated disc
In principle, sport is not only allowed in the case of herniated discs, it is urgently recommended.
However, there are some sports that place too much strain on the spine and should not be performed or only with the introduction of a specialist. For example, weightlifting is not only unsuitable, it is often the cause of degenerative diseases of the spine.
Endurance sports such as walking or swimming or exercises in the event of a herniated disc as part of physiotherapy are recommended.
Jogging in the event of a herniated disc is not advisable, however, as every occurrence results in a shock and subsequent compression of the spine, which - even if only slight - can still hinder healing.
Read more on the subject at: Exercise after and after a herniated disc