Epidural Infiltration
definition
Epidural infiltration (infiltration close to the spinal cord) is a conservative syringe therapy used to treat orthopedic diseases of the spine that lead to irritation / inflammation of the nerve structures in the area of the spinal canal (spinal cord, nerve roots).

Causes of nerve inflammation of the spine
To Inflammation of the spinal cord and nerve roots always occur when the space for these nerve structures in the spinal canal becomes too small. With such a Nerve inflammation is it a Not bacterial inflammation, i.e. Bacteria and pus play no role here. The sole cause is pressure damage to the nerves. As a result of the inflammatory process, the spinal cord and nerve roots swell, which further reduces the remaining reserve space for these nerve structures.The result is a vicious circle: pressure damage -> inflammatory swelling -> further pressure damage.
In what diseases is epidural infiltration used?

Classic clinical pictures for therapy with infiltrations close to the spinal cord are the Herniated disc / protruding disc and the spinal canal narrowing (Spinal stenosis).
disc prolapse
In the case of a herniated disc, the disc material from the core of the disc emerges from the back of the spinal canal and presses the spinal cord located there, and more often the nerve roots. It is usually a sudden event with severe back and leg pain (lumbar sciatica; lumbar spine) or neck and arm pain (cervicobrachialgia; cervical spine), depending on where the herniated disc is located. A bulging disc can, in exceptional cases, trigger symptoms of pain that are so severe that therapy with epidural infiltration makes sense.
Further information can be found under our topic:
- disc prolapse
and - Intervertebral disc bulge
Spinal stenosis
In spinal canal stenosis, signs of wear and tear on the spine are the cause of a usually slowly increasing spinal canal narrowing. The symptoms usually arise insidiously. That is more often affected Lumbar spine. The pain spread often affects both legs. The weakness of the legs and increasing insecurity when walking are very common complaints.
Further information can be found under our topic: Spinal stenosis and Spinal stenosis of the lumbar spine
Symptoms
The development of complaints is based on two things:
- The strength of the pressure damage: The stronger the pressure on the nerve structures, the greater the discomfort.
- The speed of pressure damage: The faster the pressure on the nerve structures develops, the greater the discomfort. In the assessment of imaging procedures (e.g. MRI), in relation to the complaints presented, this can mean, conversely, that comparatively very tight spaces for the nerve structures can cause few complaints if they have developed slowly enough. The nerve structures had the opportunity to adapt (adaptation) to the new space. If the extent of the possible adaptation is exceeded, the clinical picture decomposes. The complaints will then accentuate (increase significantly).
Symptoms of nerve damage include
- Local back pain
- Referring pain to arms or legs (Cervicobrachialgia / Lumboischialgia)
- Reflex failures
- Sensory disorders of the skin
- Loss of strength of the muscles / paralysis (Paresis) e.g. Loss of maximum walking performance, tired legs, unsteadiness when walking, weakness of the ankle and the lower leg
Please also read our pages Is Does tingling indicate a herniated disc? and Is numbness an indication of a herniated disc?
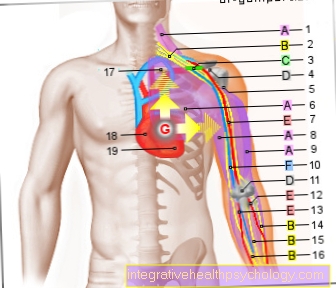
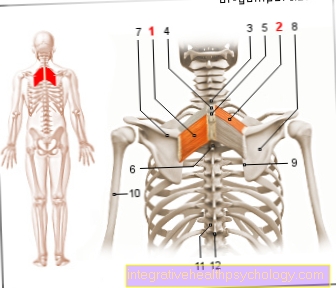
Access routes
There are two types of access routes for infiltration, depending on the level of the inflammatory processes to be treated: on the one hand, epidural infiltration and, on the other hand, sacral infiltration.
Epidural infiltration is used on affected areas of the upper lumbar spine and the sacral access route is used more on affected areas of the lower lumbar spine and sacral nerves.
The main difference between the two access routes is the position of the needle; the therapeutic effects and drugs used remain the same.
With sacral infiltration, access takes place at the lower end of the sacrum. The spinal canal continues into the sacrum, but since the sacrum does not have any gaps like the movable spine, the needle must be inserted into the vertebral canal from the lower end of the sacrum.
In epidural infiltration, the needle is positioned between the spinous processes of the lumbar spine and from there pushed into the vertebral canal, the so-called epidural space. This access route can also be used on the cervical spine, but it must be checked by x-rays at this level.
Epidural Infiltration
As with spinal cord anesthesia, with epidural infiltration, a height is set for the infiltration from the back. This is based on the level of the existing pathological changes, for example whether a spinal canal narrowing has the main finding in the area of the 2nd lumbar vertebral body, or whether it is deeper or higher.
Lumbar spine infiltration is usually performed with the patient sitting and leaning forward. After the skin has been disinfected, the height of the access is determined by touch and the infiltration needle is inserted into the spinal canal up to the hard skin of the spinal cord (Dura) advanced. After piercing the vertebral arch ligament (Ligamentum flavum) there is a sudden drop in the plunger pressure of the syringe, from which the doctor recognizes that the spinal canal has been reached.
If the skin of the spinal cord is injured, nerve fluid flows out of the needle (Cannula) and the needle has to be withdrawn a little (this would correspond to the positioning of the needle for spinal anesthesia). The resulting hole in the hard skin of the spinal cord closes by itself. The patient does not usually have to worry about complications. Injury to the spinal cord nerve fibers is also not to be feared, because from a certain area of the lumbar spine they swim in the nerve water and can easily avoid the cannula.
In contrast to sacral infiltration, the access route for epidural infiltration is variable. This means that changes in the spine at a higher level can also be treated with nerve root irritation.
Epidural infiltration is also suitable for herniated discs in the cervical spine or for a painful narrow spinal canal in the cervical spine.
In contrast to therapy on the lumbar spine, the needle position must be checked using a mobile X-ray device (X-ray image converter).
Epidural infiltration of the cervical spine
A long needle is used to locate the spinal canal under X-ray control and a mixture of saline and cortisone is injected directly in front of the spinal cord at the level of the herniated disc. Epidural means that the drug is injected into the hard skin of the spinal cord (dura) in front of (epi), so it is not injured and the spinal cord does not run the risk of being injured. Since the spinal cord and its skin cannot be seen on an X-ray, a small amount of an X-ray contrast agent is injected before the drug is administered.
Based on the distribution of the contrast agent, it is possible to check the position of the needle tip, so that the method is not very dangerous. By distributing and flushing the spinal cord and its outgoing nerve roots, this infiltration usually reaches several nerve roots at the same time.
The pain therapy effect is very good. The infiltration can be repeated several times. An anesthetic is not necessary. The procedure is not particularly painful either.
Epidural infiltration of the lumbar spine
The goal of epidural infiltration in the lumbar spine is to inject a drug directly into the epidural space in the spinal canal. This plays a decisive role in the treatment of chronic back pain or in preparation for operations. In the case of epidural infiltration of the lumbar spine, the anesthesia is particularly effective in the area of the lower extremities and the lower lumbar region. Another area of application is obstetrics. An injection is given into the vertebral canal shortly before birth to minimize pain during the birth process. In the event of complications, a caesarean section can also be performed without any problems.
At the beginning of the procedure, the patient is prepared by disinfecting the affected area on the back and numbing the area locally. This preparation prevents infection and reduces the pain when sticking the needle. Epidural infiltration is usually performed while sitting or lying on your side. The needle is inserted between the spinous processes of two adjacent vertebrae.
To check whether the doctor has reached the epidural space, a so-called "loss of resistance" technique is available. The doctor uses a small syringe filled with liquid. Before the needle can reach the epidural space, it must first pierce the skin and a ligamentous apparatus. While the syringe is in this solid ground, the doctor must apply some force to squirt the liquid from the syringe against the resistance of the tissue. Only when the needle is in the epidural space does it work without great effort.
With this method, the doctor can check whether the injection has been placed correctly even without parallel imaging. When the needle is finally in position, the anesthetic is injected. This is now in the gap between the hard meninges (dura mater) and the periosteum of the vertebral body and can thus develop its effect at the exit points of the spinal nerves. This includes freedom from pain in the affected segment, as well as restricted mobility and insensibility.
Overall, the epidural infiltration of the lumbar spine only takes a few minutes without complications. It is now a tried and tested means of effectively preventing pain, be it just before painful procedures or for pain therapy.
Sacral infiltration
For the treatment of nerve irritation, especially Sacral blockages or sacral infiltrations are suitable for the lower lumbar spine sections. A mixture of local anesthetic / local anesthetic and cortisone is injected through the sacral canal (Sacrum canal) is injected into the spinal canal. The access is in the course of the sacrum above the arched transition to the coccyx. Imaging (X-ray) is not absolutely necessary for sacral infiltration. You orientate yourself on the anatomical landmarks.
Then 20 ml of a mixture of a local anesthetic and cortisone are injected into the spinal canal under sterile conditions. There, the fluid spreads around the spinal cord and several nerve roots in the lower lumbar spine (LWS) at the same time.
Sacral infiltration is particularly suitable for the treatment of:
- a herniated disc L4 / 5
- a herniated disc L5 / S1
and - Intervertebral disc protrusions of the two lowest intervertebral discs
in the case of corresponding nerve root irritation or spinal stenosis in this area, where several nerve roots can be involved in the disease process at the same time. Higher nerve roots are no longer reached in therapeutically effective doses due to the access route of the drug application, or very high drug volumes have to be infiltrated (30/40 ml).
Depending on the local anesthetic used (local anesthetic), the patient is then asked to lie down for some time (1-2 hours), as the local anesthetic can sometimes lead to sensory disturbances and a feeling of weakness in the legs, which creates a risk of falling. There is also the possibility of spontaneous water loss (Incontinence). The patient must be made aware of this in advance of therapy. After the anesthetic wears off, these effects disappear again.
The pain therapeutic effect is good and also persistent due to the applied cortisone. Sometimes the increase in volume and pressure in the spinal canal can cause a temporary increase in pain. As a harmless side effect of cortisone, facial flushing (see flush syndrome) can occur, which disappears after a few days. The sacred infiltration can be repeated several times. It can also be carried out in the practice if the local anesthetic is dispensed with entirely or a very low dose is chosen.
Read more about the topic here: Cortisone therapy for a herniated disc
Risks
As with any medical procedure, epidural infiltration can lead to complications. These can be caused by the attending physician as well as by unfortunate coincidences.
For example, if the doctor injures a vessel in the spinal column or spinal cord with the needle, bleeding can occur. Depending on the location of the damaged vessel, the blood can get into the liquor or into compartments around the spine. In the case of major bleeding, the resulting hematomas must be surgically removed. This circumstance would only be another source of pain for the patient and should therefore be avoided by the doctor as much as possible.
In addition to the vessels, there are numerous nerves running in the lower back that could be injured with a needle. Depending on the type of nerve affected, symptoms of different severity can be expected. If the doctor hits a peripheral nerve, it can lead to sensitivity disorders or motor failures of the muscles.
In the dramatic case of an injury to the spinal cord, the consequences are far more far-reaching. From harmless insensitivity to pressure and pain in small areas of the skin to paraplegia, everything is possible. Admittedly, the doctor has to do a few things wrong before it comes to that. In addition, internal organs such as the kidney and liver can be accidentally punctured and injured if the doctor's needle is inaccurate. This can lead to dysfunction and bleeding. Such gross errors by the doctor are considered gross malpractice and are also very rare.
Since a drug is administered, the risk of allergy or even anaphylactic shock is always acute. In the event of fever or rashes after epidural infiltration, the patient should immediately consult a doctor to clarify possible complications. At the same time, such symptoms can also indicate a bacterial infection, which can be caused by the procedure. Since the meninges are pierced during epidural infiltration, such an infection can spread to the brain and lead to meningitis.
Serious consequences such as cerebral damage can occur here.
Since the treatment is often monitored with imaging methods such as X-rays, the patient is exposed to a certain level of radiation exposure, which, thanks to technically advanced equipment and relatively short exposure times, is very low.
Side effects of epidural infiltration
Various circulatory symptoms can occur as side effects of epidural infiltration - nausea, dizziness and Vomit.
As a direct effect of injecting the local anesthetic into the epidural space, numbness and weakness can occur in the patient's legs, which can persist for up to several hours after the injection. Therefore, the patient should initially lie down and not actively participate in road traffic.
The cortisone used can cause a number of side effects - but these are unlikely or only to be expected to a limited extent, since comparatively small amounts of cortisone are used in epidural infiltration. Possible side effects from cortisone would be Weight gain, Increase in blood sugar, Rise in blood pressure, osteoporosis, the Cushing Syndrome and further shifts in hormone control crises, e.g. the sex hormones.
Some patients may experience an allergic reaction as part of the epidural infiltration. This can be done through the cortisone, the local anesthetic or one of the substances in which the medication is dissolved.
Changes in the skin, such as redness or itching, may be signs. An extreme case would be a anaphylactic shock, i.e. a systemic hypersensitivity reaction to one of the substances.
Complications
With epidural infiltration there is always the possibility that the needle used for the injection injures or irritates structures running there.
- If a vein in the epidural space is injured, a hematoma (bruise) arise. This can be small and without symptoms. In the worst case scenario, the hematoma would be pressing on the nerve root in the spinal canal, causing symptoms of paraplegia downstream from the injury. Such a hematoma is very rare.
- In addition to injuring vessels, peripheral nerves can also be affected by the epidural infiltration. This could lead to sensitive failures in the skin areas that are supplied by the affected nerves.
-
Another complication would be that the injection was not performed sterile and the puncture cell becomes infected by the entry of bacteria. The worst possible outcome can be that bacteria reach the brain and cause meningitis (meningitis).
-
For injuries to the hard meninges (Dura mater), so if the doctor unintentionally pricks too deep, post-punctual headache can occur. Patients complain of headaches in the forehead and neck area with other symptoms such as nausea, vomiting, dizziness, neck stiffness and visual disturbances. The reason for this is presumably that the place where the meninges was injured is CSF (Brain water) leaks, and irritates the meninges through various mechanisms.
Injury to the spinal cord is a rare complication. This can occur when an epidural infiltration is performed above the second lumbar vertebra (L2) and the needle is inserted too deeply through the dura mater (Hard meninges) and the arachnoid mater (Spider skin) into the subarachnoid space (Cerebral water space) is coming. -
If the local anesthetic is accidentally injected here as well, there is a risk of spinal anesthesia - i.e. a complete or partial shutdown of the spinal cord. This can be at the appropriate height (Proximity to the brain stem) cause cardiovascular collapse, respiratory paralysis and convulsions.
Effect of epidural infiltration
Note: This section is for the very interested reader
The effect of the epidural infiltration is based on the injected medication. Usually, cortisone and a local anesthetic are injected.
The cortisone has an anti-inflammatory effect where the syringe is placed. It is a naturally occurring substance in the body that is produced in the adrenal cortex.
In addition to regulating metabolic pathways in the body, cortisone has a regulating function in the immune system. This is relevant for the use of cortisone in epidural infiltration. It has an anti-inflammatory effect by inhibiting NFKB.
This is a transcription factor (a protein that controls the reading of the DNA and thus the production of proteins), which regulates the synthesis of proinflammatory mediators (inflammatory signal substances), such as the prostaglandins. Due to the reduced amount of inflammation-promoting substances, the inflammation and thus also the swelling at the problem area on the spine are reduced. Since the swelling no longer constricts the nerve fibers, the pain should subside.
The local anesthetic prevents the pain that arises from being passed on. Local anesthetics used in epidural infiltration are sodium channel blockers.
These work in that the electrical potentials are conducted through the nerve via the information, are interrupted or electrical stimuli do not develop. The exact way it works is that the local anesthetics block sodium channels on the nerve fibers - the lack of sodium influx does not lead to depolarization of the nerve fiber (Become positive) and thus not to the formation of a potential difference along the nerve fiber.
In this way, pain signals are no longer transmitted from the previously painful area to the brain. But this condition is not permanent.
Read more on the topic: Conduction anesthesia
Furthermore, due to the absence of pain transmission, no further inflammatory cells are stimulated to secrete proinflammatory substances, so that this also causes a reduction in inflammation and thus a further reduction in pain.










.jpg)