Skin changes
Below you will find an overview and a brief description of the most important skin changes. You will receive information about the individual skin lesions and the typical symptoms in which they occur. In each section you also have the option of referencing our main articles and obtaining further information.

Forms of skin changes
The skin changes mentioned below describe the terms that a specialist in dermatology uses to describe skin changes with medical precision.
Skin lesions
Skin changes are known as skin lesions. All skin diseases can be described with the help of these efflorescences.
Skin lesions can be roughly divided into two groups:
- Primary lesions are skin changes that are directly caused by a skin disease
- Secondary fluorescences Secondary fluorescences arise either from primary fluorescence or from external damage to the skin
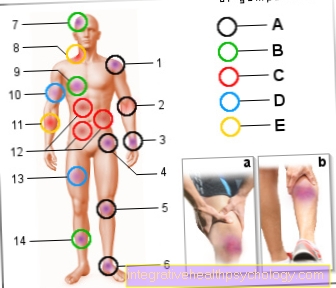
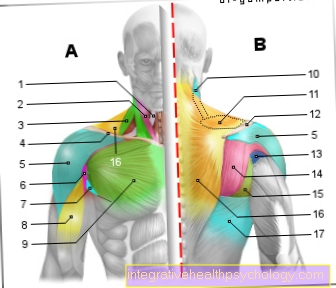
Illustration of skin lesions

Skin changes
Efflorescences
A - Primary lesions
(Due to a skin disease
caused)
- Macula (spot)
- Papula
(Papule, nodule) <0.5 cm
Nodus (like papula) 0.5 - 1 cm - Urtica (wheal)
- Vesicle
- Bulla (bladder)
- Pustula (pustule)
B - Secondary lesions
(From A or through damage
of the skin) - Squama (scale)
- Crusta (crust)
- Cicatrix (scar)
- Rhagade (cracks, fissure-shaped cracks)
- Erosion
- Excoratio (defect down to the dermis)
- Ulcer (swelling)
- Atrophy (tissue atrophy)
You can find an overview of all Dr-Gumpert images at: medical illustrations
Primary lesions
Here is an overview of the primary fluorescences:
- The macula, in English the spot, is a circumscribed, non-palpable change in the skin. So you can see the boundaries of this spot, but the spot itself is not raised. That means that you can go through the mere Stroke-over-the-skin can't feel the change. The macula is limited in its extension to the uppermost layers of the skin.
- The papula, also called nodule or papule, is a small, circumscribed elevation. There are papules of the upper, but also the lower layers of the skin. Papules occur, for example, in acne.
- The nodus, or knot, is a circumscribed increase in substance in or under the skin. They are bigger than a papule.
- The urtica, or wheal, is a blurred flat elevation.
- The vesicle, or vesicle, is a fluid-filled cavity in the upper layer of the skin, the epidermis.
- The bulla, the bladder, is similar to a vesicle, only larger. These large, fluid-filled bubbles are often made up of small bubbles.
- The pustula is a sterile, yellowish collection of leukocytes (white blood cells) in a cavity in the epidermis (upper layer of skin). Pustules occur in psoriasis and acne, for example.
Secondary lesions
A brief overview of the secondary fluorescences:
- Squama, the scale, is characterized by an increased collection of horn lamellae. These dandruff occurs primarily in psoriasis.
- Crusta, the crust, is a layer of dried secretion.
- Cicatrix, the scar, is characterized by healing of a previous defect. The scar can be either atrophic (i.e. less tissue than before) or hypertrophic (with increased tissue growth).
- The rhagade, or fissure, is a gap-shaped crack that extends into the dermis. They are called fissures on non-keratinized skin / mucous membrane regions. They often appear in the corners of the mouth.
- An erosion (abrasion) is a superficial defect that heals without scars.
- An excoratio is a defect that extends into the dermis (lower layer of skin). Nevertheless, the excoratio usually heals without a scar. The defect is therefore deeper than with erosion.
- An ulcer or swelling describes a deeper defect that leaves a scar after it has healed.
- Atrophy is a shrinkage of tissue without a previous defect.
- A pustula (pustule) can also appear as a secondary fluorescence.
Classification of skin changes
The following is a list of the most common skin changes divided into:
- Skin changes in old age
- Benign changes in the skin
- Skin changes at different locations
- Skin changes in diabetes
- Skin changes after chemotherapy
Changes in the skin with age

Skin aging
With increasing age, the skin is subject to many remodeling processes. Skin aging starts noticeably as early as the age of 30.
Depending on which environmental influences the skin is exposed to, the aging process progresses faster or slower.
Accelerating skin aging are e.g. Nicotine consumption, increased exposure to UV light, as well as frequent exposure to chemicals and stress. These external factors, in combination with internal factors such as a slowed metabolism in old age and a decreased ability to regenerate, the skin ages.
You can find detailed information at: Skin aging
Skin folds
The water content of the skin decreases with the aging process. The skin becomes dry and less stretched. The fact that there is less fat directly under the skin also leads to the formation of wrinkles.
The skin becomes thinner, less elastic and also less supplied with blood. As a result, wounds heal more poorly than in younger people.
In addition, the structure of the glands in the skin area changes. Perspiration and sebum production decrease. This also leads to reduced skin resilience. It becomes more prone to cracks, injuries, and irritation.
Find out more about the topic here: Skin folds
Age spots
Age spots appear mainly on the face, on the forearms and on the back of the hands and thus in places that are particularly exposed to UV radiation.
It is a small, light brown, sharply delimited skin discoloration caused by the accumulation of so-called age pigment (Lipofuscin) arise. This pigment is produced when exposed to UV light and is usually cleared from the cells of the skin. With age, this mechanism is only functional to a limited extent, so that the age pigment remains in the skin and causes the typical spots. These are harmless, but should be examined by a doctor if they are suspected, as they can easily be associated with a malignant skin lesion (Lentigo maligna) can be confused.
You can find detailed information here: Age spots - where do they come from and what helps?
Age warts
Age warts, or seborrheic keratoses, are the most common benign skin tumors. They tend to develop on the back, arms and back of the hands.
Their appearance varies greatly. Some age warts are light brown, others almost black. Mostly they do not get bigger than 1 cm. They are sharply demarcated and usually grow raised, i.e. they extend beyond the normal skin level.
Age warts do not need to be removed. If necessary, e.g. if the wart is in uncomfortable places, it can be removed with a laser or a sharp spoon.
In some cases, age warts can be mistaken for malignant skin changes. Since malignant skin diseases also occur more frequently in old age, all skin changes should first be examined by a doctor.
Read more on the subject at: Age warts
Benign changes in the skin

Blisters, calluses and corns
Blisters, calluses and corns occur when there is mechanical damage to the skin. On the one hand, increased friction and pressure can lead to the upper layer of skin becoming detached from the lower one, which leads to blisters. However, the skin can also try to adapt to the new situation by reacting with increased horn formation. This creates calluses or corns.
Blisters, calluses and corns are often caused by new shoes or incorrect footwear as well as incorrect or overuse of the skin, which often occurs during sport.
Read more about the topic here: Blisters, calluses and corns
Warts
Warts are most commonly caused by human papillomaviruses, which lead to increased keratinization of the skin. Most often these vulgar warts are found on the hands and the soles of the feet. They can appear at any age and are transmitted through contact or smear infection. As a result, several family members are often affected at the same time. There are various options for treatment, which is the most suitable therapy for you; it is best to discuss this with your dermatologist.
In addition to the vulgar warts, which are by far the most common, there are dellar warts, genital warts or even age warts.
You can find detailed information at: Warts
Pigment disorders
The skin's color pigment, melanin, protects the deeper layers of the skin from UV radiation. A pigmentation disorder can arise either from the fact that melanin is produced more or less. The affected skin areas can be distinguished from healthy skin, as it appears either lighter or darker. The most important and most common pigment disorders are freckles, liver spots and age warts, which as a rule have no disease value. In the case of liver spots, for example, it is important to distinguish between congenital and acquired liver spots, since the congenital liver spots have an increased potential for degeneration. Pigment disorders also occur with melasma, vitiligo or albinism.
You can find detailed information at: Pigment disorders
Spider veins
Spider veins are the smallest form of varicose veins. However, spider veins are harmless and do not need to be removed. For cosmetic reasons, however, the spider veins can be removed with the help of different procedures and at the patient's request. However, since these interventions are usually not medically indicated, the costs are not covered by the health insurance companies.
Although spider veins are not dangerous in themselves, they can be a first indication of a disease of the deep veins or venous valves, so it is advisable to observe the course and, if necessary, to carry out an ultrasound examination.
Learn more about this at: Spider Veins - Causes and Treatment
Skin changes at different locations

Skin changes on the face
Skin changes on the face can be a variety of different symptoms and diseases. The best way to clarify which disease or cause is responsible for the development of the skin change is through a visit to a dermatologist. This can usually make a suspected diagnosis based on a look at the changes.
Skin changes on the face can be divided into different groups. For example, these can arise due to infections. Changes in the skin which occur as a result of the infection often show further symptoms such as an increased temperature. A number of different bacteria and viruses, as well as fungi, can cause such an infection. The well-known cold sore, for example, represents an infection-related change in the skin.
Certain fungi are also suspected to be the cause of the common seborrheic eczema of the scalp and face.
Since the skin on the face is usually not covered by clothing, there is higher UV exposure there than on the rest of the body. Changes that can occur due to UV radiation include sunburn as well as malignant diseases such as skin cancer.
Skin changes caused by side effects to medication are relatively rare, but quite possible. However, such a drug rash usually occurs on large areas and is not limited to the skin on the face.
Ultimately, allergies can also be the cause of a skin change. An allergy to certain care products or an overreaction of the body to actually harmless substances can play a role here.
You can find detailed information here: Skin changes on the face
Changes in the scalp
Changes in the scalp can have various causes. In most cases, skin changes that occur on the scalp are harmless phenomena that are easy to treat. In rare cases, however, it can be that a malignant disease is behind the skin changes which should be diagnosed and treated as quickly as possible.
Since the scalp is at a direct angle to the sun and thus to the harmful UV radiation, skin changes often develop here. In addition to sunburn, this also includes the development of skin cancer. Therefore, the scalp should always be examined during skin cancer screening, as otherwise skin cancer often goes undetected for a long time at this point.
But dandruff and so-called atheromas, benign growths under the skin, are common skin changes on the head.
In general, if skin changes occur quickly and for no apparent reason, as well as if existing marks on the skin change quickly, in the best case, a dermatologist should be consulted for clarification.
For more information on scalp changes, we recommend these articles:
- Pus pimples on the scalp
- red spots on the scalp
- Eczema on the scalp
- dry scalp
Skin changes around the breast
Skin changes that arise on or under the breast can have very different causes.
In general, any skin changes can occur on the chest, which also occur on the skin of the rest of the body. This can lead to changes caused by acne or UV radiation, as well as injuries and irritations, but also due to dangerous illnesses. In most cases, however, skin changes are harmless. Malignant diseases that show up as changes in the skin on or under the breast are primarily skin cancer and breast cancer.
Skin changes that occur under the breast are mostly due to dry and irritated skin. Such a cause is particularly likely if the skin under the chest is reddened and painful to the touch. The skin under the breast should, as it is often overlooked, also be checked regularly for skin changes.
Changes in the skin of the breast can also be an indication of the presence of breast cancer. Changes in the nipple in particular, such as retractions and color changes, are an alarm signal that should be urgently clarified. Even if bloody or clear secretions emerge from the chest, a doctor should be consulted for clarification. This also applies if an irritated and red skin does not heal for a long time or other skin changes occur within a short time.
Skin changes on the breast, however, rarely occur in the early stages of breast cancer. Regular checks by a treating gynecologist, who examines the breast for conspicuous lumps as an early indication of breast cancer, make sense.
In general, changes in the skin that only occur on one breast are noticeable and require clarification in any case.
If skin changes occur on or under the breast, it is always advisable to consult the attending physician. This can find out the cause of the skin change and, if necessary, rule out a dangerous disease. Depending on the symptoms, a general practitioner, gynecologist or dermatologist can be consulted. The individual prognosis for skin changes, whether malignant or benign, with a rapid diagnosis and an associated early start of therapy is always better than with a late diagnosis, which is why a visit to a doctor should not be avoided.
The investigation of local changes in the skin is usually carried out by taking a skin sample. More about this topic can be found: Skin biopsy
Skin changes on the back
Changes to the skin on the back can have many causes. The most common skin change in this area is the common birthmark or mole. Moles can be very different in size and color. Most of them are already present at birth or develop in the first months of life. In particular, moles that appear spontaneously, grow larger or change their color and texture should be medically assessed. These could be precursors to skin cancer.
Acne, probably the best-known skin disease, manifests itself in numerous reddened pus pimples and pustules, which can occur primarily on the face, décolleté, but also on the back. Since the skin on the back is particularly firm and resistant, acne can be very stubborn, especially there.
Lipomas can develop anywhere in the subcutaneous fat tissue. They are often located in the head and neck region, in the shoulder and back area. These are more or less hardened love handles that can be felt under the skin and have no disease value. They usually occur between the ages of 50 and 70. The lipoma can be clearly demarcated from the surrounding tissue. In most cases, lipomas are only superficial and rarely go deep.
Much rarer than the benign lipoma is the malignant liposarcoma, which, however, usually arises independently and does not arise from a lipoma.
Shingles is a viral disease caused by the varicella zoster virus (chickenpox virus). This leads to a burning, often itchy, blister-like rash that runs along nerve tracts and usually only occurs on one half of the body.
In most cases, the rash begins in the back area next to the spine and then spreads forward in a belt-like manner. Shingles usually originates in the back area, as the causative viruses are located in the ganglia of the spinal cord and trigger the infection from there. The viruses usually reach the ganglia after a chickenpox infection in childhood, where they persist and e.g. be reactivated if the immune system is weakened. This then manifests itself as shingles.
Reddish rash on the back is often caused by allergies or drug reactions. In principle, this type of reaction can cause a rash all over the body, but the trunk and back are preferably affected. A rash on the back usually manifests itself as red spots on the back.
Skin changes on the glans
Skin changes on the glans (medical: Glans penis) can have different causes.
The individual skin changes should be clarified by a dermatologist so that he can diagnose the underlying disease and initiate appropriate therapy. The most common reason for skin changes that appear on the glans is an infection with bacteria, fungi or viruses. Often these infections occur as part of a sexually transmitted disease. Redness can also occur if the skin is excessively irritated. In the case of an allergy, for example to the detergent, condoms (latex allergy) or care products used, irritation, pustules and redness can occur, which usually recede by themselves if you avoid the triggering substance. Infectious Fournier gangrene, which needs urgent treatment and is associated with a high mortality rate, can rarely occur.
Ultimately, penile cancer can manifest itself on the glans and lead to skin changes there. A dermatologist should always be consulted, especially if the skin changes on the glans over time or if it is dark or multicolored.
Read more on the topic: red spots on the glans, completely reddened or itchy glans
Skin changes in diabetes

In the context of diabetes (diabetes mellitus) skin changes are common. Different forms can be distinguished.
Diabetic dermopathy
Diabetic dermopathy is the most common skin change in diabetes mellitus. It occurs in up to 70% of diabetics. Red spots or blisters form on the front of the tibia, in particular, and the skin becomes flaky and parchment-like.
In addition, hair loss can occur in the affected areas.
Diabetic scleredema
This skin change occurs in 20-30% of diabetics. It is characterized by a waxy, painless remodeling of the subcutaneous tissue, especially on the back of the hand and fingers. This makes the skin firm, which leads to stiffness and restricted movement of the hands.
A special form is Buschke's diabetic scleroedema, in which the skin is remodeled due to increased sugar accumulation in the tissue. This occurs especially in poorly adjusted diabetics. The patients describe a feeling of tension and tightness in the skin. In addition, the skin has an unusual sheen and loses its natural texture and elasticity.
Necrobiosis lipoidica
This skin disease is characterized by an inflammation of the middle layers of the skin, in which more fat accumulates (hence "lipoidica" from the Greek lipos = fat).
Usually it occurs on the front of the lower legs. Initially, intensely red blisters usually appear, which over time expand to the size of the palm of the hand, sink into the tissue and develop into red-yellowish, slightly thickened surfaces.
The lesions are surrounded by a bluish, raised edge. In the worst case, the inflammation can cause tissue to die (necrosis). Overall, lipoid necrobiosis is rare. It affects about 0.3% of diabetics.
Bullosis diabeticorum
Bullosis diabeticorum is rather rare. These are blisters that appear spontaneously, mostly overnight, on the palms of the hands and soles of the feet, which heal on their own after about 2-4 weeks.
Read more on the topic: Rash on the foot
Pruritus diabeticorum
This skin disorder describes the severe itching on all skin areas, which often occurs in diabetics. It is caused by lack of fluids, diabetic nerve damage, reduced sebum production or secondary skin infections from frequent scratching.
Infections
Diabetics are generally more susceptible to skin infections of all kinds. Damage to the skin, for example through increased scratching, quickly leads to the colonization of pathogens (especially bacteria and fungi). These skin infections are also manifested in rashes and itchy skin changes.
Others
With diabetes there can be many different skin changes. There is increased reddening of the facial skin due to widened vessels (rubeosis faciei), yellowing of the fingernails (yellow nail syndrome), and white spots on the skin (vitiligo, white spot disease).
Skin changes after chemotherapy

chemotherapy
Chemotherapy is used to destroy degenerated cells. Since these tumor cells usually divide unchecked, chemotherapy is designed to destroy precisely these cells with a high division rate.
The disadvantage is that some healthy body tissues also have a high rate of cell division because they have to constantly renew themselves, e.g. the skin and oral mucosa, which are therefore also attacked by chemotherapy.
Cancer patients therefore often suffer from inflammation of the oral mucosa and gums, as well as all kinds of skin rashes during chemotherapy.
Most chemotherapy-induced rashes are reddened skin that appears all over the body (generalized rash).
The type of rash that develops also varies depending on the chemotherapy drug used. With some preparations, painful lesions can occur on the palms of the hands and soles of the feet (hand-foot syndrome). However, the rash usually subsides at the end of therapy.
radiotherapy
Radiation therapies are even more damaging to the skin than chemotherapy. This is because radiation therapy exposes the skin directly to the harmful radiation. In some patients, this manifests itself as a rash that can appear weeks or months after radiation therapy.
It can consist of red, scaly patches, accompanied by weeping blisters or skin thickening and itchy.
Other patients may also experience pigment spots or darkening of the skin in the irradiated area. In general, naturally fair-skinned people are more often affected.
Hair loss
The so-called skin appendages (hair and nails) are also severely affected by chemotherapy and radiation therapy, as they also arise from rapidly dividing cells. Hair loss and brittle nails occur. After the therapy, the hair usually grows back. In some cases, radiation therapy can cause permanent hairlessness in the irradiated area.
Prevention and Care
If possible, exposure to the sun should be avoided during chemotherapy / radiation therapy so as not to put additional strain on the skin. Adequate care of the skin is also recommended, for example with creams and ointments containing marigold (calendula).
Concentrates containing chamomile or sage are particularly suitable for mouth rinsing.













.jpg)