Cerebral hemorrhage
Synonyms
- ICB
- intracerebral hematoma
- intracerebral hemorrhage
- Intracerebral haemorrhage
- Cerebral hemorrhage

definition
Spontaneous intracerebral bleeding (ICB) is bleeding into the brain tissue (Parenchyma) that is not caused by trauma.
Intracerebral haemorrhage (cerebral haemorrhage) can be classified according to cause (medical etiology) and severity, as well as according to the location in the brain tissue.
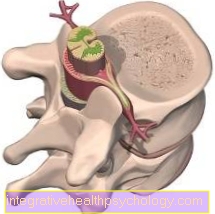
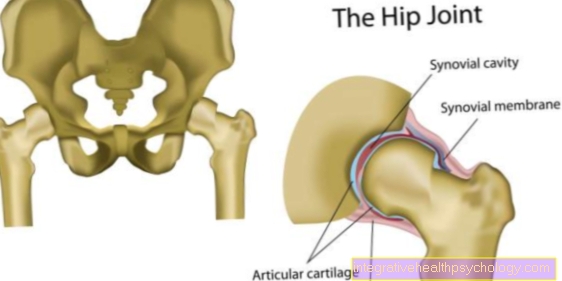
Illustration of a cerebral hemorrhage

Cerebral haemorrhage (cerebral haemorrhage)
- Skull roof -
Calvaria - Hard meninges (dura) -
Cranial dura mater
(outermost meninges) - Subdural gap -
Subdural space - Cobweb skin of the brain -
Arachnoid mater cranialis
(middle meninges) - External cerebral water space -
Subarachnoid space - Cerebrum covered by soft
Meninges (pia) -
Pia mater cranialis
(inner meninges) - bruise
(Hematoma) in brain tissue
Bleeding in the area of the brain tissue
and the meninges:
A - Intracerebral Haemorrhage (ICB) -
Bleeding into the brain tissue
(Parenchyma) by bursting a cerebral vessel
B - Epidural Bleeding -
Blood between the bones of the skull and the
outermost meninges (Dura mater)
C - Subdural Bleeding -
Blood between the meninges
and cobweb skin
D - subarachnoid hemorrhage -
Blood between cobweb skin and
the inner (soft) meninges
You can find an overview of all Dr-Gumpert images at: medical illustrations
Generic term circulatory disorders of the brain, classification
Disturbances of the cerebral blood flow, which are the most common cause of acute neurological deficits, are distinguished cerebral ischemia, i.e. under-supply of the brain, which, at 85%, is far more common among circulatory disorders of the brain than vascular (vascular) cerebral hemorrhages (15%).
A detached blood clot (Embolus), which is deposited in the brain vessels, inflammatory changes in the vessels (Vasculitis) or plaque deposits (arteriosclerosis) from the larger blood vessels can lead to the vessels becoming narrowed or clogged and the subsequent section not being adequately supplied with oxygen and nutrients (Ischemia).
This leads to the loss / death of the tissue. This is particularly dangerous in the brain because, on the one hand, important functions such as movement processes or memory performance fail and, on the other hand, the nerve cells cannot be reproduced, so that permanent damage can occur.
In the second group of cerebral circulatory disorders, a distinction is made between ICB and subarachnoid hemorrhage, i.e. acute hemorrhage in the space between the meninges filled with nerve water (liquor) (Meninges) surrounding the brain.
In contrast to cerebral haemorrhage, which will be discussed in more detail below, subarachnoid hemorrhage is caused by an accident (medical trauma) or a tear in an existing cerebral vessel enlargement (Aneurysm rupture) conditional.
Read more on this topic: Brain aneurysm
You can also find more information on the topic of subarachnoid hemorrhage.
What are the typical symptoms of a cerebral hemorrhage?
Cerebral hemorrhages are potentially life-threatening conditions that can arise due to various causes. They differ not only in their causes, but also partly in their symptoms. Depending on the type of cerebral hemorrhage, different symptoms that are characteristic of the cerebral hemorrhage emerge.
Read about this too What are the signs of a cerebral hemorrhage?
Symptoms of an intracerebral hemorrhage
Symptoms of intracerebral haemorrhage usually appear suddenly and differ depending on the location and size of the bleeding. From asymptomatic small microbleeds to mass bleeding with rapid death, the range of symptoms is wide.
The possible symptoms are often similar to those of a stroke. These include speech impairment, hemiplegia, and impaired vision. A look to the side of the bleeding is also typical. Furthermore, there may be nausea and vomiting, as well as difficulty walking and standing. Headaches and - in the early phase of the bleeding - epileptic seizures are also typical symptoms.
Extensive bleeding can also lead to severe loss of consciousness and a coma.
Symptoms of epidural bleeding
Epidural bleeding, which usually affects young people after an accident, for example when doing sports, leads to very typical symptoms.
Initially, there is usually a brief loss of consciousness. However, those affected usually regain consciousness quickly and then show no symptoms. Over time, however, the pressure in the brain increases due to the bleeding and leads to nausea, vomiting, restlessness and headaches. A renewed impairment of consciousness with an unconsciousness is typical. Hemiplegia can also occur.
Read more about this under Epidural bleeding
Symptoms of subdural bleeding
Subdural bleeding can have an acute symptomatic as well as a chronic course. Acute symptoms are indistinguishable from epidural bleeding and also lead to symptoms such as headache, nausea, vomiting and impaired consciousness.
Symptoms of chronic bleeding are more insidious and manifest as a general slowdown and impaired memory. Chronic subdural bleeding is therefore often easily overlooked, especially in older people.
Symptoms of subarachnoid hemorrhage
The dreaded bleeding through an aneurysm is also called Subarachnoid hemorrhage designated. Subarachnoid hemorrhage also occurs as a result of trauma, for example an accident, in only about 15% of cases. The annihilating headache, which owes its name to the intensity of the pain, is very typical of such bleeding. Sufferers describe this type of headache as a pain that they have never had before. It spreads over the entire head and can extend to the neck and back. Vomiting, nausea and sweating can also occur. In some cases there is little to no impairment of consciousness. In some cases, however, those affected immediately collapse unconscious. A wide variety of paralysis, speech disorders and neurological deficits are possible with such a bleeding. Epileptic seizures can also occur.
Read more about this under Subarachnoid hemorrhage
What is the difference between a stroke and a brain hemorrhage?
A stroke is an acute circulatory disorder in the arterial vascular system of the brain. In about 80 to 85% of the cases, an ischemic event, i.e. insufficient blood flow, is responsible for the stroke. The reason for this is usually the occlusion of an artery by a blood clot. Atrial fibrillation is a common disease associated with this.
However, in 15% of cases, a stroke can also be caused by intracerebral cerebral hemorrhage or subarachnoid hemorrhage. Strokes don't always show the same clear symptoms. One tries to categorize them symptomatically roughly according to the affected brain area. This must be distinguished from cerebral haemorrhage that occurs after an accident.
Read more about this under Stroke - What Are The Signs?
Epidemiology - How Frequently Does This Happen?
Spontaneous cerebral haemorrhage is the cause of a stroke in 15% of those affected. While men and women are affected about equally often, one can observe ethnic differences in the frequency.
In the white population, 15-20 people develop the disease annually per 100,000 population, compared with 35 per 100,000 Hispanic and African-American residents in the United States and as many as 60 new cases per 100,000 residents among the Japanese each year.
The likelihood of developing a brain hemorrhage increases with age.
Cause of a cerebral hemorrhage
There are several causes of spontaneous intracerebral bleeding.
The most important risk factor for ICB (intracerebral bleeding) is high blood pressure (Hypertension).
There is an additional risk when taking certain medications, such as the anticoagulants heparin or Marcumar (Anticoagulants), as well as therapies to prevent the formation or loosening of blood clots, as well as to dissolve existing blood clots (Thrombolysis), which are also used to treat a heart attack, or are taking aspirin, which prevents platelets from clumping together (Antiplatelet drugs) and is sometimes mistakenly called a blood thinner.
In addition to diseases of the blood-forming system and coagulation disorders, the risk factors include, above all, long-term alcohol or drug consumption, as well as the use of certain medications, e.g. certain antibiotics or painkillers.
On the other hand, common risk factors for heart and vascular diseases such as diabetes mellitus, cigarette smoking and elevated blood lipid levels do not play a major role in the development of intracerebral bleeding. The risk of bleeding can even be increased with low cholesterol levels.
Read more on the topic: What are the causes of a cerebral hemorrhage
An aneurysm is a spindle-shaped or sac-shaped expansion of a cerebral artery. They occur mainly on branching vessels and are more common in women than men. Aneurysms are dangerous because they can burst and cause cerebral haemorrhage. Such a cerebral hemorrhage is known as Subarachnoid hemorrhage.
This life-threatening bleeding is associated with a high mortality rate. Complications in the course of therapy are frequent and cause the poor prognosis. Significant risk factors for aneurysm bleeding are smoking, high alcohol consumption and untreated or uncontrolled high blood pressure. However, some people also have weak walls in their vessels, which is why aneurysms tend to develop. Unfortunately, to this day nothing can be done about this.
Read more about this under
- Consequences of alcohol
- Illnesses related to smoking
Bleeding in the brain after a fall
A Cerebral hemorrhage can occur due to different causes. A fall on the head is with one movement of the Brain connected within the skull. The movement can tear the blood vessels in the brain and cause bleeding. A cerebral hemorrhage as a result of a fall can generally happen to anyone.
However, there are some risk factors that significantly increase the likelihood of cerebral hemorrhage after a fall.
The use of blood-thinning medication poses a general risk of bleeding in the brain. For this reason, patients who take blood-thinning medication have an increased risk of developing cerebral haemorrhage after a fall.
A second risk group are people who are drunk. Since the protective reflexes normally present in drunken people are significantly reduced, the risk of falling unchecked on the head in the event of a fall is significantly increased. In addition, alcohol disturbs the sense of balance and makes a fall more likely.
How much do blood thinners increase the risk of cerebral haemorrhage?
As an undesirable effect, blood-thinning therapy increases the risk of bleeding in general.
Cerebral haemorrhages and severe gastrointestinal bleeding are particularly feared. About 15% of spontaneous intracerebral cerebral hemorrhages result from blood-thinning therapy. Therefore, blood-thinning therapy must always be carried out after weighing the risks and the hoped-for benefits.
Differentiation of the cerebral hemorrhage based on risk factors
The mass hemorrhage (hypertensive bleeding), which makes up 40% of ICB, occurs mainly in parts of the brain in which there are vessels with a rather thinner wall. By high blood pressure these wall sections can be changed over time, fat deposits and the formation of bulges or widening of the vessels (Microaneurysms).
In addition, if the blood pressure suddenly rises sharply, for example under stress, these vasodilatations can burst and lead to Cerebral hemorrhage, mainly in the area of the basal ganglia and the Thalamuswhich, among other things, make a significant contribution to the control of movement sequences and complex memory skills.
Likewise, especially in younger patients, it can be caused by congenital or acquired vascular malformations, e.g. malformations or benign neoplasms of Blood vessels (Angioma) bleeding in the brain.
In addition, there are diseases in which abnormally changed with increasing age Protein deposits (Amyloid) can lead to changes in the vessel wall in medium-sized arteries.
Certain malignant primary Brain tumors, as well as metastases of certain Tumors can bleed into brain tissue.
What are the typical signs of a cerebral hemorrhage
Most cerebral hemorrhages do not announce themselves in advance. They occur after serious accidents and injuries and therefore cannot show any signs. After an accident, a cerebral haemorrhage can never be safely ruled out based on the symptoms, which is why imaging should always be performed in the event of head injuries or whiplash injuries. This is the only way to safely see bleeding. Signs are impaired consciousness, headaches or even paralysis. For the examiner, unusual pupillary reflexes are also a strong sign of a cerebral hemorrhage.
A special feature is the subarachnoid hemorrhage, which is associated with a so-called warning bleeding in about 25% of cases (warning leak) goes hand in hand. This precedes the actual bleeding days or weeks and is accompanied by severe headaches. Most of the time it is not taken seriously by those affected, so that they do not see a doctor.
Consequences of a cerebral haemorrhage and the resulting symptoms
ICB leads to an increase in volume in the brain and an increase in intracerebral pressure (pressure in the brain).
First, the blood volume and the volume of the nerve water (Cerebrospinal fluid) lowered. In the long term, this can lead to a decrease in blood flow to the brain and thus to a reduced supply of oxygen to the tissue (Ischemia), causing additional damage to the nerve tissue.
Typically, symptoms such as:
- a headache
- Nausea and
- Vomit
suddenly appears as a sign of increased intracranial pressure.
Depending on the location of the bleeding, localized neurological deficits and / or impaired consciousness can also occur.
The neurological failure pattern often provides an indication of the location of the bleeding even without an imaging procedure.
The thalamus is partly responsible for the generation of muscle movements. If bleeding occurs in this area, symptoms of paralysis typically occur on the opposite side of the arms and legs or on the face.
Even with bleeding in the area of the basal ganglia, the initial symptoms are headache and vomiting, typically hemiplegia (Hemiparesis) on the opposite side and look to the affected hemisphere.
Another typical symptom of bleeding in the area of the basal ganglia of the dominant hemisphere of the brain (hemisphere) are language, reading and language comprehension disorders (aphasia).
Bleeding in the area of the cerebellum often leads to dizziness, unsteadiness of gait and unnatural, fast, directed eye movements (Nystagmus).
Bleeding of the brain stem is particularly dangerous, as vital centers for respiratory and circulatory regulation are located here.
Read more on the topic: Cerebral hemorrhage coma
It can also multilocular, i.e. several bleeding foci at different points in the brain with correspondingly diverse failures occur. They often occur in conditions with abnormal protein deposits (Amyloid angiopathy) or occur in coagulation disorders.
If the bleeding occurs in the nerve fluid (Cerebrospinal fluid) filled spaces (ventricles) collapse, there is a risk of developing nerve water congestion (Hydrocephalus occlusus), which can lead to a life-threatening increase in intracranial pressure.
For more information, read our topic: Cerebral hemorrhage symptoms
Cerebral hemorrhage and coma
A cerebral haemorrhage can cause a number of different symptoms.
A coma is a state of consciousness that occurs relatively frequently in the course of a cerebral hemorrhage. In a coma, the affected person can no longer be awakened even by a strong pain stimulus.
Generally it happens with one Bleeding in the brain to an increase in pressure and volume in the skull. Since there is only limited space available in the skull and this does not adapt to the size of the bruise, the pressure in the skull increases.
Due to the pressure increase, certain areas of the brain are typically pinched off as the bleeding progresses. In the course of this, the brainstem is very often trapped.
The brain stem is responsible for a number of important functions in the body. If this structure is trapped, it usually results in a Loss of consciousness as well as for Apnea.
A coma is a very serious symptom that can occur as part of a cerebral haemorrhage. It is usually an acutely life-threatening condition, as the coma is a sign of impairment of the cells of the brain.
diagnosis
Imaging tests are required to diagnose ICB. In the computed tomogram (CT), the position and size of the bleeding, as well as the increase in size (possible up to 30%) can be checked by another CT after 24 hours.
The MRI of the head (head MRT) and the MRI of the brain can also reveal bleeding, but they are second choice because of price, availability and the generally limited general condition of the patient.
Due to characteristic signal changes in the MRI of the head, older bleeding can also be detected, and vessels can be visualized using special methods in order to detect possible malformations or enlargements (MRI angiography).
Usually no additional laboratory diagnostic tests, such as an examination of the parameters of the nerve water (Cerebrospinal fluid), indexed.
MRI
In the acute diagnosis of cerebral haemorrhage, the first choice diagnostic tool is CT, as it can be performed very quickly and easily. This is the most effective way to obtain information in an emergency. However, the MRI is also an important diagnostic tool. The MRI can provide extended findings, particularly in the case of uncertain findings in the CT, symptoms that develop more slowly, or uncertain symptoms. Some of these are better suited to excluding other possible diagnoses. MRI is usually superior to CT, especially when chronic bleeding is suspected. Furthermore, the MRI is also used during the course to localize and map causes such as vascular changes, tumors and others.
Read more about this under MRI Or CT - What's the Difference?
OP for a cerebral hemorrhage
Cerebral haemorrhage is treated in different ways, depending on the location and extent of the bleeding. In addition to the possibility of influencing the course of the bleeding by administering certain drugs, neurosurgical surgery may be necessary.
Diagnostic imaging prior to surgery is essential as the location of the bleeding must be determined prior to surgery. Computed tomography can quickly provide a detailed picture of the injury and is therefore usually used in cases of cerebral hemorrhage.
Surgical removal of the bruise in the brain always involves opening the skull. In the case of superficial bleeding, it may be sufficient to open the skull at the point where the blood has accumulated. In some cases, the source of the bleeding must be found and stopped and the blood drawn using minimally invasive procedures. This can be done with the use of a robot or "by hand" be performed. Which methods are used in the individual case depends on the type of bleeding, the skills of the surgeon and the equipment of the hospital.
If an operation is necessary for a cerebral hemorrhage, this is usually performed within 72 hours of the occurrence of the bleeding and can improve the prognosis of the person concerned.
The main page on this topic can be found here: Operation of a cerebral haemorrhage
When do you need an operation?
Operations are not uncommon for cerebral hemorrhages, but not every cerebral hemorrhage has to be operated on per se. There are criteria that are used to decide whether a cerebral hemorrhage should be operated on or not. So-called epidural bleeding must always be operated on, as immediate relief of the brain must be guaranteed. Otherwise there is a risk of crushing and irreversible damage.
For bleeding aneurysms (Subarachnoid hemorrhage) the decision on surgical treatment of the aneurysm is made individually.There is also the option of using a catheter (interventional) to treat.
Subdural hematomas are treated surgically if there are symptomatic signs that intracranial pressure is excessively high or there are entrapment of the brain. A deterioration in the state of consciousness and the orientation of the person concerned also speaks for an operation.
In the case of intracerebral bleeding, it is always a matter of individual decision-making. Whether or not an operation should take place is always considered individually.
Cerebellar hemorrhages are usually more likely to be operated on.
Extensive bleeding into the ventricles of the brain is also a reason for surgery.
What is the therapy for a cerebral hemorrhage without an operation?
Surgical therapy does not make sense for every cerebral hemorrhage. In this case, conservative therapies are carried out, which have different goals and vary depending on the type of cerebral hemorrhage.
Severe intracerebral cerebral hemorrhage is treated in an intensive care unit. Usually those affected are ventilated and sedated. You will receive pain therapy and will be monitored. In addition, the blood pressure is set to a systolic value below 140 mmHg. Monitoring coagulation is an important goal. Anticoagulant drugs are stopped to prevent further bleeding. If necessary, coagulation factors are administered or drugs that counteract the effect of active agents that inhibit coagulation.
Another important goal is to lower intracranial pressure. Various therapeutic options are used for this purpose. Cerebral fluid or blood can be drained through a small tube in the ventricular system. This is known as external ventricular drainage. Medicines can also be administered to lower intracranial pressure.
Duration of an operation
The duration of an operation in the event of a cerebral hemorrhage cannot be given in general terms. There are several reasons for this. Cerebral haemorrhages are not all treated with one and the same operation, because firstly they can be of different nature and secondly also differ in their extent and localization. In most cases, however, operations lasting several hours can be assumed, as these are quite complex operations.
forecast
The prognosis of a cerebral haemorrhage depends on the current constitution and general condition of the patient, the pre-existing risk factors and the size, location and extent of the bleeding. While the prognosis is rather favorable for minor bleeding, the mortality rate is (mortality) overall for the ICB at 30 to 50%.
In particular, patients with large, extensive bleeding, advanced age, and multiple risk factors generally have a poor prognosis.
Even those patients who survive the bleeding and any secondary bleeding often suffer permanent damage, such as symptoms of paralysis or speech disorders.
What are the chances of survival after a cerebral hemorrhage?
Cerebral haemorrhages are very serious conditions that are potentially life threatening.
Depending on the type of cerebral hemorrhage, there are different chances of survival. There are cerebral hemorrhages with a comparatively good prognosis and others with a rather poor prognosis. A general survival probability cannot therefore be given.
Intracerebral bleeding, for example, is associated with a high mortality rate. About half of the patients die in the first year after the bleeding. On the other hand, there is the comparatively good prognosis of the epidural hematoma, with which there is a 70% chance of survival. The probability of survival depends heavily on the type of bleeding, the general condition of the person affected and the success of the therapy.
More about this topic can be found: What are the chances of survival in the event of a cerebral hemorrhage, What are the consequences of a cerebral hemorrhage
How good are the chances of recovery today?
Read more on the topic: What are the chances of recovery after a cerebral hemorrhage?
The term chances of recovery is very difficult for a cerebral hemorrhage. First of all, the primary goal is to ensure the survival of those affected, as these are usually life-threatening conditions. At the same time, of course, one tries to prevent consequential damage and to help those affected to return to their original state. However, this is highly dependent on the extent of the bleeding and the brain damage it caused.
Very extensive bleeding and accompanying injuries to the brain usually leave permanent neurological damage such as paralysis. With rehabilitation measures, however, one tries to improve the condition of those affected as well as possible. The supply options are very good due to specialized neurological and neurosurgical centers as well as adapted neurorehabilitation.
Cerebral hemorrhage in children
In general, older people are statistically more likely to suffer from cerebral haemorrhage than children. This is related to the increased tendency to fall in combination with frequent use of blood-thinning medication.
However, children can also suffer from cerebral haemorrhage. The reasons for the occurrence of cerebral hemorrhage in children vary widely. In addition to a fall or excessive force on the skull, certain clinical pictures can also be responsible for cerebral haemorrhage.
Cerebral hemorrhages caused by a pathological vascular structure often occur in childhood. The same is the case with bleeding, which occurs due to a congenital coagulation disorder.
Newborns, and especially premature babies, have an increased risk of developing cerebral haemorrhage. An increase in pressure, as it occurs in the course of a cerebral hemorrhage, can be caused by the touch of the in babies Fontanelles be checked.