Coronary heart disease (CHD)
Synonyms in a broader sense
Ischemic heart disease, coronary artery narrowing, Angina pectoris, Coronary syndrome, chest tightness, left pectoral chest discomfort
high blood pressure, Heart attack
English: coronary artery disease, coronary heart disease
definition
If there is a coronary heart disease (CHD) are the coronary vessels (Coronary arteries), through which the heart muscle is supplied with oxygen and nutrients, constricts. The blood flow in the coronaries is reduced, so that the heart is insufficiently supplied.
The most common cause of coronary heart disease in developed countries is that Atherosclerosis (so-called. Hardening of the arteries) of the coronary vessels. The vessel walls harden, the vessel loses its elasticity and the diameter of the vessel becomes smaller. Limiting blood flow leads to coronary insufficiency, i. the Coronary arteries can no longer meet the heart's need for oxygen; there is a disproportion between the supply and demand of oxygen Heart musclehence myocardial ischemia, i. a defect or Deficient oxygen supply to the heart, occurs.
.jpg)
Frequency of CHD and occurrence in the population
In the western industrialized countries, coronary heart disease and its consequences are the most common cause of death. The lifetime probability of developing CHD is 30% for men and 15% for women.
Chest pain (angina pectoris) or a heart attack are often the first symptoms of coronary artery narrowing.
causes
Coronary artery disease occurs as part of a multi-causal disease process. This means that the development of the disease is conditioned by various causes. The so-called cardiovascular risk factors play an important role in this.
Smoking, being overweight, diabetes mellitus and high blood lipid levels increase the risk of developing coronary artery disease. Calcification of the arteries (this is known as arteriosclerosis) is considered to be the main cause of the disease. With CHD, the heart vessels eventually narrow. Coronary arteries are blood vessels that lie around the heart like a wreath and supply it with oxygen. The narrowing of the heart walls is caused by deposits of fat and calcium, the so-called plaques. Because of these constrictions, the affected parts of the heart can no longer be adequately supplied with oxygen. This is often particularly pronounced under physical exertion and symptoms arise.
You can find out more about the topic here: Cause of coronary artery disease
Typical risk factors
-
Smoke
-
Little movement
-
Unhealthy diet
-
Obesity
-
Permanently high blood lipid levels (especially high LDL cholesterol and low HDL cholesterol)
-
Diabetes (diabetes mellitus)
-
High blood pressure (arterial hypertension)
-
Stress, emotional strain
-
Increased age
-
Hereditary predisposition to hardening of the arteries (arteriosclerosis)
You might also be interested in: Diet for heart disease
What role does alcohol play?
Alcohol consumption is generally not prohibited in coronary heart disease. A moderate consumption of 1 to 2 glasses of wine or beer occasionally is to be agreed with the illness. Increased consumption of alcohol does not lead directly to a heart attack, but is still unhealthy.
Alcohol promotes the development of obesity and influences some medications.
Some scientists recommend occasional alcohol consumption as it lowers cardiovascular risk. One speaks of 25 grams for men and 15 grams for women per day, although you should by no means drink every day.
Symptoms
Angina pectoris
Angina pectoris is the typical symptom of coronary heart disease (anginal complaints). The usually dull, pressing pain is localized by the patient behind the breastbone and often extends in a ring around the chest. Often the patients report a radiation of pain in the arms, mostly in the left arm. In women, pain in the upper abdomen occurs more often than in men, which can be misunderstood as gastrointestinal complaints (gastrointestinal complaints).
There are two forms of angina pectoris:
- Stable angina pectoris: The symptoms occur regularly and after certain loads or activities and last a few minutes. Physical and emotional exertion, cold or a full stomach can be trigger factors.
The pain subsides quickly after the administration of medication (nitro preparations) and / or during physical rest and has a constant intensity from attack to attack. - Unstable angina pectoris: This form of chest pain, which occurs due to an insufficient supply of the heart muscle with oxygen, is also referred to as pre-infarct syndrome and combined with acute myocardial infarction to form the coronary syndrome.
The pain of unstable angina is more pronounced than that of stable angina pectoris and can also occur during rest. It is also possible that an unstable angina will develop from a stable one. The unstable pectanginal complaints are less easy to deal with with medication than with the stable form of angina. Often the intensity, frequency and duration of the pain attacks increase as the coronary disease progresses.
In 20% of the cases, the unstable angina turns into a heart attack, which is why inpatient monitoring and examination of the patient is necessary: A heart attack must be ruled out by diagnostic measures, as this alone cannot be differentiated from unstable angina pectoris due to similar clinical symptoms is.
Classification of angina pectoris:
The Canadian Cardio-vascular Society classifies exercise-dependent angina pectoris into four grades:
- Grade I: The patients have no complaints under normal stress. These occur with very strong or prolonged exertion.
- Grade II: The anginal complaints affect the patient only moderately in normal activities.
- Grade III: The patient's performance is clearly restricted due to the chest pain.
- Grade IV: The patient is considerably limited in his performance and feels pain with every physical exertion or even at rest.
This classification is used to classify and assess the angina pectoris pain in the patient.
Read more on the topic: Symptoms of a heart attack
Chest pain
Coronary artery disease can cause chest pain, especially behind the sternum, which often radiates to the neck, jaw, arms, or upper abdomen. Most of the time it is a seizure-like tightness in the chest that occurs under physical exertion or stress.
This chest tightness is called angina and it is the cardinal symptom of coronary artery disease. It occurs when the heart is briefly less well supplied with blood through the vascular constrictions.
Also read our article: Chest pressure- what to do
Shortness of breath
In addition to chest pain or chest tightness, various non-specific symptoms such as shortness of breath can occur in coronary heart disease. With shortness of breath (dyspnea), those affected suffer from a feeling of difficulty breathing and shortness of breath. The shortness of breath is often accompanied by fear of suffocation, which can panic those affected.
If there is pronounced shortness of breath with a diagnosed CAD, the heart should be examined thoroughly.
Heart failure is a complication of CAD and can cause shortness of breath.
You can find more information on the topic here: Difficulty breathing due to a weak heart
A thorough investigation is necessary in order to adapt the therapy accordingly and to alleviate the symptoms as much as possible.
What is the life expectancy with coronary heart disease
Life expectancy with coronary artery disease (CHD) depends on many factors. The number of coronary arteries affected and the location of the bottlenecks are essential for the prognosis (prognosis of CHD). Depending on where the vessels that supply the heart with oxygen are narrowed, different parts of the heart are affected by the disease. Depending on the location of the bottlenecks, the cardiac conduction system, for example, can be affected, which has a strong impact on life expectancy.
How far the coronary heart disease has progressed is also decisive for the prognosis. The presence of other diseases such as diabetes mellitus or circulatory disorders are also crucial for life expectancy.
It is important to recognize the disease at an early stage and to treat it specifically. This results in a good prognosis and you can avoid complications of CHD such as a heart attack and heart failure. The long-term prognosis for coronary artery disease depends on how the patient changes his lifestyle. The risk factors for CHD should be reduced as much as possible and plenty of exercise and a healthy diet are the basic rules.
Obesity and nicotine consumption should be avoided and medication prescribed for the disease should be taken regularly. There are various therapy options for coronary heart disease, which usually lead to good results and can enable patients to lead a long, symptom-free life.
Read more on the topic: Life expectancy in coronary artery disease
General therapeutic approaches
Coronary heart disease is a disease that cannot be cured. But with targeted therapy you can live well with the disease.
The therapy of CHD has two goals:
1. Relieve discomfort
2. Prevent dangerous complications.
In order to prevent the progression of the disease, every therapy includes a change in lifestyle. This includes a lot of exercise, a healthy diet and not smoking.
The use of medication is usually recommended even when there are no symptoms in order to counteract the progression of the disease. Depending on the severity of the disease, medication alone may be enough to treat CHD. There are also homeopathic approaches (homeopathy for CHD). However, if the symptoms cannot be sufficiently relieved with medication, there are other therapeutic options.
The CAD can also be treated surgically with so-called stents or a bypass operation. Stents are thin tubes made of wire mesh that keep the constricted blood vessels open permanently. In a bypass operation, a body's own blood vessel or artificial tissue is used to bridge the gap.
Here you will find information on the topic: Therapy of CHD
Medication
There are drugs that are prescribed as standard for coronary artery disease because they have a positive effect on the progression of the disease. These include the antiplatelet drugs and statins.
The antiplatelet agents prevent platelets from attaching to the walls of the coronary arteries and causing plaques to form. Examples are drugs with active ingredients such as acetylsalicylic acid (Aspirin® protect 100), clopidogrel, prasugrel or ticagrelor. Some studies have shown that these drugs can help prolong your life and prevent complications such as heart attacks.
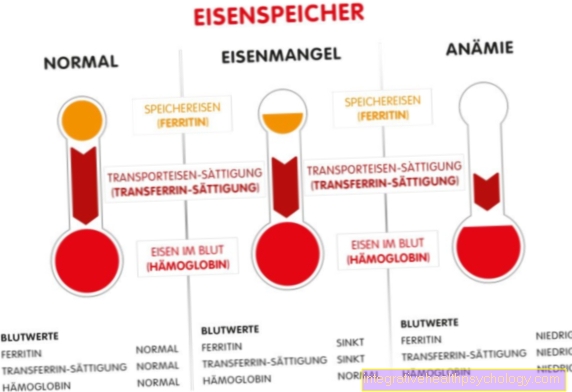
Statins (for example simvastatin) are drugs that ensure low blood lipid levels. They are also known colloquially as cholesterol-lowering drugs and they reduce the amount of cholesterol that is ingested from food entering the bloodstream.
Depending on the symptoms and other illnesses, other medications such as beta blockers or ACE inhibitors can be used.
Statins
Statins are drugs that lower blood lipid levels by inhibiting HMG-CoA reductase (a metabolic enzyme that is required for the formation of cholesterol). One of the most important risk factors for coronary artery disease is high cholesterol. More precisely, an increased LDL level triggers CHD. The LDL attaches itself to the vessel walls and leads to the deposition of other cells there. In the course of the process, calcifications form in the places, the vessel is narrowed. Statins can counteract this development by inhibiting the formation of LDL.
ASS
ASA is the abbreviation for acetylsalicylic acid, also known as aspirin, and is by definition a pain reliever. In addition to the pain-relieving effect, however, it also has a blood-thinning effect, which is why it is suitable for the treatment of coronary heart disease (CHD).
So-called thrombocytes are activated in the body to help blood clot in injuries. These attach to each other and so stop the bleeding. ASA acts on the platelets and inhibits their aggregation (= sticking together). In CAD, there are constrictions in the coronary arteries. The blood is diluted with drugs such as ASA so that blood clots do not form in these areas and then enter the brain, for example.
When do I need bypass surgery?
A bypass operation is intended to promote blood flow in endangered heart muscle areas in the case of CHD with the help of diversion bridges, the bypasses. These diversions lead the blood around the vascular constrictions so that the affected heart muscle areas are well supplied with blood with a bypass.
The indication for a bypass operation for symptomatic coronary artery disease exists above all when the vascular constrictions are in anatomically unfavorable places, for example very close to a vascular outlet or vascular sites that branch. Patients who suffer from diabetes mellitus or renal insufficiency in addition to CHD are more often sent for bypass surgery than for stenting because of the complex vascular constrictions.
As a rule, coronary bypasses eliminate the angina pectoris caused by CAD and significantly extend survival.
Stent
A stent is a small round wire mesh that can be used to treat coronary artery disease (CHD). A CHD is characterized by the fact that the coronary arteries are narrowed in some places. This means that not enough blood can flow through and the tissue behind is undersupplied.
A stent can be used to widen the constriction again. This is usually brought to the heart through a catheter. The catheter is advanced either through a vessel in the groin or through a vessel on the forearm to the heart. On site, the stent can be placed precisely at the previously diagnosed bottleneck.
During the procedure, the location of the stent can be checked with X-rays. Once the stent has been placed in the vessel, it is inflated with a small balloon so that it rests against the vessel wall. Due to the solid wire mesh of the stent, the vessel can usually not constrict again at this point. To increase the effect even more, there are stents that are coated with special substances. These should prevent calcifications from forming again.After the stent has been inserted, additional drug treatment with blood thinners such as ASA or clopidogrel must be carried out. This will prevent blood clots from forming.
When do i need a stent?
In addition to bypass surgery, a stent is an option for patients with coronary heart disease under certain conditions. A stent is a small, tubular metal mesh that is inserted into the affected vessel to keep the vessel open. There are stents that are drug-coated and have anti-inflammatory and growth-inhibiting drugs on them so that the vascular tissue does not proliferate, as well as stents without drugs.
In the case of drug-free stents, the cardiac patient must take anticoagulant drugs such as acetylsalicylic acid (Aspirin® protect 100) or clopidogrel for at least one year.
A stent can be used in patients in whom the vascular stencils are located more simply, in straight sections, not directly at branches and vascular outlets. A stent is usually only inserted in symptomatic coronary artery disease when symptoms affect the quality of life.
What is the course of CHD?
Coronary artery disease can take different courses. The most common symptom is chest pain (angina pectoris), which occurs like a fit. Other non-specific symptoms can vary in severity, such as shortness of breath, drop in blood pressure, increased pulse, pale skin, nausea, sweating or upper abdominal pain.
With CAD it can even be that the symptoms are completely absent, then one speaks of CAD with silent myocardial ischemia. This form is common in the elderly and diabetics.
In the classic course of CHD, the symptoms only occur in the initial stage when the heart's need for oxygen is increased, i.e. during exercise or stress. If the disease progresses and the blood vessels deteriorate, the symptoms can occur more frequently.
If coronary artery disease is untreated, serious complications can occur, such as heart failure and the dreaded heart attack. In the context of a dangerous heart attack, all forms of cardiac arrhythmias can occur, which can be fatal. In the chronic course of CAD after a heart attack, those affected suffer from cardiac insufficiency and recurring dangerous cardiac arrhythmias. In order to have a positive influence on the course and prognosis, it is important to diagnose coronary artery disease as early as possible and to treat it in a targeted manner.
Can you do sports with a CHD?
Patients with coronary artery disease can and should exercise. A lack of exercise is a risk factor for the development and progression of CHD. If you exercise regularly and sufficiently, you slow down the worsening of the disease and complications such as heart failure and heart attacks.
Endurance sports are good for those affected, for example cycling, walking, jogging or swimming. It is advisable to initially perform these activities at low to moderate intensity. You can also do strength training to build up individual muscle groups. The intensity and frequency of training should be discussed with the attending physician beforehand.
Ball sports are less suitable for patients with coronary artery disease, as the players quickly become "too ambitious" and absolutely wanted to reach the balls, even if they overloaded themselves.
Is CHD inherited?
Coronary heart disease is not inherited in the classic sense. However, there is a familial risk if one or both parents also developed vascular disease under the age of 60. The vascular calcification (arteriosclerosis) plays an important role here, as it is a major risk factor for the development of coronary heart disease.
Division into asymptomatic and symptomatic CHD
The insufficient supply of oxygen to the heart muscle cells (myocardial ischemia) manifests itself in various forms:
- Asymptomatic CHD, also called silent myocardial ischemia: The patient does not feel any symptoms.
Some patients with coronary artery disease, especially those with diabetes mellitus and smokers, experience painless angina attacks. Although the heart muscle is insufficiently supplied and there is insufficient oxygen available, the patients do not feel any tightness in the chest. This clinically silent form of CHD can lead to cardiac insufficiency (heart failure), sudden cardiac death or cardiac arrhythmias, despite the lack of symptoms. - Symptomatic oxygen deficiency (ischemia) causing symptoms:
- Angina pectoris (the terms chest pain, "tightness of the heart", "tightness of the chest" are used synonymously)
Complications
Sudden cardiac death
Coronary artery disease is present in over 80% of patients who experience sudden cardiac death. About 25% of patients with CHD die of sudden cardiac death as a result of cardiac arrhythmias.
Heart attack
Heart attack is a dreaded complication of coronary artery disease. In the context of CHD, the coronary vessels change pathologically. Plaques form in the interior of the vessels (vascular lumen) and the blood flow deteriorates in the affected areas. It can happen that the vessel wall tears and small blood clots form. These blood clots can block a coronary artery and cause a heart attack.
To avoid a heart attack, it is important to treat coronary artery disease as early as possible and to take the medication regularly.
Also read our topic: Signs of a heart attack
Cardiac arrhythmia
Many cardiac arrhythmias are associated with coronary artery disease. The beating rhythm of the heart can be slowed down (bradycardiac arrhythmia) or accelerated (tachycardiac arrhythmia).
Heart failure
If there is a permanent insufficient supply of the heart muscle and muscle cells have possibly perished, the heart's function may be restricted: As a suction-pressure pump, it maintains the blood pressure in the vascular system through its regular beating and ensures the blood flow (perfusion) to all organs - lies If there is a coronary artery disease with narrowed vascular lumens, the supply of the heart itself is inadequate and the pumping capacity is insufficient (insufficient).
You can find more information on this topic under our topic heart failure.
Diagnosis
How is CHD diagnosed?
A cardiologist diagnoses and treats coronary artery disease. Your family doctor is also a point of contact, especially for the first signs and suspicions of ischemic heart disease. First of all, a detailed anamnesis is important. In this doctor-patient conversation, the previous history, family illnesses and current complaints are thoroughly discussed.
A physical examination can identify risk factors for CHD and monitor the heart. A laboratory test is carried out routinely and can, for example, prove a past heart attack. In order to diagnose coronary artery disease, imaging procedures are necessary, which show the blood flow to the heart.
If CHD is suspected, EKGs are first written, once at rest and once under stress, for example on a bicycle ergometer. Coronary disease can still be normal on the ECG. Therefore, more examination methods are usually necessary to diagnose the disease. A heart ultrasound exam can be done to check the chambers of the heart, valves, and blood flow. With this technique, you cannot see the coronary arteries, but you can draw conclusions about the blood flow due to the movement of the muscle.
A myocardial scintigraphy is an examination that can also be performed at rest and under stress. In scinitgraphy, a weakly radioactively marked substance is injected into the patient's vein, which, among other things, accumulates in the coronary arteries. The radioactive radiation can then be displayed on images and any vascular constrictions in the coronary arteries can be detected. This method usually gives better results than the ECG.
An important examination for the diagnosis of CHD is the coronary angiography, also called cardiac catheter. This examination method can also be used therapeutically, for example to insert a stent.
In some cases, additional imaging methods are necessary to determine the severity of the CHD, for example PET, CT and MRI.
What changes does coronary artery disease make on the EKG?
In affected patients with coronary artery disease, electrocardiograms (EKGs) are written at rest and under stress:
- the resting ECG, in which the patient is at rest, is normal for most of those affected.
- During exercise, for example on a bicycle ergometer, when the heart consumes more oxygen and the coronary arteries cannot meet this requirement, the ECG changes particularly when the disease has progressed significantly.
ECG changes usually only show up when the coronary arteries are constricted by at least 50 - 70%. In most cases, more tests are needed to diagnose the disease and its severity.
The cardiac catheter examination
Cardiac catheter angiography is an examination in which the coronary arteries are x-rayed to identify narrowed vascular sites. The examination is invasive because a catheter is advanced through the inguinal artery or arm artery and into the coronary arteries.
The catheter is a very thin, long tube through which a contrast medium is injected into the coronary arteries to make them visible. Small changes in the x-ray can indicate advanced stages of CAD and damage to the vascular wall.
Alternative causes
Exclusion diseases for CHD (differential diagnoses)
Chest pain is characteristic of CAD, but it also occurs with other diseases that are not limited to the heart.
Cardiac pain caused by the heart can Cardiac arrhythmias occur with a fast heartbeat or with a Myocarditis occur. Is the patient in a High blood pressure crisis (hypertonic crisis) with very high blood pressure values, there is often severe pain in the chest area. Valvular heart disease are often accompanied by chest problems.
Reasons for Chest painthat are not related to heart disease may be in the area of the lungs: One Pneumonia (Pleurisy) causes severe pain and a reduced general condition of the patient, as in coronary heart disease or an angina pectoris attack. A Pulmonary embolism, the occlusion of a pulmonary artery by a loosened thrombus, for example from the venous system of the legs, causes severe chest pain and is an important differential diagnosis for CHD and myocardial infarction.
A dissection (bulging) of the main artery (Aortic aneurysm) or one Inflammation in the mediastinum (middle area of the chest) are other possible causes of pain.
Is there a Reflux disease and if the patient has acid regurgitation, symptoms such as burning sensation behind the breastbone can occur, which can be interpreted as angina pectoris pain. An endoscopic examination of the esophagus and gastric entrance is used to diagnose the gastro-oesophageal Reflux.
A acute pancreatitis (acute pancreatitis) is a disease of the upper abdomen and causes severe, ring-shaped radiating pain in the area of the Rib cage (thorax). Pancreatitis can be confirmed by determining lipase and amylase, two pancreatic enzymes in the blood.
Pain comparable to an angina attack can also be caused by a Biliary colic caused. Lock here Gallstones (Cholecystolithiasis) or smaller concretions of the gallbladder duct, so that a biliary backlog with inflammation of the gallbladder (cholecystitis) occurs. This inflammation is extremely painful and it can cause pain to radiate into the skin Rib cage area come.
anatomy
The heart itself becomes through the Coronary arteries (Coronary arteries) supplied with oxygen and nutrients. They arise from the aorta
( artery) and fill with blood during the relaxation phase of the heart, in diastole.
The right coronary artery (Coronary aria) starts on the right side of the aorta and runs first on the front of the heart to finally reach the back of the heart as the Ramus interventricularis posterior. It extends to the apex of the heart.
The left coronary artery arises on the left from the aorta, runs to the front of the heart and divides into the circumflex branch, which extends to the diaphragm facing heart surface extends, and the Ramus interventricularis anterior.
The right coronary artery supplies the right atrium (atrium) and the right heart chamber (ventricle), the posterior section of the heart septum (septum interventriculare), the sinus and the AV node that generate the heartbeat.
The left coronary supplies the left atrium, the left ventricle, much of the cardiac partition, and a small portion of the anterior wall of the right ventricle.
There are different coronary supply types.
For most people (60-80%) the so-called balanced or normal supply type in which the above-mentioned supply situation prevails through the coronary arteries.
At the Legal type, which occurs in 10-20% of people, the supply of the heart by the right coronary predominates, i.e. it also supplies large parts of the left heart.
Lies a Left type before, which is also the case in 10-20% of people, the area covered by the left coronary artery is larger than the area covered by the right coronary artery.
These anatomical features are in case of one Coronary arteriesclosure is of crucial importance for the therapeutic procedure.
Illustration heart
_2.jpg)
- Right atrial -
Atrium dextrum - Right ventricle -
Ventriculus dexter - Left atrium -
Atrium sinistrum - Left ventricle -
Ventriculus sinister - Aortic arch - Arcus aortae
- Superior vena cava -
Superior vena cava - Lower vena cava -
Inferior vena cava - Pulmonary artery trunk -
Pulmonary trunk - Left pulmonary veins -
Venae pulmonales sinastrae - Right pulmonary veins -
Venae pulmonales dextrae - Mitral valve - Valva mitralis
- Tricuspid valve -
Tricuspid valva - Chamber partition -
Interventricular septum - Aortic valve - Valva aortae
- Papillary muscle -
Papillary muscle
You can find an overview of all Dr-Gumpert images at: medical illustrations















.jpg)