Air embolism
Definition - what is an air embolism?
Air embolism is the narrowing of a vessel due to the accumulation of air, up to and including a vascular occlusion. Normally, our body absorbs small accumulations of air without any health consequences.
An air embolism becomes dangerous when there is a large amount of air in the right ventricle and the heart pumps less effectively. A distinction is made between arterial and venous air embolism.

Causes of an air embolism
The prerequisite for the development of an air embolism is that air can find a way to get into a vessel. Medical interventions are characteristic causes. A typical cause is an open IV access (intravenousinto the vein) or an infusion system.
You might also be interested in this topic: Phlebitis
If a three-way valve is opened at one of these accesses to a venous vessel and the infusion system is decoupled, air can enter. There may also be a leak in the infusion system or access due to a defective product or damage to the product. If air enters a vein via one of these routes, the amount of air depends on the patient's position and the height of the vein in relation to the height of the heart.
Another typical cause of the development of an air embolism is incorrect filling or insufficient venting of the infusion system. In addition, parallel infusions can be the cause of an air embolism. Parallel infusions, in which, for example, gravity infusions and infusion pumps influence each other because they are connected, it can lead to a pearl-string effect, i.e. liquid - air - liquid.
An air embolism can also develop if a port catheter or central venous catheter is used carelessly or if a leaky catheter draws in air. All catheter examinations (e.g. cardiac catheter examination) carry the risk of an air embolism.
Other possible causes include injury to larger veins, a pneumothorax, and the birth process.
The consequences of air embolism depend on how much air gets into the bloodstream.
Air embolism from an infusion
An infusion is a common cause of air embolism. An open infusion system can cause air to enter the vein due to an open three-way stopcock, decoupling in the infusion system, or a leak in the system.
An air embolism by infusion can also occur if the infusion system has either not been properly filled or has not been adequately vented. Parallel infusions have an increased risk of causing an air embolism because the two infusions influence each other.
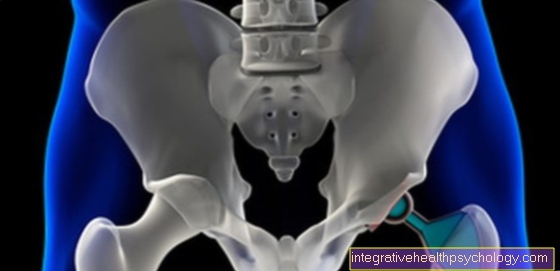
Air embolism during the birth process
Childbirth carries the risk of amniotic fluid embolism. Amniotic fluid gets into the maternal organism via the uterus or placenta and causes embolization.
The risk is present when labor is induced and is increased in the case of complications such as a uterine rupture, a tear in the cervix or a high vaginal tear.
Other risk factors such as maternal age> 35 years, previous caesarean sections, or multiple pregnancies increase the risk of embolism.
Read more on the topic: Childbirth complications
diagnosis
The clinical symptoms play an important role in the diagnosis of air embolism. If there is a temporal connection with a medical procedure, infusion, catheter examination or the like, this must be reported.
An air embolism can be detected directly with the heart ultrasound device. Often there are changes in the ECG (electrocardiogram) that resemble a heart attack.
In most cases, the blood gas analysis shows a decrease in the oxygen content.
Concomitant symptoms
If an air embolism develops, there are certain symptoms that can appear individually or together. A strong cough and pain when breathing or even shortness of breath are possible symptoms.
Often there is also accelerated breathing, Tachypnea. Those affected can Syncope (Circulatory collapse, short-term loss of consciousness) and anxiety and panic. Sweats often occur.
If the air embolism occurs in a cerebral vessel, neurological failures are to be expected. The symptoms can then be similar to a stroke.
You might also be interested in this topic:
- How can you recognize a pulmonary embolism? What are the typical signs?
- Circulatory disorder in the brain
How quickly do symptoms occur after an air embolism?
In most cases of air embolism, the symptoms appear immediately after the accumulation of air has entered the vessel. The consequences of an air embolism depend on the volume of air and the speed at which the air is infused.
How much air do you need for an air embolism?
In general, any amount of air entering the vessel must be viewed extremely critically. The consequences are strongly dependent on how much air enters, at what speed and what the condition of the person concerned is.
Smaller accumulations of gas in the veins are absorbed in most cases.
It becomes dangerous when there is a large amount of air (> 100 ml air) in the right ventricle. A gas supply of more than 100 ml of air per second or more is usually fatal.
Significantly smaller amounts of air are threatening in the arterial system. Just 2 ml of air in the cerebral arteries can lead to a stroke and just 0.5 ml of air in the coronary arteries can lead to a heart attack. The amount that is needed for an air embolism depends on the location and the vessel (artery or vein).
Therapy of air embolism
In the therapy of air embolism, the immediate measures are important and can save lives. The first measure is to eliminate the cause of the air embolism. A further inflow of air into the vessel must be prevented.
Depending on the extent of the air embolism and the symptoms, it may be necessary to ventilate the patient. A central venous catheter can sometimes be used to draw air from the right atrium.
One method of treatment is compression therapy with bandages, stockings, depending on the location and cause of the air embolism. The Durant maneuver can help prevent progressive embolization of the lungs. As part of this positioning, the patient is placed on his left side with his head down.
Read more on the topic: Compression bandage and compression stockings
Depending on the symptoms, it may be necessary to take measures to stabilize the circulation (medication, shock storage). Resuscitation may be necessary if necessary.
What are the emergency measures?
As an immediate measure, the cause of the air embolism must be prevented, i.e. the further influx of air into the vessel must be prevented.
If the air embolism is severe, immediate ventilation of the patient may be necessary. To prevent further embolization of the lungs, the Durant maneuver can be helpful. In this position, the person concerned is placed on the left side with the head down. The goal is to keep the air in the right ventricle and not reach the pulmonary vessels. Resuscitation may be necessary in severe cases.
Duration vs. forecast
The prognosis and duration depend on the time of diagnosis and treatment.
If air embolism is diagnosed immediately and treated in a timely manner, those affected have a favorable prognosis. In many cases the embolism regresses completely. Some patients retain symptoms like Paresis (Paralysis) or lung disease.
If air embolism is detected late, the chances of dying from it are very high.










.jpg)