Lymphedema
definition
Lymphedema is not a disease in itself, but a symptom of many other diseases. It is an underactive lymphatic system. The lymph can no longer be completely removed and accumulates in the tissue. The lymphedema is chronic in the affected area.
The causes can be diseases, but also surgical interventions and malformations. As a preventive measure, those affected can wear compression stockings and should avoid anything that leads to lymph formation.

The reasons
The causes of lymphedema can be used to divide lymphedema into a primary and a secondary form.
The primary form is very rare and describes a congenital form in which parts of the lymph vessels are not created. This also includes Milroy and Meige diseases. A complete absence of the lymphatic system is incompatible with life.
The secondary form describes all other causes of lymphedema that have in common a mechanical, acquired drainage disorder. Tumor diseases of the lymphatic system or surrounding tissue can be an obstacle to drainage. Mechanical obstacles can also arise from injuries or operations. Lymphedema is particularly common when the tumor is removed, as parts of the lymphatic system are often also removed. Chronic underactive veins can also result in impaired lymphatic drainage. A special form of lymphedema is elephantiasis, a disease caused by parasites. Elephantiasis is a tropical disease and does not normally occur in Europe. Lymphedema can also occur in conjunction with other edema.
Find out all about the topic here: Causes of Edema.
Radiation as a possible cause
Lymph vessels can be damaged by radiation as part of tumor therapy. In most cases, this is not the sole cause of lymphedema.
The drainage pathways can already be restricted by the tumor itself, so that the radiation is an intensifying factor. People who have Hodgkin's disease are more likely to have lymphedema from radiation.
The stages of lymphedema
Stage 1
Lymphedema can be divided into three to four stages, with stage zero showing no symptoms.
The first stage is a completely reversible edema, which occurs during physical exertion and usually only appears in the afternoon to evening. The lymphedema is very rich in protein and still soft. The affected areas can be pressed in with the fingers and the impressions remain briefly visible.
The mobility of the joints can be restricted and sufferers report sensory disturbances and dullness. Fibrosclerotic - scarred and hardened - changes in the tissue are usually not yet present or only locally limited.
Elevation at night can make the swelling go away. Depending on the cause, certain parts of the body are affected. With early therapy, a further development of the lymphedema of the first stage to the next stage can be prevented. People who discover these symptoms should seek medical advice as the cause should be sought.
Stage 2
The initially reversible lymphedema can change into irreversible, chronic edema. The tissue changes fibrosclerotically (hardened and scarred connective tissue) and permanently. Furthermore, a new formation of fatty tissue begins in the affected body region. The edema is no longer soft and can be pushed away, but becomes hard and firm. Swelling due to elevation can no longer be observed.
The restriction of movement of the joints increases and the sensitivity of the skin decreases. The skin is also rough and cracked and can be painful.
Treatment can only relieve symptoms and not completely end lymphedema. There is always a high risk of relapse. The damage to the connective tissue is irreversible. In the absence of treatment and skin care, the lymphedema can reach the stage of Elephantiasis to reach. The Elephantiasis describes a clinical picture that is characterized by massive swelling of body parts as a result of lymphatic congestion.
Stage 3
The third stage of lymphedema is usually only reached if therapy is not initiated in the early stages. The third stage is therefore almost only found in developing countries, and there it is mainly a consequence of the parasite disease Elephantiasis (This disease is caused by massive swelling of parts of the body as a result of lymph congestion).
Several liters of lymphatic fluid collect in the tissue, making normal movement impossible and disfiguring the affected parts of the body. The skin also shows major changes. The skin on the affected part of the body is cracked and blisters, scars, fistulas and papillomatosis form. In extreme cases, the skin becomes dry and grayish and looks like elephant skin, which gives the stage its name. Furthermore, there are wound healing disorders. If left untreated, a lymphangiosarcoma, a malignant tumor, can develop.
As with many diseases, the prognosis of lymphedema depends heavily on the time of diagnosis and the start of therapy. In later stages, there is only an alleviation of long-term effects and pain.
The accompanying symptoms
The lymphedema itself is actually not a disease, but a symptom. This symptom occurs in many different conditions, and depending on the cause, the other symptoms will also vary. With all lymphedema, the restriction of movement is a serious side effect.
In the case of a congenital malformation, the lymphedema is often only accompanied by pain, skin changes and local wound healing disorders.
In the case of a tumor disease, the symptoms of the tumor disease itself are in the foreground. This includes the so-called B symptoms, which are made up of night sweats, fever and weight loss. Depending on the type of original tumor, those affected suffer from weakness, immune system disorders and pain
With the parasite disease Elephantiasis the lymphedema in the scrotum can lead to infertility. Before the actual lymphedema develops, those affected develop fever, allergic reactions and headaches. In extreme cases, bacterial superinfections and blood poisoning can occur. The tissue changes can also degenerate and cause malignant tumors.
Leg pain as an accompanying symptom
The legs are the most common part of the body affected by lymphedema. Many liters of lymph fluid can collect in the legs and cause severe pain due to the pressure on the tissue. The drainage disorder itself, such as a tumor, can also cause pain.
The pain can either cause pressure itself or blood vessels constrict, which then leads to pain in the affected leg because of the insufficient oxygen supply. Just like blood vessels, nerves can also be directly affected and stressed by the pressure. Furthermore, a large amount of lymph fluid also means a considerable weight that the body has to carry.
The areas of the body most damaged by extra weight are the knee joints. The knee joints wear out faster than in a healthy person and means additional pain, especially when moving.
In addition, by the third stage at the latest, the cracks and rashes of the skin are painful and dry. These skin changes are permanent. The pain in the legs does not have one cause, but is a combination of many reasons that do not have to occur in every person affected.
The localization of the edema
Lymphedema on the leg
Depending on the cause of the lymphedema, the legs are often the first region of the body that the person concerned notices. The reason for this is that the body has to work against gravity in the legs in order to transport the lymph and also the oxygen-poor blood back to the core of the body. Gravity is an additional obstacle to the actual cause of the lymphedema. This also explains the observation of many affected people that the leg edema in the first stage recedes as soon as the affected person put their legs up.
Especially in the legs, developmental causes such as the lack of venous valves or valves of the lymphatic vessels are a major risk factor, as these normally counteract gravity. Sufferers often experience severe leg pain and develop skin discomfort in the legs.
Lymphedema does not necessarily have to affect both legs, as the cause, such as an accident-related, broken lymph vessel, is one-sided. In the case of swollen legs, it must always be clarified whether it is actually lymphedema or another type of edema, since underfunction of the heart can also lead to edema without the lymph being involved.
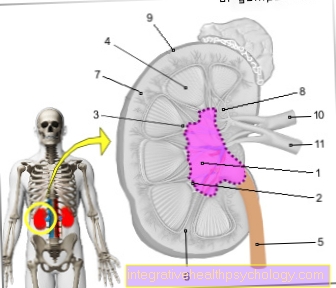
Find out more about the topic here: Lymphatic system.
Lymphedema on the foot
Lymphedema, which affects the legs, almost always begins at the foot and goes up to the drainage disorder. So if the outflow disorder of the lymph vessels is in the lower leg, the lymphedema affects only the foot permanently, while a drainage disorder in the groin means lymphedema in the whole leg.Due to the force of gravity, the lymph fluid always collects first in the subcutaneous fatty tissue of the foot.
One examination option for diagnosing lymphedema is therefore the mobility of the toes. This is limited at an early stage even with mild lymphedema. Affected people have difficulty walking and have trouble wearing normal shoes. In about half of those affected, both feet are edematous, as the cause is above the junction of the two drainage routes. In the first stage, the edema regresses when the person concerned puts their legs up.
The edema reappears after exercise. Tight clothing and particularly tight belts on the legs and feet can increase the formation of edema and should therefore be avoided in the case of known lymphedema. In the case of the feet and legs, if you step on both sides, you should always think about edema caused by the heart, as this usually begins in the legs.
Read more about the topic here: Water in your feet.
Lymphedema on the arm
In contrast to the legs, lymphedema on the arms almost always occurs on one side only. In the legs, the drainage pathways of the lymphatic vessels are linked in the trunk of the body, while the arms have their own drainage pathways. The arms are also low in most situations during the day and therefore the body has to move the lymph fluid against gravity.
Edema on one arm is very likely to be lymphedema, as heart-related edema is always first visible in the legs. In the arms, too, the edema initially subsides when the arm is raised. A common cause of arm lymphedema is surgery for breast cancer. In most cases, lymph nodes in the armpit area are also removed, which also represent stations for the lymphatic drainage of the arms. With this operation, lymphatic tracts could be permanently damaged and thus lymphedema could be triggered.
At the onset of the disease, lymphedema can be examined by measuring the circumference of the arm on both sides. As a preventive measure, breast cancer patients should not wear tight clothing after the operation, as this is an additional risk factor.
Find out all about the topic here: Lymphedema of the breast.
Breast lymphedema
Basically, lymphedema can occur anywhere in the body. After breast cancer surgery, in which lymph nodes are usually removed and / or irradiated, lymphedema can also occur in the breasts.
However, the occurrence of lymphedema in the chest is much less common than in the arms or legs. Often, slight lymphedema in the chest area is also not noticeable, as the breast size can also increase with weight gain and is not always the same on both sides.
Lymphedema of the face
Lymphedema on the face is very rare, but it does happen. The causes range from cancer to congenital drainage disorders.
In contrast to the legs, facial edema is more pronounced in the morning than in the evening. This is because during the day gravity helps with removal. The target of the lymph is venous blood vessels below the collarbone and thus below the face.
The biggest problem with facial lymphedema is social exclusion and the associated depression.
Also read the topic: Angioedema.
Lymphedema in the abdomen
Lymphedema can also develop in the abdominal area. However, since there are many different reasons for an increase in volume in the abdomen and also for pain in the abdomen, this is often not recognized as lymphedema. To be on the safe side, other causes of the increase in volume must be excluded.
Lymphedema is rather rare in the abdomen, as the lymph vessels there are large and the way to the vein angle, the destination of the lymph, is not far. In most cases, the legs are also affected, as the lymph backs up and the lymph vessels in the abdomen are fed by those in the leg.
Lymphedema in the genital area, scrotum
Just like the rest of the body, lymph can build up in the scrotum. Operations in the groin area can injure the lymph vessels and cause lymphedema.
Lymphedema in the testicle is also a typical symptom of the parasite-induced elephantiasiswhich, however, occurs more in tropical regions. The Elephantiasis describes a clinical picture that is characterized by massive swelling of body parts as a result of lymphatic congestion.
In Europe, tumor removal in the genital area or the groin is more likely to be a cause of lymphedema. In extreme cases, many liters of fluid can collect in the scrotum.
Also read the article: Water in the testicle.
The consequences of lymphedema
In the absence of treatment, lymphedema can have many long-term effects. The skin develops blisters and eczema, which gradually heal less and less. In the elephantiasis stage, the skin becomes leathery and gray. The pressure can also damage blood vessels and muscles.
The accumulation of the lymph can make the body many kilograms heavier and, in the long term, damage the joints. The tissue changes and in extreme cases can also produce malignant tumors.
The skin changes as a result
At the beginning, no damage can be seen on the skin. From the second stage onwards, blisters and rashes form, which in some cases can be inflamed.
Wound healing disorders later occur and even small injuries cause large eczema.
In the absence of treatment, the skin can reach the stage of Elephantiasis to reach. The Elephantiasis describes a clinical picture that is characterized by massive swelling of body parts as a result of lymphatic congestion. The skin can then no longer heal at this stage. If detected early, skin care should be performed regularly and wounds should be checked regularly.
More information on the topic Wound healing disorders you'll find here.
The treatment
Treatment depends on the location of the edema, the cause, and the stage. The primary therapy is decongestion. With manual lymph drainage, the lymph fluid is shifted into non-congested areas and can thus be transported further in a natural way. This is possible because small connections, so-called anastomoses, exist between the various lymph vessels and the entire pathway is not blocked.
The next step is to prevent re-accumulation by applying compression stockings or compression bandages to the affected limbs. Physiotherapy and exercise can help keep the joints flexible. The actual cause of the lymphedema cannot be treated. In later stages, the edema can often no longer be completely removed.
In addition to treating the edema itself, treatment and care of the skin is necessary. Anti-inflammatory ointments and moisturizers can be used for this. However, these should be fragrance-free, as the already damaged skin often does not tolerate this well. The exact therapy should be discussed with the attending physician and checked regularly by him.
Read more about the topic here: Lymphatic drainage.
The compression stockings
After the lymph has been removed by manual or mechanical lymphatic drainage, the goal is to continue to prevent the edema. Compression stockings, for example, are suitable for this because they reduce the accumulation of lymph.
Compression stockings are a medical product and should not be used without consulting a doctor. There are different thicknesses and lengths of the stockings and depending on the type of edema other stockings are useful. It is also necessary to change the stockings regularly as the strength can decrease.
More information on the subject Compression stockings you'll find here.
Which medications can help?
In most cases, drug therapy is only used to support the skin. There are various ointments for the skin that support healing and fight bacteria. A causal treatment is not possible.
So-called water tablets do not help with lymphedema and can even be harmful, as they increase the protein content in the tissue and worsen the lymphatic transport. These water tablets are useful for heart-related edema.
Homeopathy
Lymphedema is a serious disease that should always be clarified and treated by conventional medicine. Without adequate treatment, the lymphedema develops into the so-called Elephantiasis (a massive swelling of parts of the body due to a build-up of lymph).
Homeopaths recommend Lycopodium clavatum and Gingko Biloba. This can be taken supportively. Purely homeopathic therapy is not recommended.
Which exercises can help?
With some movement exercises and physiotherapy, the lymphatic drainage in the body can be supported. Exercise, swimming, and cycling are helpful sports.
Except for swimming, the prescribed compression stockings should be worn in these sports. When swimming, the even water pressure from the outside supports the lymphatic transport. When resting, the affected body regions should be elevated. A classic massage of the body areas is not recommended, as this stimulates the production of lymph. Certain movements can specifically support removal, but other exercises can also have a harmful effect, which is why the exercises should be learned as part of physiotherapy.
Basically, walking is better than standing and long sitting should also be avoided. Gymnastic exercises also promote blood circulation and muscle building. Healthy muscles can increase the transport of lymph and venous blood, which is why this is also called a muscle pump. Cross-country skiing or endurance running with overloading the legs should be avoided. However, this does not mean that these sports have to be eliminated entirely.
Find out more about the topic here: Physiotherapy.
Can surgery help?
Conservative therapy for lymphedema can be very stressful for those affected and usually has to be continued for life.
An alternative can be surgery. There are different approaches to re-enable lymph drainage. Two procedures aim to create new channels for the lymphatic fluid by transplanting lymph tissue from healthy areas of the body. The transplanted tissue forms fresh lymph vessels in the new location. This system is called the lympholymphatic anastomosis.
Another method that directs the lymph fluid directly into the veins is called a lympho-venous anastomosis.
Another possibility, which only works with lymph vessels that have been constricted by radiation and surgery, is to remove the disruptive scar tissue. The final surgical option is tissue removal. This is not a curative therapy, but only a relief, as there is less space for fluid in less tissue. This resection allows compression therapies to work better again. Surgery is always associated with risks and should therefore be the last option
Which doctor treats lymphedema?
Lymphedema is a disease that many different doctors are involved in treating. The first symptoms are often noticed by the family doctor of the person concerned. After oncological operations, the treating oncologists can also diagnose lymphedema in follow-up examinations.
The treatment is partly carried out in lymphology specialist clinics and by the family doctor. When surgery is added, a surgeon is called in. In the case of elephantiasis caused by parasites, a tropical medicine specialist may be necessary.
Lymphedema prophylaxis
So-called primary prophylaxis includes all measures that can be taken to directly prevent lymphedema. These include giving up nicotine and losing weight if you are very overweight. Regular exercise also promotes the transport of lymph fluid. After surgery in the groin, tight belts should not be worn and physiotherapy is also useful after breast cancer surgery.
Secondary prophylactic measures refer to measures to prevent a relapse and the formation of new edema after therapy. This includes wearing compression stockings or compression bandages. Certain gymnastics and swimming can also improve lymphatic transport. Tight clothing should be avoided.
Affected areas of the body should be protected from overheating and cold. The water temperature when showering or bathing should be lukewarm. Injuries and insect bites should also be prevented, as both increase the formation of lymph fluid. The skin care should not contain any perfumes, as any allergic reactions can also lead to an increase in lymph formation.
Can Lymphedema Be Cured?
The cause of lymphedema cannot be eliminated and therefore there is actually no cure. However, symptoms can almost completely disappear if diagnosed early and started treatment immediately. ´
The prophylactic measures, such as wearing compression stockings, often have to be maintained for life. In some cases, surgical measures can limit further treatments.
However, those affected should take certain precautionary measures. Long periods of standing and long car journeys should be avoided and certain sports can have a protective effect. From the second stage onwards, complete elimination of the edema is usually no longer possible. Especially in the third stage, the Elephantiasis (massive swelling of body parts as a result of lymphatic congestion) the severely damaged skin and the surrounding tissue can no longer be healed.
Difference to lipedema
At the beginning of the disease, lymphedema and lipedema are very similar. Both of them lead to an increase in volume in certain areas of the body. Lymphedema can occur all over the body, while lipedema occurs in almost all cases in the legs.
Lymphedema affects both men and women, but lipedema almost only women. In most cases, the men affected have hormonal disorders. While the cause of lymphedema is usually mechanical, lipedema is suspected to be hormonal. This assumption exists because lipedema usually occurs after hormonal changes such as menopause.
Lipedema is a pathological, structural change in the subcutaneous fatty tissue, which then tends to accumulate more fluid. In the first stage of lymphedema, the edema is soft and can be pushed away. The lipedema cannot be pushed away from the start. Lymphedema can occur asymmetrically on only one leg or arm, while lipedema is always symmetrical. A genetic predisposition is also observed in lipedema.
Find out all about the topic here: Lipedema.
Can I use the sauna with lymphedema?
Affected areas of the body should be protected from temperature fluctuations and especially from overheating, as this increases the formation of lymph fluid and hinders its removal. We therefore advise against going to the sauna. The resulting temperatures in a sauna would increase the lymphedema.












.jpg)













