Actions in the event of a stroke
introduction
A stroke is a life-threatening emergency that requires immediate medical treatment. This results in an interruption of the oxygen supply to the affected brain areas and nerve cells die. The longer this interruption exists, the larger areas of the brain are affected. The time until the necessary initiation of therapy thus plays a decisive role in the treatment of the stroke.

In addition to rapid transport to a specialized hospital by medical staff, the early detection of a stroke plays a crucial role. There are some memory aids that everyone should be able to use in order to act quickly.
Also read: stroke
The FAST test for stroke
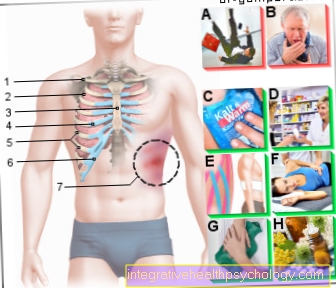
The "FAST test" offers laypeople the opportunity to assess whether or not they have had a stroke. "FAST" is an acronym and is composed of several terms.
- The "F" stands for "Face". Ask the person concerned to smile. If there is a stroke, one of the corners of the mouth hangs down, a sign of hemiplegia.
- The person is also asked to stretch their arms (“A”) forward and turn the palms of the hands up. If an arm sinks or the palm of the hand is turned downwards, this is another sign of a stroke.
- "S" stands for language in this test. It is important to pay attention to a basic inability to speak or a slurred language.
- The "T" stands for "Time" and is intended to underline the relevance of contacting the emergency service as quickly as possible.
Read more on this topic at: This is how a stroke is diagnosed
Emergency call in the event of a stroke
Sending the emergency call as quickly and correctly as possible is crucial for the prognosis of a stroke. There are a few things to keep in mind here.
In principle, the emergency number 112 applies to mobile phones and landlines throughout Europe. The suspicion of a stroke should be expressed so that an emergency doctor is sent through the emergency service.
Furthermore, the control center will ask some questions about the current situation, all of which must be answered. In any case, you should wait until the control center ends the call. Important questions in this context are the exact location and possible complications when getting there.
The more precise the information provided by the caller, the faster the emergency service will be on site.
What to do until the ambulance arrives in the event of a stroke?
In principle, one should make sure that the person concerned is never left alone, but that a person is always with them, calms them down and recognizes possible worsening of the situation. Since swallowing disorders can occur, no more food or drink should be given if a stroke is suspected and removable dentures should be removed.
Furthermore, the upper body should be positioned about 30 ° upwards, for example with a large pillow in the back.If vomiting or even loss of consciousness occurs, the person concerned should be brought into the stable side position to keep the airways free and to prevent swallowing.
You should always check your breathing and, if possible, your pulse. In the event of a failure to breathe or a loss of pulse, resuscitation measures should be carried out immediately until the emergency doctor is on site.
How should the person be positioned in the event of a stroke?
The correct positioning of a stroke patient depends on the acute level of consciousness. If the person is still awake and does not show any signs of nausea or vomiting, the upper body should be positioned slightly upwards (around 30 °), for example by a pillow or an armchair.
However, if there is a clouding of consciousness to the point of unconsciousness, the person should be transferred to the stable side position.
In this case, the person is turned on one shoulder and the leg on the upper side is bent and placed on the floor as a support. Furthermore, the hand on the upper side of the body should be pushed under the back of the head so that the head is tilted a little and any vomit flows out forward and cannot be swallowed. In addition, the head should be slightly overstretched to ensure that the airways are secure.
Resuscitation measures in the event of a stroke
Basically, resuscitation measures are always indicated when breathing and cardiac activity are no longer evident. These two criteria can be determined by checking your breathing or your pulse.
In the former, the person concerned is placed on their back and you can hear whether breathing is taking place a short distance from the mouth and nose. You should also pay attention to a slight breeze, which you can feel on your ear when you breathe sufficiently. In addition, attention should be paid to the movement of the chest.
The pulse is felt in the carotid artery. This is located about 2 finger widths below the lateral edge of the jaw. However, since the palpation of the pulse is very error-prone, it is now advisable to make the decision about the initiation of resuscitation measures largely dependent on the failure to breathe.
If this is the case, resuscitation according to the 30: 2 scheme should be started immediately. This suggests that after 30 compressions of the chest, you give 2 breaths.
Ventilation is provided mouth-to-mouth by holding the patient's nose closed and stretching the head. Then blow in enough air twice for one second so that the chest of the person concerned rises visibly.
The heart pressure massage works like this: in the lower third of the sternum, use both hands to press the chest in so hard 120 times per minute that it drops 6 cm and then let go. To keep the rhythm, e.g. the song "breathless" to be sung in the head.
Learn more at: First aid
What happens in the hospital after a stroke?
Once the patient arrives at the hospital, a series of examinations and therapies are initiated. This procedure is now highly standardized and some hospitals have set up special departments for dealing with strokes, so-called stroke units.
After a thorough neurological examination has taken place, imaging is sought immediately in order to show a possible stroke and to distinguish whether it is a pure vascular occlusion or whether there is a major bleeding, which can be identical. The method of choice here is computer tomography of the skull (cCT).
To do this, read the articles:
- CT-You should know that
- MRI for a stroke
If bleeding could be ruled out, a so-called thrombolysis is started immediately, i.e. the drug dissolution of the blood clot. However, such treatment is only effective for the first 4.5 hours after a stroke begins.
Alternatively or in addition, depending on the location of the blood clot, mechanical removal of the clot can also be attempted, a so-called mechanical thrombectomy. Here, the thrombus is destroyed and removed using a small wire that is inserted through the groin. This technique has become more and more established in recent years, but can only be carried out in the case of clots in larger brain vessels.
In the further course, the patient is closely monitored for some time in order to identify and treat possible complications early.
For more information on this topic, we recommend our page on: This is how a stroke is diagnosed
Also find out about. Stroke therapy
Prepare previous illnesses and medication list
When the emergency doctor arrives, it is always advisable to have a list of the medication taken and the patient's previous illnesses ready. On the one hand, these serve to estimate how high the risk of a stroke or bleeding is, but they are particularly important when planning therapy.
For example, certain blood clotting disorders are a clear contraindication to the administration of medication to dissolve a blood clot, as the risk of bleeding would be too high. In addition, information about possible pre-existing illnesses is used to facilitate the interpretation of the imaging and the risk assessment of complications.
Recommendations from the response
You might also be interested in these topics:
- This is how you recognize a stroke
- This is how a stroke is diagnosed
- These are the consequences of a stroke!
- Cure for a stroke
- Blood clots in the head
- Life expectancy in a stroke
- stroke















.jpg)