Thigh amputation
definition
An amputation is the complete or partial separation of a limb from the rest of the body.
The thigh amputation is a surgical procedure to separate the leg above the knee joint. The thigh amputation is also known as a major amputation.

Indications for a thigh amputation
The indication for an amputation always comes last in medicine and is only given if there are no other conservative or surgically tissue-conserving measures available.
In addition to the most serious accidents with non-reconstructible injuries to the leg and muscles, tumors and circulatory disorders are the most common indications for amputation of the leg.
In particular, circulatory disorders in the context of a sugar disease (diabetes mellitus) have increased significantly in the last few decades and are the most common indication for an amputation. In addition to diabetes, peripheral arterial occlusive disease can also result from smoking and is one of the vascular diseases caused by arteriosclerosis. Further indications for a thigh amputation are rapidly ascending infections, for example with gas burn or other malignant soft tissue germs, which cause severe blood poisoning with a greatly increased risk of death by further ascending into the body's circulation.
You may also be interested in this topic: Causes that lead to an amputation
Causes of the femoral amputation
The most common causes of a thigh amputation include blood vessel diseases, which lead to a blockage of the blood vessels due to circulatory disorders.
These include peripheral arterial occlusive disease, also abbreviated to PAD, and vascular diseases as a result of the diabetes mellitus. Such a vascular occlusion hinders adequate blood flow to the leg, which as a result can die.
Another cause is the infection and colonization of the leg with bacteria. In order to prevent the bacteria from reaching the rest of the body via the bloodstream and the lymphatic system and endangering life, an amputation must be performed in some cases.
This also applies to tumors. To prevent the tumor cells from spreading in the body, in some cases they have to be completely removed by removing the leg.
In addition, injuries or congenital malformations can cause a thigh amputation.
Further information on this topic can be found at: Causes of an amputation
What amputation techniques are there?
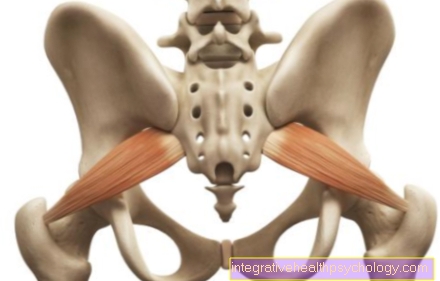
In the case of a thigh amputation, the bone can be removed along the entire length of the thigh, whereby the bone is always severed as far as possible towards the knee in order to obtain a long stump for simple prosthesis fitting. Thanks to new surgical techniques, good prosthetic restorations are now also possible for shorter stumps.
A distinction is made between the so-called transcondylar thigh amputation, in which the amputation is carried out close to the knee with as much of the interior space as possible, the cancellous bone, as a support surface, from the thigh amputation according to Gritti, in which the bone is also separated as close to the knee as possible, which then bones with the end of the stump the kneecap is covered.
Also read the article on the topic: Amputation technique
How long does a thigh amputation take?
The operation of a thigh amputation itself only takes a few hours. The subsequent hospital and rehabilitation treatment, however, requires significantly more time. Especially in the case of major operations such as a thigh amputation, the subsequent hospital stay can last up to 4 weeks, followed by rehabilitation treatment between 3 and 10 weeks.
OP preparation
A thigh amputation requires careful and extensive preparation. As soon as the indication for amputation has been made and other therapy alternatives have been ruled out, the doctor is obliged to have a detailed informative discussion in which he explains the exact procedure in the operation, the subsequent rehabilitation treatment and possible risks and complications.
If the patient agrees in writing to follow the treatment, first a series of examinations to assess the general condition, resilience and the associated risk of complications. These include blood count analyzes, examinations of the heart and lung function, and a vascular status. Imaging by means of computed tomography is also usually carried out in order to obtain a precise understanding of the anatomical conditions.
In addition to the preparations for the operation, measures should be taken in advance for the time after the operation, for example in the form of physiotherapy to specifically strengthen the muscles and the purchase of possible aids. Another important point is the emotional preparation for the upcoming ampuation, here psychotherapeutic discussions can be of great help.
OP process
A thigh amputation is a long and complicated operation, but it can be carried out safely thanks to standardized surgical steps.
Unless there are medical reasons to the contrary, the operation is always performed under general anesthesia.
For example, various serious heart or lung diseases speak against general anesthesia.
Read more on the topic: General anesthetic.
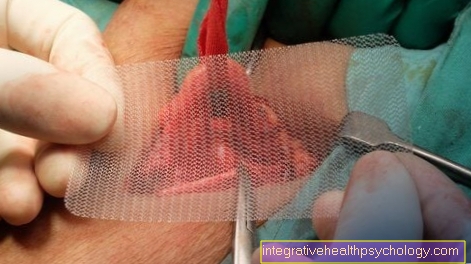
Immediately before the operation, the leg to be amputated is thoroughly disinfected and the rest of the patient is covered with sterile cloths in order to keep the risk of bacterial infection as low as possible.
The patient lies on his back during the entire operation. Usually the amputation is carried out in a "bloodless" state. This means that a large cuff is placed around the leg and inflated. This compresses and closes the blood vessels.
In this way, the intraoperative blood loss can be significantly reduced and the surgeon has a better view of the operating area.
An incision is made first through the skin, then through the soft tissues, muscles, tendons and fat until the bone is exposed.
This is cut through with a bone saw and then rounded at the edges so that no sharp edges can damage the surrounding tissue later.
Lidocaine is injected into the ends of the nerve fibers that have been cut. Lidocaine is a local anesthetic that locally numbs the nerve. This is to prevent the occurrence of phantom pain.
After the bone has been severed, the soft tissue behind the bone must be removed. The cut does not go straight through the leg, but at a slight angle. This creates a kind of flap made of skin and subcutaneous fatty tissue, which can be folded over the bone stump and has a cushioning function.
A drain is then inserted to drain any blood that may seep into the wound after the operation.
Finally the wound is sewn up. First the deep structures are sutured and finally the skin. Clasps or threads can be used to close the skin.
Further information on this topic can be found at: Amputation technique
Risks of a thigh amputation
Every operation involves risks and complications, but we always strive to keep these as low as possible.
The most common complications include impaired or delayed wound healing, bleeding, nerve damage that can lead to phantom pain, infections, or poor stump care.
In addition, there are general operational risks, such as intolerance to the anesthesia, pain and the risk of vascular occlusions as a result of the long period of hospitalization. Many of the complications ultimately make it much more difficult to adjust a prosthesis, which means that the patient can only slowly regain his independence.
Aftercare
Follow-up treatment begins immediately after the operation. Wound healing is the first priority after the operation.
A healthy, properly healing wound is dry, not reddened or swollen and the wound edges are close together.
The stump can be raised slightly to aid blood flow back to the heart.
It should be wrapped with bandages, making sure to use a corn-ear-shaped wrap to promote blood and lymph flow.
The sutures or staples are usually removed after 14 to 21 days. Most of the time, patients lie in bed after surgery to allow the body to recover from the efforts of the surgery.
To prevent thrombosis and embolism as a result of the lack of exercise, heparin injections or other blood-thinning drugs such as aspirin are prescribed.
Of course, appropriate pain therapy is also carried out. Pain medication can be given directly into the veins as tablets or as a drip.
Pain catheters (epidural anesthesia) are also a good alternative. These are introduced by anesthetists into the space surrounding the spinal cord and thus inhibit the conduction and perception of pain at a central level.
Care of the amputation stump
Proper care of the amputation stump is crucial for its later functionality.
The residual limb must later be able to transfer the weight and movements of the body to the prosthesis. To do this, the skin must slowly get used to more pressure and strain, just like the muscles.
In the first time after the operation, edema should be prevented from forming. The wound healing is to be supported and infections and muscle spasms prevented.
For this purpose, lymph massages are carried out, which are intended to stimulate the lymph flow and support the immune system.
The shape of the stump is also decisive. Bandages are used that are wrapped in the shape of an ear of corn. Bandages must never be wrapped in a circle. This would inhibit blood flow and lead to edema.
In addition to bandages, so-called liners, which are usually made of silicone, or stockings are also used. They fulfill the same function as the bandages.
In addition, the skin is relieved and cared for with massages and creams.
Physiotherapy helps strengthen muscles and learn new movement patterns.
In summary, the care of the amputation stump is very important and must not stop even after the wound has healed. Caring for the residual limb is time-consuming, especially in the immediate aftermath of the amputation, but it leads to good results if carried out correctly.
The subsequent adjustment of a prosthesis then takes weeks to months, as transition and learning prostheses must first be made in order to ensure the relearning of the ability to stand and, in particular, to walk.
Do you need rehab after the operation?
Rehabilitation treatment is necessary after each thigh amputation so that the patients learn to deal with their new life situation.In addition to helping with wound care for the fresh surgical wound, prosthesis adjustment and walking training are essential components of the rehabilitation stay.
The aim of rehabilitation treatment is to enable patients with their new disabilities to live independently in their dimensions. Psychological support for coping with the loss of a body part also takes place here.
What does the prosthesis look like?
Preparation for a prosthesis treatment begins in the hospital. If the wound healing of the scar is timely and without irritation, an initial appointment with an orthopedic technician can be arranged after consulting the doctor. The first step is to make a plaster cast of the stump from which the first prosthesis socket will be created. This corresponds to the individual stump shape and includes the remaining leg. There are many different techniques from which the most suitable one is selected after a detailed discussion.
The first prosthesis that a patient then receives is a provisional, so-called interim prosthesis, as the residual limb can change significantly in the first time after the amputation, for example by increasing and decreasing the residual limb volume. Once the wound has finally healed and the residual limb does not change any more, a final definitive model is made. Various parts are adapted to this definitive socket in order to create the individually optimal prosthesis. There are also many possibilities and variations that can be tried out and optimized in cooperation with the orthopedic technician.
More on this: Prosthesis supply
What level of care do you get after a thigh amputation?
Although a thigh amputation is a major turning point in the life and everyday life of every person affected, it does not automatically receive a fixed level of care. The application for this must be made and depends on the individual case.
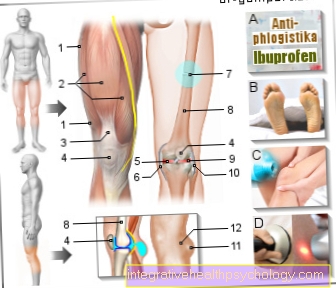
Concomitant symptoms prior to amputation
Accompanying symptoms before the amputation depend on the underlying disease.
If the cause is a vascular occlusion, pain often occurs. In addition, the leg can feel cold and stiff because it is no longer supplied with enough blood.
Patients with diabetes mellitus, on the other hand, usually do not feel any pain, since they have suffered nerve damage due to diabetes, which prevents the transmission of pain signals.
Infections show up based on the classic signs of inflammation pain, redness, overheating, swelling and loss of function.
Tumors have very different symptoms. They can be painful, but they don't have to be. Sometimes they are noticeable due to restricted mobility. Often these are incidental findings that do not cause any symptoms and are discovered by chance during an examination.
Diagnostics before the thigh amputation
The basic rule is to remove as much as necessary but as little as possible. In order to be able to determine the exact amputation level, it must be determined before the operation at which part of the body the cause of the amputation lies and whether other regions of the body are also affected. This is e.g. this is the case when tumor cells are carried away to the rest of the body via the blood from the thigh.
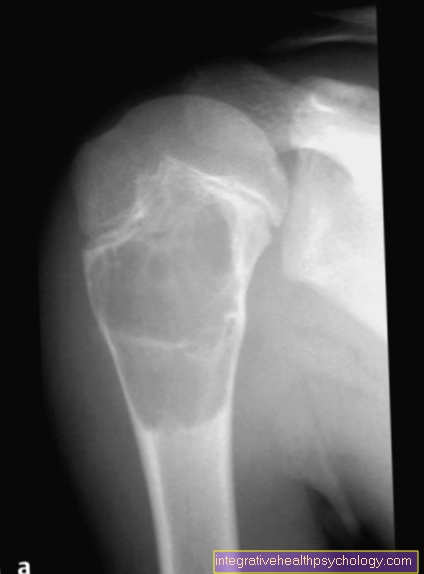
Is there e.g. If there is a vascular occlusion, imaging methods, i.e. CT or MRT, must be used to determine exactly where the vessel is occluded in order to then be able to decide where the leg has to be cut off. By default, a CT or MRI image is made to assess the vessels, bones and muscles.
Further diagnosis depends on the underlying disease.
You may also be interested in the following topics:
- Amputation heights
- Lower leg amputation
Further information
- Causes that lead to an amputation
- Symptoms before an amputation
- Amputation heights
- Prosthesis supply
- Lower leg amputation











.jpg)