Polyneuropathy
Synonyms
Neuropathies, polyneuritides
definition
A Polyneuropathy is a widespread disease of several peripheral annoywhich, for example, for the sense of touch (sensitive) and muscle movement (motorized) are responsible, with many different causes (e.g. toxic, infectious, metabolic (metabolic), genetic factors). The disease almost always begins at the lower extremity, is usually symmetrical and has slowly progressing symptoms. Often with polyneuropathy there is one Nerve inflammation.

Epidemiology
The worldwide spread of polyneuropathy is increasing 40 per 100,000 Population estimated, but there are regional differences. These differences are based on ever new causes of damage, especially environmental toxins such as insecticides, toxic drugs and drugs, while the traditional harmful substances (Noxious substances) how Thallium and arsenic (e.g. at as murder or suicide means) are rare today. An example can be cited here are the accumulated polyneuropathies in Morocco as a result of poisoning caused by mixing edible oil and gun lubricant. Polyneuropathy as a result of a diphtheria has become increasingly rare, but the frequency of polyneuropathy with involvement of the meninges (Meningopolyneuritis) as a result of a tick bite (Lyme disease) increased. In Europe are by far the most common causes Diabetes mellitus and Alcohol sickness, in contrast, in tropical and subtropical regions malnutrition (Malnutrition) and leprosy. Diabetic polyneuropathy occurs ten times more often than other polyneuropathies with a proportion of 30-40%. Alcohol polyneuropathy affects men more often and usually occurs between the ages of 50 and 60, whereas diabetic polyneuropathy affects more women and usually manifests itself between the ages of 70 and 80. Both diseases can also occur in adolescents. The hereditary (hereditary) Polyneuropathy manifests itself in early to middle age.
causes
There are many different causes of the Polyneuropathy. The most common are listed below:
- Genetic causese.g. hereditary (hereditary) Polyneuropathy
- Metabolic disorders, e.g. in diabetes mellitus
- Malnutrition or malnutrition
- Vitamin B12 uptake disorder and other admission disorders (Absorption disorders) of Intestines
- Disorders of the protein balance (Dysproteinemia) in blood
- Infections, e.g. after a Tick bite (Lyme disease)
- Disorders of the vessel walls (arteriopathy)
- Toxic disorders, e.g. in triaryl phosphate poisoning
- Tumor diseasese.g. in each third of the cases of Lung cancer or tumors of the lymph tissue
Symptoms

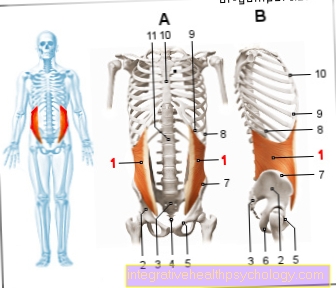
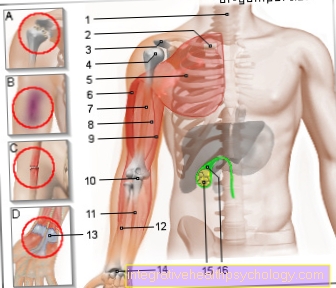
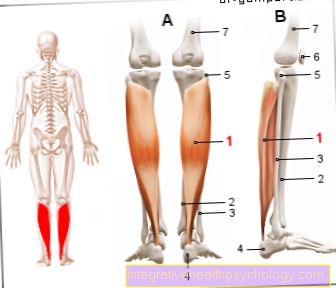
At the beginning of a polyneuropathy, both legs are usually affected symmetrically, but especially the lower legs. Occasionally, one-sided complaints in the area of the thighs and the pelvic girdle can also be observed. Those affected rarely describe symptoms of the face or trunk. A distinction is made between symptoms that affect the sensitive nerve tracts and complaints in the motor system.
Symptoms of polyneuropathy typically begin at rest or at night. Patients report all kinds of abnormal sensations, which can culminate in painful sensations over time.
Possible abnormal sensations can be:
- tingle
- Burn (Also read: Burning in the fingers)
- "Ant running"
- Sting
- "Feeling of being electrified"
- Swelling
- Sensation of heat / cold
- Feeling of pressure
- "The feeling of being on cotton wool"
- Numbness
- Increased sensitivity to pain, so that even light touches hurt
In addition to the sensory disorders, the motor nerves can also be affected and cause symptoms:
- Muscle spasms, especially at night
- Muscle wasting (muscle atrophy)
- Muscle aches
- Muscle weakness
- Muscle twitching
- Unsteady gait, especially in the dark
Read more on the topic: Symptoms of polyneuropathy
course
Just as different as the symptoms can be Course of a polyneuropathy be. Usually the disease begins with Parasitic sensations on both feet or lower legs. Those affected report e.g. typically about Burning soles of both feet at night or Tingling in both calves.
Depending on the cause, it can start creeping (e.g. diabetes polyneuropathy) or suddenly (e.g. due to infection). In the course of the disease, symptoms increase and even numbness. Surprisingly, if there are simultaneous abnormal sensations, it is very common significantly reduced pain sensation observe. As a result, e.g. Broken pieces, splinters or ingrown toenails not noticed. If those affected do not perform careful and regular foot care, inflamed, poorly healing wounds can quickly develop.
Furthermore, many polyneuropathy patients also show disorders of the motor nervous system during the course of the disease. It lets itself in unsafe Watch gang, frequent tripping and "Getting caught ”with your feet. Special forms of polyneuropathy (Guillain-Barré syndrome) can also begin with motor failure.
species
Polyneuropathies for infectious diseases:
5% of polyneuropathies occur in infectious diseases and are assigned to polyneuritides. The "inflammatory" polyneuropathies are caused by three mechanisms:
- Direct exposure to the pathogen
- Damage from its poison
- Damage from the immune system response
Viral polyneuritides are caused by Herpes zosterFlu (influenza), measles, AIDS i.a. caused. However, these are very rare. On the other hand, bacterial forms are more common, especially borreliosis, diphtheria, botulism and leprosy.
- Lyme disease: Asymmetrical sensory disorders, paralysis, involvement of the meninges and cranial nerves
- diphtheria: Paralysis of the soft palate and the pharynx muscles with nasal pronunciation and swallowing disorders due to the paralysis of the responsible cranial nerves, later also paralysis of the Respiratory muscles and sensory and motor paralysis of all four extremities
- botulism: Difficulty swallowing and abdominal discomfort after consuming canned food, then paralysis of the eye muscles, but no sensitivity disorders
- leprosy: Tuberculoid leprosy causes asymmetrical sensory disorders and paralysis, lepromatous leprosy causes cranial nerve symptoms. Dimorphic leprosy is a hybrid form.
Toxic polyneuropathies
Usually found with this type of Polyneuropathy a symmetrical distribution pattern with sensory and motor failures. Addictive substances and environmental toxins such as industrial and pesticides are among the most common causes.
- Alcoholic polyneuropathy: very common form. In addition to the effects of the alcohol itself (Ethanol) and its degradation product (acetaldehyde) malnutrition plays an important role in alcoholics. Defects in the enzymes that are responsible for breaking down alcohol can also be involved in the cause of the disease. Symptoms include severe leg pain, often muscle cramps and calf pressure pain. The sense of touch and vibration is reduced, the muscle reflexes are weakened, the ASR is absent. The motor nerve conduction speed is usually normal or only slightly reduced. The critical limit value for alcoholic polyneuropathy is considered 80-100g Alcohol daily.
- Vitamin deficiency polyneuropathy: Eye muscle paralysis and fluctuations in attention (Vigilance) mostly suggest a vitamin B1 deficiency in chronic alcoholism. A vitamin B2 deficiency leads to pellagra polyneuropathy with an inflammatory reaction of the skin (dermatitis), Diarrhea (Diarrhea) and dementia. The vitamin B6 deficiency also leads to polyneuropathy.
- Polyneuropathy from Triaryl Phosphate Poisoning: Example of Acute Toxic Neuropathy. Triaryl phosphate is contained in mineral oil offshoots and, if mistakenly used as an edible oil, leads to diarrhea and fever. After 10 to 38 days there is paralysis of the feet, later paralysis of all four extremities; the sensitivity is also disturbed. In some cases the failures of the annoy not or not completely back.
Asymmetrical: There are three different types:
- In the case of mononeuropathy, only disorders in the supply area of a peripheral nerve can be recognized.
- In mononeuropathy (Mononeuritis) multiplex (Multiplex type) disturbances can be seen in the supply areas of several peripheral nerves, but the neighboring nerves are hardly or not at all impaired.
- The main neuropathy is a combination of mononeuropathia multiplex and a symmetrical polyneuropathy.
Diabetic polyneuropathy

In addition to alcoholic polyneuropathy, diabetic polyneuropathy is the most common polyneuropathy. 20-40% of diabetics show signs of polyneuropathy, most of them are between 60 and 70 years old and have been ill for more than 5 to 10 years.In 10% of these patients, the investigation of the polyneuropathy led to the diagnosis of diabetes in the first place. The causes are both the direct effects of the metabolic disorder and the changes in the blood vessels caused by diabetes (diabetic angiopathy) to a polyneuropathy. With this form mainly axon degeneration occurs, but sometimes also demyelination of the nerve fibers (see diagnosis).
The symptoms are initially symmetrical, sensitive irritation symptoms with sensory disturbances and often burning and painful areas on the feet. Typical are the lack of the Achilles tendon reflex and a reduction in the sense of touch, especially the sense of vibration. Later on, around 50% of patients experience failures in their movement function (motor skills). Asymmetrical disorders or failure of individual nerves (Multiplex mononeuropathy), especially the eye muscle nerves, further cranial nerves or the femoral nerve, a nerve in the area of the thigh muscles, occur. In addition, in about half of the cases there are disorders of the organs (vegetative disorders): dry, red skin, bladder disorder, an accelerated pulse (Tachycardia), Difficulty swallowing, diarrhea and impotence in male diabetics. There is also a risk of a painless heart attack.
The focus of therapy is the optimal setting of the diabetes.
Read about this too
- Diabetic neuropathy
- Burning feet
Polyneuropathies due to alcohol
In addition to type 2 diabetes mellitus ("diabetes"), that counts Abuse of alcohol to the most common causes a polyneuropathy. Experts estimate that 15-40% of all alcoholics suffer from polyneuropathy. alcohol thus damages the nerve cells and is therefore "neurotoxic“.
In the case of chronic or long-term abuse, those affected mostly develop symmetrical abnormal sensations in both legs (especially in the lower legs). Patients complain about tingle, Burn and Pain in the calves or feet. Often there are also motor failures, so that patients over Impairment of walking or frequent stumbling to report. Usually these failures are still included muscular dystrophy ahead.
Occasionally, the small hand muscles may be affected first. In the case of an alcohol-related polyneuropathy The patients also sweat more on the palms and feet. The skin becomes progressively thinner and even can painful ulcers develop. Since the sensation is reduced, those affected often develop chronic wounds.
Fortunately, with strict abstinence from alcohol, one can observe a slow but almost complete decrease in symptoms.
Nephrogenic and hepatic polyneuropathy
Dialysis patients with severe kidney disease in particular complain of nocturnal calf cramps and burning pains in their feet ("burning feet"). The paralysis pattern is symmetrical. Polyneuropathy can also occur in patients with chronic liver failure.
Read more on this topic at: Burning feet
Hereditary (hereditary) polyneuropathy
In connection with hereditary diseases such as the Porphyria polyneuropathies can occur. Porphyria is an inherited disorder in the synthesis of heme, a complex with iron in red blood cells. This leads to tachycardia, one increased blood pressure (hypertension) and strong, labor-like stomach pain (Colic). Neurologically, there is either a motor mononeuropathy multiplex or a symmetrical paralysis of all four extremities.
According to international classification, a distinction is made between hereditary motor-sensitive and hereditary-sensitive neuropathies.
Hereditary motor-sensitive neuropathies (HMSN I-IV):
The HMSN type I. is the hypertrophic ("enlarged“) Form of Muscle wasting (Muscular atrophy), also called Charcot-Marie-Tooth disease, which is usually inherited as a dominant trait. It is the most common of the hereditary neuropathies and manifests itself between the ages of 10 and 30 years. A symmetrical, sensitive and motor polyneuropathy with calf atrophy is characteristic ("Stork legs“), Arches foot- and hammer toe formation and a prematurely reduced motor and sensory nerve conduction speed due to a thickening of the nerve cords.
The HMSN type II is the neural form of muscle atrophy. In her, the nerve conduction velocity is normal compared to type I and the distribution pattern can also be asymmetrical.
The HMSN type III is inherited recessively. Typical are the even more thickened nerve cords and thus the even more reduced nerve conduction velocity than in type I.
The HMSN type IV, Refsum-Kahlke syndrome, is a symmetrical one Polyneuropathythat spreads from the extremities to the trunk of the body. It is based on a recessive inherited disorder of the metabolism of a particular person fatty acid (Phytanic acid). Symptoms include Disorders of the Movement coordination (Ataxia), Night blindness (Hemeralopia), damage to the retina (Retinal degeneration) and deafness. With this type, too, the nerve conduction velocity is considerably delayed.
The HMSN types V, VI, and VII are rare forms that are most symptomatic eye are combined.
Hereditary sensitive neuropathies (HSN I-IV):
Due to the lack of perception of pain (analgesia) it comes to Broken bones, Injuries or mutilations.
Polyneuropathies due to damage to blood vessels
In diseases of the blood vessels, with inflammation of the blood vessel wall a so-called Vasculitis can result in damage to the annoy caused by insufficient blood circulation or nutrition. This leads to sensory and motor paralysis, which are distributed either symmetrically or according to the multiplex type. In addition, it can lead to disturbances in the nutritional or metabolic state of the body.
diagnosis
To diagnose a Polyneuropathy The treating family doctor or neurologist will first ask you to ask detailed anamnesis. To do this, he asks questions about the nature of the complaints, their timing and course. He is also interested in previous illnesses (such as Diabetes mellitus), family history or medication use.
Then a physical examination quickly provide further information. The doctor tests for this sensitivity, Temperature-, Pain-, such as Vibration sensation.
Various devices such as a small tuning fork, are used here. In addition, the Reflexes examined in the affected area; these are typically weakened in polyneuropathy. These exams are for patients completely painless.
If the suspicion of polyneuropathy is confirmed, further examinations must be arranged to confirm the diagnosis. E.g. the Nerve conduction velocity (NLG) can be measured to determine the stage of the disease. Laboratory tests, Nerve water puncture, Biopsies and further neurological examinations are then initiated.
Read more on the topic: Diagnosis of a polyneuropahtia
therapy
For pain and sensory disturbances, thioctic acid is given, the effect of which has been proven especially in diabetic polyneuropathy. Acetylsalicylic acid, e.g. aspirin, and Paracetamol questionable, if the pain is persistent, must be Carbamazepine, Pregabalin, both actually drugs against epilepsy, and antidepressants (Thymoleptics) as well as so-called "nerve suppressants" (Neuroleptics) can be used. Of course, the underlying disease requires special treatment measures. Physical exercise and occupational therapy are also important training. If the cause is a known harmful agent, the ingestion should of course be avoided, as for example with excessive alcohol consumption.
Prognosis / rehabilitation
Polyneuropathies are usually slowly progressive and usually regress gradually. However, residual symptoms, especially a loss of reflexes, can still be detected after years. The prognosis also depends on the cause, e.g. the symptoms and the subsidence of symptoms (Remission) in alcoholic polyneuropathy depending on the dose of alcohol. Polyneuropathies associated with diseases such as leprosy progress with their underlying disease, but can be influenced therapeutically. With well adjusted Diabetes mellitus and well-treated diphtheria, symptoms gradually resolve (Remission), with acute porphyria, however, relapses often occur (Relapse).
Polyneuropathy - curable?
Numerous factors and underlying diseases can influence the development of the complex clinical picture “polyneuropathy”. So it is not surprising that general statements about the question of curability are hardly possible are. However, depending on the underlying disease, it may well be possible that the disease is curable.
Basically: The longer the polyneuropathy or its accompanying illness exists, the less likely it will be a cure.
E.g. the diabetic polyneuropathy incurable, since irreversible damage to the sensitive nerve fibers has existed for a long time.
At a alcohol-related polyneuropathy however, they are Chances of a cure are much better. Because as soon as the neurotoxin alcohol is removed from the circulation in the long term, the damaging effect subsides.
Furthermore, some forms of polyneuropathy are also due to infection, such as. the Lyme disease after a tick bite. As soon as the pathogen is fought with antibiotics, the polyneuropathy subsides and is therefore curable. Also through Vitamin deficiency states (e.g. Vitamin B12) the complaints can be triggered. When the vitamin is given, the symptoms disappear.



















.jpg)