schizophrenia
Synonyms in a broader sense
- Split consciousness
- endogenous psychoses
- schizophrenic psychoses
- Psychoses from the schizophrenic circle of forms
definition
To understand the term schizophrenia, one must first clarify the term psychosis. A psychosis is a condition in which the patient loses touch with reality (reality). Normally we humans perceive our reality with the help of our senses and then process it in our thinking. In the context of a psychosis or a psychotic state, both can be disturbed.

Schizophrenia is a form of psychosis in which, on the one hand, sensory perception can be disturbed and hallucinations can occur, and on the other hand, the thinking itself can also be severely disturbed. The processing of perceptions can e.g. lead to delusions.
All in all, people in a psychotic state gradually lose touch with reality and thus with their life. They find it increasingly difficult to fulfill the tasks assigned to them (as partners, employees, drivers, etc.).
What psychosis or schizophrenia does not mean is a split personality or multiple personality disorder!
Read more on the subject at: Personality Disorder or What is Schizophrenic Psychosis?
Symptoms
Overall, the clinical picture or the symptoms can vary greatly from patient to patient. Although this is a multi-faceted disease, the clinical symptoms are divided into 3 classes:
- Positive symptoms
- Negative symptoms
- Psychomotor symptoms
Particularly specific for schizophrenia are, for example, disorders of the own sense of self in the sense of external control, in which those affected have the feeling that their thoughts are not their own, as if ideas were given or taken from them. A delusional experience is also part of the schizophrenia, for example in the form of paranoia or megalomania. Acoustic hallucinations in the form of commenting, mostly negative voices, possibly accompanied by other hallucinations, are also very typical. In addition, thinking and logical combinations are usually restricted and the environment and experiences can no longer be interpreted correctly.
The affect, i.e. their emotional experience, is also impaired, which explains the apparent apathy. In some contexts, however, inappropriate overreacting and incomprehensible reactions are also possible. The severity of these symptoms varies depending on the form of schizophrenia. Multiple personalities, as they are often staged in films and television, are a rather rare occurrence in schizophrenia.
Some of the symptoms described above are very specific to schizophrenia, while some symptoms are more accompanying. For this reason, these are divided into symptoms of 1st and 2nd rank.
Read more about this: Symptoms of schizophrenia
Symptoms of the 1st rank
The term “symptom of the first order” is understood to mean symptoms that can give a clear indication of the possible presence of schizophrenia, as they are very specific for schizophrenia.
One of the most common symptoms of the first order is the hearing of voices. A distinction is made between voices in dialogue and commentary, as well as sounding thoughts, i.e. the feeling that one's own thoughts are being repeated by another person. The latter often causes those affected to feel that they are being dictated to the thoughts of others.
In addition, there may be bodily influencing experiences, which describes that those affected have the feeling that someone else has access to their body and, for example, raise their arm, although they do not want to. Many people compare these experiences with the feeling of being a puppet.
Further symptoms of the first rank are thought impulses, thought spreading, thought deprivation. With the latter, those affected feel that mostly a supernatural being like the devil would put their thoughts to them and that they could no longer have clear thoughts.
This spectrum of symptoms also includes the feeling of being influenced by the will and the delusional perception, i.e. that real perceptions are given a delusional meaning.
2nd tier symptoms
Symptoms of the second tier are not very specific to the presence of schizophrenia, as opposed to symptoms of the first tier. It is important to understand that this division of rank does not make any statement about the severity or effects of the individual symptoms, but rather describes the specificity of these symptoms for schizophrenia.
Hallucinations, which can also occur with other mental illnesses, are an example of such a symptom. A distinction is made here between acoustic, optical and olfactory hallucinations. Affective disorders can also be part of the spectrum of symptoms in schizophrenia. These disorders include, for example, depressive moods, exaggerated euphoria, perplexity or so-called parathymia, i.e. a difference between the expression and what is felt. An example of the latter would be when a person is laughing when actually feeling very sad.
In addition, those affected may have delusional ideas or beliefs.
These delusional ideas are usually linked to the other symptoms of schizophrenia. For example, people with visual hallucinations often imagine, in the sense of a delusion, that they are being persecuted or punished by a higher power.
Read more on the subject at: Symptoms of schizophrenia
Positive symptoms
The symptoms of many mental illnesses are divided into positive and negative symptoms. The term positive symptoms here includes all symptoms that are added compared to the normal state
In schizophrenia, this includes acoustic and visual hallucinations, such as hearing voices. In combination with the mostly existing delusional ideas or imaginations, these can lead to a complete distortion of reality for those affected and drastically reduce the quality of life.
Further symptoms that can be assigned to the positive symptoms are formal and substantive thought disorders. The former are usually described by schizophrenic patients as a blockade of thoughts or as the robbery of thoughts by a higher power, which means that they can no longer pursue logical trains of thought. In contrast, content-related thought disorders go hand in hand with delusional ideas or ego disorders.
Thus, normal circumstances are often related to the person himself and an attempt is made to find an explanation for this, which is usually not understandable for outsiders.
Other positive symptoms are:
- Behavior changes
- Disturbances in emotional expression
- associative loosening (disorientation)
- Perseverations (repetitions)
- Neologisms (word creations)
Positive symptoms are responsible for the typical picture of schizophrenia and are particularly pronounced in acute attacks. They respond well to the common antipsychotic drugs and are much easier to treat than negative symptoms.
Negative symptoms
In contrast to positive symptoms, the term negative symptoms includes all symptoms that are associated with the loss of normal physical and mental abilities, such as mental deficits or speech impoverishment.
Affective disorders are also included in this spectrum of symptoms. These usually go hand in hand with a reduction in drive and a lack of interest, which can then lead to social withdrawal.
In the area of mental performance, there can often be severe limitations, which increase as the disease progresses. In addition, there is a strong reduction in the ability to concentrate and speech impoverishment.
If schizophrenia already occurs in children and boys, restrictions in motor skills, in the sense of muscle weakness and coordination problems, can also be described.
Unfortunately, medication hardly has any effect on these complaints, so treating negative symptoms is extremely difficult.
The delusions
In the so-called delusion, the content of thinking (ideas, beliefs) is disturbed. As part of the delusion, patients develop ideas that they believe (in the sense of “knowing”) are true, even though they are not true. They stand up for their ideas and ideas with tremendous commitment and usually do not allow any contradiction. Occasionally, but by no means always, these ideas appear quite logical and well thought-out even to outsiders, so that one can speak of a downright “delusional system”. There are some “typical” delusions in schizophrenia.
- Paranoid delusion
With this type of delusion, patients feel persecuted, threatened, or even suppressed.
For example: Cars passing by can suddenly belong to the secret service. The neighbor who does not say hello is planning a bugging attack. The ringing postman suddenly becomes a hit man, and on the street you feel constantly being watched or followed. - Megalomania:
The content of this madness is the greatness of the patient.
For example: The patient considers himself the savior of the world, the most brilliant scientist, direct descendant of Napoleon or Jesus, or some other overly capable person. - Control madness:
This leads to the idea that one's own actions, thoughts or impulses are influenced and controlled by other “powers” or people.
For example: A patient who experiences his thoughts as strange and changed can be firmly convinced that his neighbor across the street is “irradiating” him with a device. Also physical complaints such as restlessness or stomach pain werden explained by “actions” of other people. - Relationship mania:
In the delusional relationship, the patient sees certain actions, situations, objects or people as being important to him.
For example: The patient believes that television or radio broadcasts convey texts for them personally. Traffic signs can also have a hidden message indicating the direction in which the patient should move. - Poverty madness
Here the patient knows about his impending financial ruin, although realistically there is no danger. Here, the concerns in particular often revolve around the care of relatives - Hypochondriac delusion:
Here the patient knows that he is suffering from at least one serious physical illness. This disease is often perceived as incurable and fatal by the patient. Negative results and assurances from several doctors cannot dissuade him from this conviction. - Sin delusion:
The sick person knows that he has sinned against a higher or lower power. If the person is a believer, the content of the madness is often religious. If there is no particular spirituality, sin can extend to worldly concerns. - Nihilistic delusion:
This is a delusion that outsiders find particularly disturbing. As a result of his perceived emptiness, the patient denies existence as a person and possibly also the existence of the world around him.
Disturbances in thinking and speaking
In many schizophrenia patients, a noticeable expression is noticeable, which is mostly due to a change in formal thinking. Formal does not mean what you think in terms of content, but how one thinks.
For a better explanation, the most common formal changes in thinking are listed below.
For the sake of completeness, it should be mentioned that such formal thought disorders naturally also occur with other disorders, such as mania, dementia etc. can occur.
- Associative loosening (disorientation):
This means that patients come from "Höcksken auf Stöcksken". Even small external stimuli cause a patient to lose track. All in all, the whole flow of language seems incoherent and difficult or impossible to understand.
For example: A patient is asked whether he has already received his medication today. He replies: No, I don't want them ... they always have such stupid side effects. My brother-in-law is stupid too. He's been with my sister for 2 years now. The 2 comes before the 3 ... in front of the house is better than behind the house etc. - Perseverations (repetitions):
With this type of thinking disorder, individual words or sentences or parts of sentences are repeated over and over again. But it also means rigidly holding onto a train of thought or a lack of flexibility in thinking. - Neologisms (word creations):
Patients “invent” new words and incorporate them as a matter of course in their flow of speech. - Disturbances in emotional expression
This type of disorder is an abnormality that many schizophrenics have. They often have great difficulty in behaving emotionally appropriately to the situation. Sad news, for example, is laughed at, a beautiful situation can lead to desperate weeping. Overall, the overall mood can be relatively unpredictable. There can be outbursts of joy in a relatively short period of time, followed by outbursts of anger.
Hallucinations
Hallucinations are loosely translated as "misperceptions of the senses". Our 5 senses convey stimuli to us with which we deal with the environment. In the context of schizophrenia, it can happen that one or more of these senses receive and transmit non-existent stimuli.
The most common is the "heard" hallucination (acoustic hallucination). Here the patients hear either so-called directed or non-directed hallucinations. Undirected hallucinations are e.g. Popping or engine noises.
Directed hallucinations are more common and usually come in the form of voices. As a practitioner, you have to be very careful about what these voices say to the patient. On the one hand, it is possible that there will be a conversation between the patient and the hallucination (dialogizing voices), on the other hand, that the voices do not agree but speak about the patient (commenting voices).
A third option is particularly problematic. These are the commanding voices (imperative voices). Often times, patients have a very strong urge to give in to these commands in hopes of finding peace. An imperative hallucination is therefore always a reason for inpatient treatment, as there is an increased risk of self-harm. (If necessary also against the patient's will. See also the topic of care law).
The second most common hallucination is the "seen" hallucination (optical hallucination). All kinds of things (animals, people, objects) can appear here. A typical and well-known example of an optical hallucination are the so-called "white mice" during an alcohol withdrawal delirium.
Less common are the taste (gustatory) Hallucinations the content of which is mostly about food and drink; the smelled (olfactory) hallucinations, in which bad smells (e.g. smoke and rotten smell) are in the foreground or the felt (tactile) hallucinations, in which "insect crawling", electric shocks or itching are described.
In schizophrenic patients, an increased perception can often be observed even before the onset of real hallucinations. Colors are perceived as brighter, sounds as louder.
Read more on the subject at: Hallucinations
The psychomotor system
The term psychomotor describes the parts of a movement sequence that can be modulated by psychological processes.
In the context of mental illnesses such as schizophrenia, this connection between psyche and movement can be disrupted, which can result in different symptoms.
This includes the training of movement automatisms, which can present themselves in many different forms. For example, people can develop the automatism that they always have to repeat everything they hear immediately or always perform a movement opposite to that of the observed people.
Another symptom is the development of tics, involuntary muscle twitching that repeats itself quickly. There can also be a strong, pronounced motor restlessness, such as constantly running back and forth in a room.
In contrast to the symptoms mentioned, which are associated with increased movement, psychomotor disorders can also be associated with a severe lack of movement and lack of drive.
Find out more about the topic here Ticks.
Nervousness as a symptom
The nervousness that occurs in most schizophrenic patients is added to the negative symptoms and is often one of the first signs of the manifestation of schizophrenia.
The emergence of this pronounced nervousness can on the one hand be attributed to a fundamental disorder that can exist in the context of these diseases. However, other possible symptoms of schizophrenia, such as hallucinations, can lead to nervousness because those affected do not know how to deal with this situation. Furthermore, motor restlessness can be observed in many patients as part of a psychomotor disorder, which can intensify the picture of nervousness.
Pronounced restlessness is also very common in schizophrenic patients. This restlessness arises on the one hand from a disturbance of the psychomotor system, which can be associated with the development of tics, automatic movement or the urge to move constantly.
But psychological aspects also play a major role in the development of restlessness. For example, schizophrenic patients can often no longer have clear thoughts and, as the disease progresses, usually develop delusional ideas that can be intensified by visual and acoustic hallucinations.
All of these factors mean that those affected can never rest both physically and mentally.
Depressive moods as a symptom
In about half of all cases, the beginning of schizophrenia is associated with a depressed mood or a depressed mood.
This is mainly based on a general mental and spiritual slowdown that can go hand in hand with the development of joylessness. Some patients report feeling empty inside. The result is often the cooling of social contacts with friends or family, which can lead to complete social isolation.
These symptoms can at first easily be confused with the presence of depression, which is one of the reasons that schizophrenia can rarely be diagnosed at such an early stage.
Thoughtfulness beyond the normal level can also be observed.This is attributed to the formal thought disorders described above and means that the thoughts revolve over and over again around the same, unpleasant topic without a solution being found.
In addition, many patients look for a possible explanation for the occurrence of the hallucinations, which then often ends in delusions.
Find out more about the topic here Depressions.
Poor concentration as a symptom
The development of a lack of concentration is a very early symptom of the onset of schizophrenia and is present in almost all patients.
On the one hand, this is due to the general disturbance of well-being that is present in many schizophrenic patients. But the so-called loss of thoughts, which many sufferers complain about, can also be the cause. They then describe that they could no longer have clear thoughts because someone else, usually a higher power, robs them of their thoughts.
In addition, the often existing acoustic and visual hallucinations can lead to a constant overload of stimuli and distraction, which then lead to severe poor concentration.
Read more about this topic here: Poor concentration.
Sleep disorders as a symptom
Most schizophrenia patients suffer from severe sleep disorders as the disease progresses, which is the result of the many possible symptoms.
The often existing mental and motor overactivity can mean that those affected cannot come to rest. In the common form of paranoid schizophrenia, many patients also suffer from delusions that go hand in hand with paranoia and lead to sleep disorders.
Furthermore, the possible acoustic hallucinations are a possible reason for the development of sleep disorders
Sleep disorders are usually treated with sleeping pills, even with schizophrenia.
Read more on the subject here Sleep disorders.
Neglect of personal appearance
The neglect of personal appearance represents, in addition to other symptoms, such as a depressive mood or memory disorders, another early symptom of the onset of schizophrenia and occurs in approx. 20-40% of those affected.
This symptom is classified as a general disturbance of wellbeing and is associated with a loss of hygiene.
This is due to the fact that many schizophrenic patients are withdrawn and personal appearance plays an increasingly minor role for them. This symptom is usually exacerbated by increasing social isolation.
Lies as a symptom
It is very common in schizophrenic patients that outsiders feel they are being lied to when the person concerned describes their delusions or speaks about hallucinations they have seen or heard.
Mostly one forgets how real a person suffering from schizophrenia feels like such hallucinations or voice perceptions. Affected people can usually not tell whether something is really real or just part of a hallucination
These impressions are reinforced by the development of delusions and an overriding reason is sought for the perceptions, which then quickly appear like a lie to outsiders.
In contrast, schizophrenic patients may actually lie in order to conceal the actual presence or extent of the illness from relatives. This phenomenon is usually more pronounced at the beginning of the disease.
Irritability as a syndrome
One of the early signs of the onset of schizophrenia can be mood disorders such as increased irritability.
This is especially the case with the most common form of the disease, paranoid schizophrenia, which focuses on developing delusions and acoustic hallucinations.
Affected people quickly get the impression that they are being lied to by all other people and that they do not want to believe them, which can then express itself as strong irritability
Symptoms around the eyes
Many schizophrenic patients have problems continuously following a slowly moving object with their eyes and fail due to quick and jerky gaze sequences. It has not yet been clearly established whether this can be attributed purely to psychological stress or specifically to schizophrenia. Studies are currently underway on this topic in order to be able to detect schizophrenia in the eyes at an early stage, but eye examinations are not yet part of today's diagnostics.

What can residual symptoms be?
The designation of the residual symptoms includes all symptoms that still exist after a successful therapy or the healing of an illness.
In schizophrenia, this is usually the case after an acute attack. In general, it can be stated that the negative symptoms are significantly more dominant than the positive symptoms.
In many patients, after an acute episode of schizophrenia, a change in personality can be recognized to varying degrees, which is often associated with a depressive mood and social withdrawal. In addition, the memory and concentration disorders can also be permanent in some patients.
Only in a small proportion of the patients are no residual symptoms detectable after an acute attack has subsided.
Read more on this topic at: What is a schizophrenic residual?
Symptoms in Children
Schizophrenia is a comparatively rare disease in children and boys. Unfortunately, the prognosis of the disease depends largely on the age of the first illness and is therefore worse in children than in adults.
The first symptoms of schizophrenia in children are often very unspecific, such as thought disorders, and are often trivialized and attributed to the developmental process. As a result, most childhood schizophrenias are only correctly diagnosed at a later age.
Other early symptoms of schizophrenia can include disorders of physical, mental and social development. It can be established that language acquisition usually only occurs a few months to years later than with other children, and that moderate to severe coordination problems and muscle weakness are present. In addition, there are affective fluctuations, such as pronounced irritability, bizarre behavior or the feeling of listlessness. There is also often a lack of social interest.
In addition to these early symptoms, the entire spectrum of symptoms of schizophrenia, such as hallucinations, delusions, hearing voices, etc., can develop in the course of the disease.
Read more about this: Schizophrenia in children
Is There a Safe Test for Schizophrenia?
There is no really safe test for any disease in psychiatric medicine. Schizophrenia in particular is not a uniform disease, because each patient has a very individual expression and shows different symptoms. Objectifying psychological abnormalities by means of a test is therefore difficult and, with diseases as complex as schizophrenia, simply impossible. Instead, the diagnosis is made by recording typical symptoms and ruling out other causes. Therefore, a thorough physical and neurological exam and at least one brain imaging must be completed before tests to detect schizophrenia can be performed. Substance abuse as a cause of the symptoms must also be ruled out. The tests then carried out do not directly record schizophrenia, but rather typical thought disorders, as can occur with this disease. There is therefore no real schizophrenia test or questionnaire, as is the case with depression, for example, but only general tests of cognitive performance and psychological well-being.
Read more on the subject at: How can you test for schizophrenia?
What should you think of online tests?
Since, as already mentioned, there is no reliable schizophrenia test, the disease cannot be adequately recorded using online tests. Most schizophrenic patients do not believe they are sick anyway and would therefore not take such a test on their own. Nevertheless, such online offers can be helpful in recognizing worrying symptoms in yourself or a family member, classifying them correctly and having them clarified by a doctor. Online tests cannot therefore provide a reliable diagnosis, but they can lead the person affected or their relatives in the right direction and thus guide them to professional help.
What treatments are there?
Treating schizophrenia is difficult because there is no causal therapy. The main approaches are therefore drugs, more precisely antipsychotics (formerly known as neuroleptics), and psychotherapy or behavioral therapy to alleviate the symptoms. Unfortunately, very few patients realize that they are sick and are therefore difficult to motivate to long-term therapy. You can only reach the patient if he has problems in everyday life due to his symptoms, i.e. if he also benefits subjectively from a therapy, and if he trusts the practitioner.
The best success is achieved through medication. These mainly affect the so-called plus symptoms, such as Delusions and hallucinations. Negative symptoms, such as Loss of drive and apathy are unfortunately hardly influenced by the medication. The side effects are also a major problem with antiposychotics, above all the disorders of the movement sequence, such as Twitching or involuntary movements that may persist even after you stop taking medication. Therefore one tries today to fall back on less effective drugs, since they have significantly fewer side effects, and to supplement the treatment with psychotherapy.
Read more on the subject at: Therapy for schizophrenia
Which medications can help?
Highly potent, i.e. very effective drugs are, for example, the typical antipsychotics such as ben- or haloperidol. These work very well and very quickly, but have the big problem of motor side effects such as involuntary twitching and grimacing, so that they should only be given for a short time today. The new atypical drugs clozapine and risperidone have a slightly different effect and therefore have side effects that are easier to control, but are nevertheless very effective and are now the first choice in the treatment of schizophrenia.
Less potent substances are, for example, quetiapine or pipamperon, which have a calming rather than antipsychotic effect and, due to their better side effect profile, are preferred for milder disease courses. Although there are hardly any serious, uncontrollable side effects nowadays, side effects are also frequent with the newer drugs. All patients must therefore be examined and monitored closely.
Can schizophrenia be cured?
Doctors have no causal treatment methods available; the drugs and psychotherapies are only used to control symptoms and to prevent relapse. It is assumed that about one third of all patients recover completely after the first attack and are thus cured, one third will suffer at least one relapse and the last third will develop chronic schizophrenia. Early therapy has a positive effect on the prognosis, as the psychosis cannot develop completely and the risk of residuals decreases, but a cure is only supported, not directly achieved.
With antipsychotics, the risk of relapse can be reduced from over 80% to less than 20% and treated patients are usually relapse-free if treatment was started early enough. But whether this relapse-free was achieved through the drugs, which only keep the symptoms in check, or whether the patients are actually cured, can only be said in the long term. Favorable prognostic factors are female gender, good social integration, short and acute onset of schizophrenia attacks, and early therapy. Negative factors, on the other hand, are the male gender, a bad psychosocial situation and a gradual onset of the disease with pronounced negative symptoms and delayed treatment.
Read more on the topic: Can schizophrenia be cured?
course
Schizophrenia is very individual. The so-called "1/3" rule is known with regard to the course, which states that in a third of the patients the symptoms occur once and then not again. A second third has recurring "attacks" and a third remains in a so-called "residual state", in which there are no longer any acute positive symptoms (see below), but a general and permanent decline in performance.
The disease often runs in the 3 phases mentioned below, which can have very different lengths. But it can also be chronic without this phase.
There are three different phases of the disease.
- The prodromal stage:
In this phase there are no classic symptoms (see below) of schizophrenia. Rather, the general performance initially decreases. The person concerned has more and more difficulties in concentrating on his work or other tasks in everyday life. They often lose interest in their fellow human beings and their work, but also in their appearance and personal hygiene. Often there is a marked social withdrawal, an increase in anxiety and sleep disorders. Occasionally, delusions may already sound like (see below) or an increasingly confused thinking is noticeable. - The active (blossoming) stage:
In this phase, which is the actual phase of the disease, the symptoms listed below appear. These symptoms must occur almost continuously for a month or more for a diagnosis of schizophrenia to be awarded. In some cases this phase is triggered by psychosocial stress. - The residual phase
This third phase is reminiscent of the symptoms of the phase of the prodromal stage. As a rule, acute symptoms no longer occur, but the patient is not yet the "old man" again. There is often a kind of exhaustion with an increased need for sleep and depression (post-psychotic depression). This phase can only last for a short time, with the result that the patient almost regains his old performance and can lead a life as before.
But it can also be that he continues to suffer from “residual symptoms” and remains in the residual phase. Unfortunately, this patient is less likely to have the symptoms completely resolved. It is often observed that after years of residual symptoms, another florid phase follows, which then merges again into the residual.
It is difficult to predict which patient will "recover" to some extent (full remission) after an initial psychotic attack and who will continue to be severely impaired in life.
Research has shown that the likelihood of a favorable outcome is higher if the person led a successful life before the illness (high level of premorbid role fulfillment), if the disorder was preceded by a stressful event, if it started abruptly without a long prodromal phase or if she appeared in middle age.
What can be signs of impending schizophrenia?
Most psychiatric illnesses begin with a so-called prodromal phase, in which the first abnormalities appear in the patient, but no typical symptoms are yet pronounced. This stage can begin years before the actual psychosis. The first signs are usually not delusions or other typical characteristics of schizophrenia, but rather negative symptoms such as depression and social withdrawal. The patients are restless, troubled by worries and their ability to think and concentrate is impaired, their perception is consumed more and more and they lose touch with reality. They often feel an approaching threat, which can later turn into a madness as part of the psychosis.
Unfortunately, the first signs are very unspecific and could just as well be an expression of other problems and diseases, such as depression. In many cases, the relatives report in retrospect that the patient had become strange years before the psychosis and had continued to withdraw. More specific signs are only expressed months to weeks before the onset of psychosis, when a delusion emerges or hallucinations occur.
Learn more about this topic at: The signs of impending schizophrenia.
Frequency and duration of schizophrenic flare-ups
The frequency and duration of an acute schizophrenic flare-up vary widely. If the episode begins extremely acute and is the first of its kind, it can be treated well with medication and disappears completely after a few weeks. Then the chances are good that there will be no further symptoms. Patients with more frequent flare-ups that tend to start slowly, often require months of treatment and are at high risk of having another flare-up. The worst prognosis is for patients with pronounced negative symptoms, as these often persist even with medication.
Duration of a schizophrenic phase
The duration of a schizophrenic phase depends to a large extent on the patient, his previous illness and the therapy. If medication is taken and it is the first attack, the symptoms can usually be controlled in a few weeks and relapses avoided. If the patient has been suffering from schizophrenia for a long time and may not take any or only irregular medication, the full picture of the psychosis can persist for months to years. In some patients, the acute episode even turns into chronic schizophrenia, which does not resolve completely and some symptoms persist.
Causes of Schizophrenia
It is still not exactly clear why a person becomes schizophrenic. It is known that genes must have a major influence on the development of the disease, as many patients have relatives with the same diagnosis. Studies have shown that the risk of developing the disease increases 5 to 15 times if a first-degree relative has schizophrenia. It is therefore believed that genetic factors play the most important role. Among other things, the causative genes regulate the metabolism of various messenger substances in the brain, especially dopamine, which is why an imbalance of these signal substances is responsible for many symptoms of schizophrenia and antipsychotic drugs that affect the dopamine receptors are used. Irrespective of this, however, damage to the brain or impaired brain development has also been shown to be a contributory factor in many patients. However, since not everyone with such risk factors becomes schizophrenic, it is suspected that other circumstances, e.g. the environment, must play a role. If there is a certain genetic and biological disposition, factors such as stress or drug abuse could trigger the symptoms.
Find out more about the topic here: Causes of Schizophrenia.
What problems do schizophrenics have in relationships?
The effects of schizophrenia on the patient's relationship are very complex and highly dependent on how severe the psychosis is. In the best case, the partner can be brought into the therapy, the patient is optimally adjusted with medication or even cured and the couple is more closely connected afterwards than before. In the worst case, however, the patient withdraws further and further, experiences a complete change of personality and becomes increasingly alienated from his partner or involves him in the disease and thus becomes an enormous burden. Regardless of the exact course, it is always important to take care of the partner, who usually suffers from the illness of his loved one.
How high is the heritability of schizophrenia?
Genetic stress appears to be the greatest risk factor for developing schizophrenia. If you have no schizophrenic relatives, the risk of illness is less than 1%. If second-degree relatives are affected, the risk increases to 3-5%, and for first-degree relatives even to 9-12%. If both parents or the identical twin are affected, there is a risk of 50%. It is therefore assumed that over 80% of all schizophrenia diseases are more or less genetic. However, these genes only make the person susceptible to schizophrenia and without adverse environmental factors, even people with a high genetic risk usually do not get sick.
Read more about the topic here: Inheritance of schizophrenia.
Which forms of schizophrenia can be distinguished?
The three main forms are paranoid, hebephrenic and catatonic schizophrenia. The paranoid form is mainly characterized by delusions and associated symptoms. In Hebephrenic schizophrenia, however, the focus is not on delusions and hallucinations, but on a reduction in affect. This can be seen in the patient's apathetic, silly behavior. Catatonic schizophrenia manifests itself in the complete isolation of the patient who does not speak and does not move. This form is the most difficult to deal with.
What is paranoid schizophrenia?
Paranoid schizophrenia is the most common form of schizophrenia. The main symptom here is paranoia, i.e. a delusion, usually accompanied by acoustic hallucinations, e.g. in the form of voices in the head. These voices are mostly commenting and derogatory, so they judge the patient and his actions and thus wear him down more and more. Paranoia is popularly known as paranoid, but the word roughly translated only means “against the mind” and in the medical sense describes any form of delusions, which is why paranoid schizophrenia does not always have to be paranoid. Many patients also develop delusions of grandeur or a combination of different delusions. In most cases the delusion consists in the misinterpretation of other people, the patient perceives the behavior of his fellow human beings as hostile, as if everyone were against him and wanted something bad for him, so there is indeed a kind of paranoia. This initially shows up as anxiety and a general distrust, but can also develop into complex conspiracy theories.
Please also read our main article on this: What is paranoid schizophrenia?
What is schizophrenia simplex?
As mentioned earlier, there are many different forms of schizophrenia. It is therefore not clear whether it is really always the same disease, or whether schizophrenia is not just an umbrella term for many different psychoses, which have to be examined and differentiated more closely. Schizophrenia simplex is one of these forms, which in most cases only shows so-called negative symptoms and is therefore very different from the typical forms of schizophrenia. This means that the patients are mainly affected by reduced emotions, i.e. appear apathetic and listless, but only rarely suffer from delusions or hallucinations. They are therefore mainly noticeable for their inadequate behavior, the patients seem somehow strange and withdrawn. Unfortunately, the severity of the symptoms increases over time and is very difficult to treat, as the common drugs mainly affect the positive symptoms. The prognosis for schizophrenia simplex is therefore still unfavorable even today.
What is a schizophrenic residual?
Like most psychiatric illnesses, schizophrenia is more or less relapsing. This means that the symptoms will eventually go away on their own even without therapy, but they can also come back. Many patients are symptom-free and practically cured after a single attack, but unfortunately not all of them achieve complete remission, i.e. complete resolution of all symptoms. If certain abnormalities remain after a severe schizophrenic phase, this is referred to as a schizophrenic residual. In most cases the positive symptoms run like e.g. Delusions and hallucinations relapsing, so disappears completely, while negative symptoms such as e.g. Apathy and indifference can persist as residuals even between attacks. Unfortunately, these can worsen with each attack and can hardly be treated. Residues are therefore a major problem in chronic courses of schizophrenia.
You can find more information about the schizophrenic residual here: What is a schizophrenic residual?
Lies in schizophrenic patients
Schizophrenic patients are mentally ill, but not stupid. They know that their beliefs are met with rejection and at some point they start telling people what they want to hear. With such lies they cover up their symptoms on the one hand, and on the other hand they try to avoid potential persecutors and hostile people. Psychiatrists therefore try very hard to respond to the patient without judgment and to build up a relationship of trust so as not to be lied to.
Is life expectancy reduced with schizophrenia?
Schizophrenia is not primarily a physical illness, but it has an enormous effect on mental health and thus also on physical health, e.g. on the heart and vessels. If left untreated, schizophrenia is downright grueling. The risk behavior that patients show in their delusion, e.g. risky driving if they feel followed. Suicide is also a problem with schizophrenic patients when they can no longer see any other way out. Schizophrenia does not primarily make you physically ill, but life expectancy is reduced by several years to decades, especially in the long-term form, due to the psychological stress and accidents or suicides.
Why are schizophrenics more artistically gifted?
Many schizophrenic patients turn to the arts in order to be able to express their emotions. Art therapy is a popular approach to all mental illness because it has been shown to help patients, and profound schizophrenia with hallucinations understandably provides the person with a huge amount of inspiration. What comes out of this is therefore usually not only due to a potential talent, but above all an expression of the patient's emotional life. Art is therefore mostly just a mirror of schizophrenia, a highly complex and fascinating disease.
Schizophrenia and alcohol - are they compatible?
Many substances have a certain psychogenic potential and can therefore trigger or intensify psychoses. This is especially true of drugs, but alcohol can also make symptoms worse due to its intoxicating effects. As a neurotoxin, alcohol and other drugs can also damage the brain, which also has a negative effect on schizophrenia. In addition, most antipsychotic drugs do not get along with alcohol. There are therefore many reasons for schizophrenic patients to stay away from alcohol.
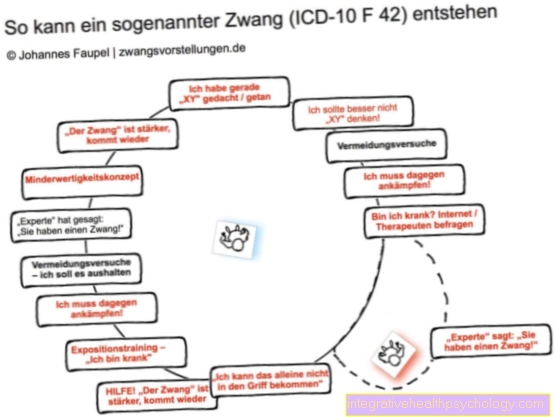
Psychosis and Schizophrenia - What's the Difference?
The doctor divides psychiatric illnesses into several categories, for example into neuroses (e.g. obsessive-compulsive disorder) and psychoses (e.g. schizophrenia). These terms have a rather unspecific meaning in the vernacular and are often used synonymously or in the wrong context. Schizophrenia is therefore a clinical picture, psychosis is just its umbrella term, so schizophrenia is one of many psychoses. The classification and nomenclature of psychiatric illnesses is very complex and many of the medically neutral terms are popularly burdened with prejudice, so that patients often feel labeled as "crazy" with their diagnosis. In addition, the names that are known to the general population are often too imprecise. Many doctors therefore use the term schizophrenic psychosis rather than the term schizophrenia and further categorize the clinical picture based on its subtype in order to describe the individual appearance as precisely as possible and not to discriminate against the patient.
Also read the article: What is the difference between schizophrenia and psychosis?
Schizophrenia and Depression - What is the Link?
As already described, if left untreated, schizophrenia leads to massive psychological and physical wear and tear in the long term. In many cases, the resulting symptoms meet all the criteria for depression. However, the schizophrenic symptoms are often difficult to differentiate from those of depression; the negative symptoms in particular are similar in both diseases. It is therefore suspected that there is a high number of unreported cases of depression among schizophrenic patients; exact figures on the frequency vary depending on the study. It is often diagnosed as postschizophrenic depression following an acute flare-up, which can last longer than ordinary depression and is associated with a high risk of suicide. Differentiating between schizophrenia and depression is important because the therapy is different and the patient should be helped as soon as possible. If treatment is given early, the prognosis for postschizophrenic depression is good and most patients recover from it, albeit after many months or a few years.
Read more on the subject at: depression
Schizophrenia and Autism - what is the relationship?
Until 1980 autism was regarded as a subtype of schizophrenia, a kind of childhood variant of the disease. Today we know that there are separate clinical pictures that differ not only in the age of the patient. However, both diseases are very variable and some forms are very similar. In addition, there are patients who show characteristics of both diseases. It has not yet been clarified whether two diagnoses are to be made in such cases or whether there are mixed forms of autism and schizophrenia.
Read more on the subject at: autism













.jpg)