Posterior cruciate ligament tear
Synonyms
posterior cruciate ligament tear, HKL, HKL rupture, cruciate ligament lesion, posterior knee instability, posterior knee instability, posterior cruciate ligament insufficiency, chronic insufficiency of the posterior cruciate ligament, cruciate ligament repair
English: posterior cruciate ligament rupture
definition
A posterior cruciate ligament tear arises due to exceeding the maximum expansion possibility of the posterior cruciate ligament, usually by external force.
This is a complete rupture, a so-called continuity interruption, of the posterior cruciate ligament, whereby sagittal instability (= occurring parallel to the central axis) and the so-called drawer phenomenon (= great displaceability of the lower leg against the thigh) become noticeable.

Cause of cruciate ligament tears
Of a posterior cruciate ligament tear in most cases not only the posterior cruciate ligament is affected. The injuries are usually much more complex and usually affect the entire knee joint in a way that is extremely impairing.
Accidents are common for posterior cruciate ligament ruptures, and not uncommon Car accidents responsible. This is due to the fact that sitting in the car causes the lower leg to be bent. If you press against it forcibly, the posterior cruciate ligament tears.
Symptoms
A tear of the posterior cruciate ligament is usually associated with typical symptoms that are characteristic of the injury.
Immediately after the trauma, which is responsible for the rupture of the posterior cruciate ligament, there is usually a swelling of the knee as well as a significant one Pain in the knee joint. Furthermore, instability of the affected knee joint is noticeable, which consists particularly in the flexion of the knee joint.
Depending on the extent of the injury and the affected soft tissue structures, bruises and open wounds can occur. Often there are accompanying injuries to other ligaments, bones or cartilage, which is why the resulting pain can only be localized diffusely.
During the physical examination, the so-called drawer phenomenon is noticeable because the knee joint lacks an important fixation due to the tear.
A positive drawer and Lachmann test are typical signs of a posterior cruciate ligament tear.

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
diagnosis

In general, examinations on a knee joint are fresh Ligament injury difficult due to the severe pain. The pain occurs at the moment of the injury, subsides, but usually returns with exertion.
A comparison with the “healthy” side should always be made. The rupture can cause severe swelling and effusions. As part of the examination, the degree of possible mobility, as well as the Meniscus mark to be clarified. As already mentioned, one can use the so-called Laughman Test to check medial and lateral ligament stability. The one also described Drawer test cannot be triggered in the event of an acute injury due to the muscular counter-tension.
In the case of acute swelling of the knee joint and one indicated as a result Knee joint examination can also provide information on whether or not there is a ligament injury in the knee joint. If blood is punctured from the knee joint during a puncture, this usually indicates a ligament injury of the knee joint
Not always will Cruciate ligament tears diagnosed in acute cases. The diagnosis is often only made when the instability of the knee joint is noticed. This can then be due to wear Changes in cartilage and the meniscus form.
The diagnosis is primarily based on the stability test in the extended and flexed position, with external and internal rotation and with the foot in a normal position. A close look at the knee with regard to swelling, effusion and the gait pattern should of course not be missing.
The neighboring joints should always be examined for clarification and blood flow, motor skills and sensitivity should be taken into account. In the case of acute injuries, the stability tests are generally difficult to carry out due to the muscle tension, so that further technical measures must be taken to establish the diagnosis. These are for example:
- X-ray diagnostics: X-ray images in various variations provide information about possible bony lesions.
- Magnetic resonance imaging (MRI): For final clarification whether and to what extent a cruciate ligament rupture is present. With the help of magnetic resonance imaging (MRT), the damage that has occurred can be precisely estimated and any necessary operations can be precisely planned and initiated.
You can also read our topic: MRI for a cruciate ligament tear Also one Puncture can shed light on a Cruciate ligament tear give. As soon as blood is punctured during such an operation, a ligament injury in the knee joint can be assumed.
Here again all the examination methods to diagnose a posterior cruciate ligament injury
Clinical diagnostics (examination)
- Assessment of knee swelling, Joint effusion, Range of motion and pain in motion
- Assessment of the gait pattern, leg axes
- Assessment of the femoral patellar joint (plain bearing of the kneecap)
- Assessment of knee stability and menisci
- Muscle atrophy (thinning of the muscle relief)
- Assessment of neighboring joints
- Assessment of blood circulation, motor skills and sensitivity (feeling on the skin)
Apparative diagnostics (examination with devices)
Necessary technical investigations
X-ray: knee joint in 2 planes, patella (kneecap) tangential
Special investigation useful in individual cases
- X-ray: knee joint p.a. when standing in 45 degrees flexion
- Friksche recording (tunnel recording)
- Recorded recordings
- Full-leg shots under load
- Functional recordings and special projections
- Sonography (meniscus, Baker's cyst)
- Computed tomography (V.a. Tibial head fracture)
- Magnetic resonance imaging (Cruciate ligaments, menisci, bone injury)
- Puncture with synovial analysis (for effusion)
- Automated drawer inspection (no standard inspection)
Please also read our topic: MRI for a cruciate ligament tear
MRI for a posterior cruciate ligament tear
- Thigh bone (femur)
- Kneecap (patella)
- posterior cruciate ligament (red)
- Shinbone (tibia)
Read everything about MRI for a cruciate ligament rupture under our topic: MRI for a cruciate ligament rupture
Anatomy cruciate ligament
The Knee joint represents the largest joint in the human body. The knee joint includes the femur, tibia, patella, meniscus, various capsular tissues, the ligamentous apparatus and many bursa.
If you take a closer look at the ligamentous apparatus, you have to distinguish, among other things, between the collateral ligaments, the internal ligaments and the cruciate ligaments. The cruciate ligaments run from the middle of the head of the tibia to the thigh bone and cross each other. The task of Cruciate ligaments consists of stabilizing the knee by preventing the lower leg from sliding forward over the thigh or the upper leg over the lower leg, depending on whether it is the anterior or posterior cruciate ligament.
The rear Cruciate ligament In particular, it prevents the thigh from moving forward, while the anterior cruciate ligament acts in exactly the opposite way.
Read more on the topic Anatomy cruciate ligament under:
- anterior cruciate ligament
- posterior cruciate ligament
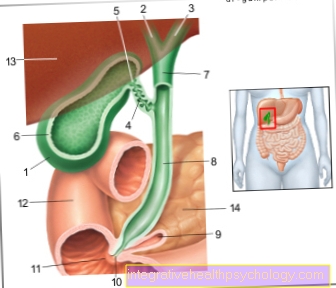
Posterior cruciate ligament illustration

- Posterior cruciate ligament -
Lig. Cruciatum posterius - Inner band -
Lig. Collateral tibial - Inner meniscus -
Meniscus medialis - Shin community -
Corpus tibiae - Calf community -
Corpus fibulae - Outer meniscus -
Lateral meniscus - Outer band -
Lig. Collaterale fibulare - Femur - Femur
- Intergranular pit -
Intercondylar fossa - Inner joint gnar -
Medial condyle - Anterior cruciate ligament -
Ligament cruciatum anterius - Transverse ligament of the knee joint -
Transverse ligament genus - Kneecap ligament -
Ligament patellae
You can find an overview of all Dr-Gumpert images at: medical illustrations
Appointment with a knee specialist?
I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
therapy
Generally the decision is between conservative and surgical treatment one posterior cruciate ligament tear hold true.
This has to be considered and decided individually. It is also important to address the patient and his or her expectations.While older, rather not sporty-oriented people have different expectations with regard to the ability of their cruciate ligaments to exert stress than, for example, competitive athletes, the operation of the posterior cruciate ligament tear is more likely to be induced in competitive athletes than in people who can be symptom-free without surgery.
From a medical point of view, there is currently no clear standard as to whether a posterior cruciate ligament tear should be treated conservatively or surgically. The representatives of both viewpoints have their own opinions, which are discussed again and again.
So there are doctors among them who are convinced that without surgery arthrosis tends to occur earlier than surgery. The advantages and disadvantages are therefore listed below, but nothing seems to be as important as the individual consideration and the associated individual contact of the patient with the attending physician when assessing between conservative and surgical therapy. Only he can ultimately make the individual decision regarding the form of therapy.
Conservative form of therapy for torn posterior cruciate ligament
Important indications for the decision for the conservative one Therapy for a posterior cruciate ligament tear consists mainly of Elongations of posterior cruciate ligament or partial crack. If a patient with a total posterior cruciate ligament rupture is able to compensate for the instability by means of their muscles, the decision is more likely to be on the conservative form of therapy. As a rule, the operation is avoided in patients who are not oriented towards competitive sports and are older than 50 years. Even if ligament injuries are older than 14 days, treatment is usually conservative.
It is important, however, that conservative therapy is used for one posterior cruciate ligament tear can only be successful if the patient carries out the necessary training independently on a daily basis. The patient's motivation is therefore particularly important and must also be discussed with the patient before deciding on the form of therapy.
The conservative form of therapy for the posterior cruciate ligament tear usually begins immediately after the acute pain has subsided with full stress, but in conjunction with an individually adapted plastic splint and physiotherapy. The goal of conservative therapy is that Improving muscle strength through exercises that simultaneously improve the stability of the person concerned Knee joint should improve.
It is the muscles that are supposed to take over the function of the torn cruciate ligament, so the individual assistance and motivation of the patient discussed in the previous paragraph with regard to the success of the conservative therapy of the posterior cruciate ligament rupture must be clarified.
In addition to the actual therapy:
- Stimulation current,
- ultrasonic and or
- Ice treatment
to get integrated. Combinations of these treatment methods are also conceivable for a posterior cruciate ligament tear and aim to improve blood circulation and ultimately also to reduce pain.
Operation of a posterior cruciate ligament tear

Which tendon is ultimately used can be seen multifactorial and individually. The decisions depend on individual indications:
- job
- Sports activity
- Complex knee ligament injury
- Bony avulsion
- Overall status
- Additional injuries
- Cruciate ligament rupture with additional meniscus lesion near the base
Even if the description of the surgical techniques appears to be quite complicated, the success rates appear good to satisfactory, especially in cases without significant additional injuries.
The operative form of therapy is usually followed by consistent follow-up treatment (rehab). These measures can take an average of around 3 months to complete, whereby full exposure is usually only achieved after 6 months.
A posterior cruciate ligament injury is usually a serious injury. The prognoses for regaining full resilience are to be assessed as rather unfavorable, regardless of the decision whether treatment should be conservative or surgical. Either way, the patient needs help and, above all, his patience.
The pictures show the procedure for Cruciate ligament surgery. While the middle third of the patellar tendon including the adjacent bone blocks is usually removed as part of the patellar tendon plastic surgery (picture left), the semitendinosus tendon and / or gracilis tendon are arthroscopically separated from the bone through a small opening in the skin and separated from the respective muscle belly using a "stripper" (picture right). The resulting remnants of the tendons will scar together with the respective environment without any significant loss of function.

As a result of serious accidents, ruptures of the anterior and posterior cruciate ligaments sometimes occur, so that operative both cruciate ligaments replaced Need to become. Please refer anterior cruciate ligament tear. Usually, these two operations are then performed as part of a more complex operation.
The reason for this is not only that an operation then only has to be scheduled once, but above all that if the two operations were separated in time, too much scar tissue would be formed in the meantime, which would make the installation of another cruciate ligament unnecessarily difficult.
The risk of infection with such a procedure is also not insignificant.
Operative is then mostly both by means of the cruciate ligament Patellar tendon (kneecap tendon) as well as the cruciate ligament plasty in the middle Semitendinosus or Gracillis tendon resorted to.
Usually the anterior cruciate ligament is replaced with the patellar tendon and the posterior cruciate ligament with the quadruple semitendinosus tendon. To keep the scarring of an operation to a minimum, the operation should be carried out arthroscopically if possible. Such interventions employ a highly sophisticated procedure.
There one posterior cruciate ligament injury usually represents a serious injury, the prognoses for regaining full resilience are rather unfavorable under both conservative and surgical therapy.
Summary of therapy
Conservative therapy consists in immobilizing the leg affected by a posterior cruciate ligament tear with the help of a special railto allow the parts of the injured cruciate ligament to grow together.
This so-called PTS rail (PTS = posterior tibial support = posterior tibia support) represents a splint for the lower leg with a calf cushion, which acts as a cushion and prevents the lower leg from falling back. This brace for immobilization after a posterior cruciate ligament tear must be worn for a total of six weeks, both during the day and at night.
If there is no pain, a load is possible, whereby Flexing movements never performed as the torn cruciate ligament will otherwise not grow together.
At the end of these six weeks, after a posterior cruciate ligament tear, movement exercises should be performed in the prone position without a splint. The purpose of this training is to strengthen the Thigh extensor (Quadriceps muscle). It is also important to limit the diffraction in the Knee joint:
A maximum of 60 to 70 degrees of flexion may be performed. From the ninth week onwards, it is sufficient to wear the splint at night. From this point on, flexion is possible up to 90 degrees. Complete healing of the posterior cruciate ligament usually takes approximately twelve weeks.
The alternative to conservative therapy for a posterior cruciate ligament tear is surgical treatment.
The indication for an operation is made if the posterior cruciate ligament is torn out, if there are accompanying injuries or if the knee is extremely unstable.
The surgical procedure consists of one arthroscopic treatmentwhich means a reflection of the joint (Arthroscopy) means simultaneous surgical manipulation of the joint structures without complete opening of the joint.
For this purpose, a few small punctures and an approximately four cm long cut are made. A person with a posterior cruciate ligament rupture will have a posterior cruciate ligament repair or PCL- Replacement plastic (PCL = posterior cruciate ligament). Such a plastic is usually made from the patient's own tendons. The tendons of the are preferably used as the material for treating a posterior cruciate ligament tear Semitendinosus muscle or des Gracilis muscle of the injured leg.
This tendon is reinforced with the help of sutures and inserted into pre-drilled channels on the lower leg and thigh at the attachment points of the original posterior cruciate ligament, where it is then fixed. It is fastened with the help of screws and metal plates.
Since these materials are resorbable, i.e. they dissolve by themselves after a certain period of time, it is not necessary to remove the metal at a later point in time.
If the endogenous tendons that are used for cruciate ligament surgery have insufficient tear resistance, man-made materials are used. If there are additional injuries to the knee joint in the event of a posterior cruciate ligament tear, these will be treated in the same session. Back or side Capsule-band structures can also be replaced by the body's own tendons, for example.
After the operation, a drain is placed in the knee joint through which the wound secretion and blood can drain. This drain is usually removed the next day. Overall, the operation for a posterior cruciate ligament tear takes about one to two hours.
After the operation, the further procedure consists of Elevation and cooling of the affected leg.
Stretching movements must not be carried out and physiotherapy exercises for Muscle building of the leg should be started. In addition, the operated person must put on an extension splint for about six weeks.
After this period of time, he receives a movable rail (PCL orthosis) and can start with slow bending exercises in the prone position up to 60 to 70 degrees. Coordination training is also useful. Exercise should be avoided for a year after surgery for a posterior cruciate ligament tear.
If a tear occurs in the surgically inserted cruciate ligament, the therapy consists in the surgical preparation of one Revision cruciate ligament surgery.
The material used in this case is the tendon of the Semitendinosus muscle of the other leg or the tendon of the quadriceps muscle. Sometimes the operation is carried out in two stages. This means that in a first operation, the drill canals of the first cruciate ligament surgery with Bone marrow of the iliac crest (Cancellous plastic) and the actual cruciate ligament plasty is only made in a second session after about three months, as it is then possible to drill again into the bone to anchor the plastic.
If there is already chronic instability after a posterior cruciate ligament rupture, treatment can be either conservative or surgical. The decision depends on the extent of the instability and the complaints in everyday life.
Duration of a posterior cruciate ligament tear

The Time to heal a posterior cruciate ligament tear usually turns out to be relatively time-consuming.
However, as the joint heals, it can usually be subjected to gradually increasing stress. The duration of a complete healing, which includes the stability and functionality of the joint as before the trauma, depends crucially on the extent of the injury, the individual factors of the person affected and the chosen treatment method.
In the case of simple injuries in young patients who are treated conservatively, complete healing can be achieved after about 12 weeks. Surgical treatment of a posterior cruciate ligament tear is chosen if the injury is extremely unstable. The healing time with surgical treatment of the injury is also influenced by individual factors.
However, a healing period of at least 12 weeks can be assumed.
The duration of a sick note that is written due to a posterior cruciate ligament tear usually varies depending on the activity performed. For example, a person who does heavy physical work during their job usually has to be on sick leave longer than other affected persons. Since strict protection of the joint is strived for at the beginning of the therapy, a sick leave of at least one to two weeks can be assumed.
In the course of healing, the injury can be examined. and the sick leave may be extended.
The resumption of physical activity may be delayed beyond the specified times. This depends on the individual healing progress and the type of sport performed.