Symptoms of root inflammation
introduction
The root inflammation, also called Pulpitis designated, is an inflammation of the tooth pulp (i.e. the tooth pulp), which is located within the tooth root. If the tooth nerve is now irritated, it transmits its pain sensations to the brain.
But tooth root inflammation is not only accompanied by pain - also that "thick jaw", a headache and fever can come along with it.
Further information is also available here: Root inflammation - What to watch out for

By mechanical or chemical Charms, But tooth root inflammation can occur mainly through bacteria. The bacteria either enter the tooth through extensive caries or they reach the nerve through enlarged gum pockets during periodontitis. They produce various toxins called Endotoxinswhich damage the body's own cells and cause nerve inflammation.
Read more on the topic: Causes of a root inflammation
Symptoms of root inflammation
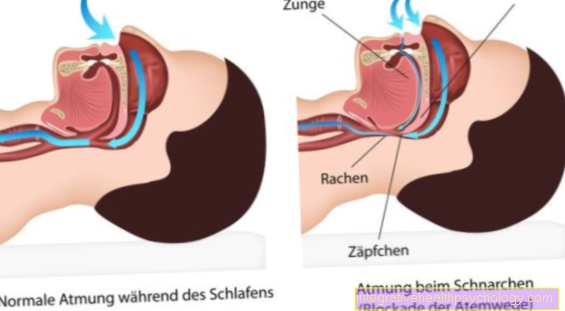
Acute nerve inflammation is characterized by rapidly occurring, knocking and / or throbbing Pain from. In addition, biting causes severe pain. Pain can be relieved by using cold drinks or cold air, such as breathing in forcefully.
If the stimulus is short-lived, pulpitis can, in very rare cases, regress and heal spontaneously. In most cases, however, tooth root inflammation leads to nerve death and chronic inflammation.
Learn more at: Pain in a tooth root inflammation
The fact that a tooth root inflammation can also be completely painless is very important. This means that even a tooth that does not cause any discomfort can still be diseased and must be treated urgently.
These are the typical symptoms of root inflammation:
- pain
- swelling
- a headache
- general symptoms of illness
- Pus formation
- Death of the tooth
The purulent inflammation at the tip of the root can - as already mentioned - run for a long time without symptoms of root inflammation. However, if the body's own defenses are exhausted, the contents of the stove break out, causing great pain and swelling of the tissue. An abscess has developed, the well-known "fat cheek".
Read more on the topic: Pain at the root of the tooth
Thick cheek as a symptom of root inflammation
A thick cheek usually arises in connection with a carious tooth that has not been treated for a long period of time. The cause of this swelling is not the caries itself, but diseases that occur in the course of a caries attack.
Learn more about: A swollen cheek - what does it mean?
The bacteria penetrate the tooth pulp from the dental caries, where they damage nerve fibers that pass from the tooth into the bony jaw.
The result is a tooth root inflammation that sooner or later spreads to the jaw.
The reason for the thick cheek is the accumulation of water in the inflamed tissue (edema). A root inflammation usually brings enormous toothache with it and therefore usually drives those affected to the dentist's office. Over-the-counter pain relievers can help relieve the pain, e.g. Ibuprofen.
Read more on the subject at: Ibuprofen for root inflammation
Headache as a symptom of root inflammation
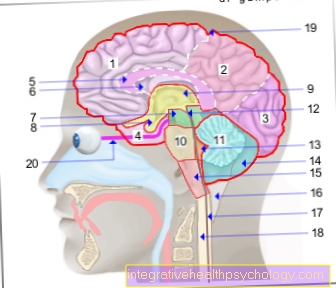
It is quite possible that toothache caused by a tooth root inflammation spreads to other areas and causes other pain. This includes pain like Headache, earache or Jaw discomfort. In addition, neck problems can also be caused by teeth, which is often underestimated.
The most common form of radiation is headache. But how can it be that a tooth causes so many pains? A typical symptom of tooth root inflammation is the thick cheek, the abscess. If this boil is not treated early by a dentist by allowing the pus that is in this swelling to drain through an incision, it can migrate. The inflammation spreads and tries to get into the bloodstream.
The respective direction of spread can definitely lead to headaches. The severity of this headache is variable. They appear at intervals or even continuously. The headache leads to unilateral or bilateral complaints. It is also possible that the entire head area hurts and an exact location of the pain cannot be identified.
The individual perception of these complaints is also different. Those affected are often not even aware that a tooth is the actual cause and the symptoms are dismissed as simple headaches. The result is reaching into the medicine cabinet, where pain medication is supposed to relieve the symptoms without having to go to a doctor who will make the correct diagnosis. But it is precisely this behavior that enables dire consequences to arise.
If the tooth root inflammation is not treated in good time and the inflammation enters the bloodstream, in an emergency, sepsis with organ failure as a complication can occur, which is life-threatening.
Because of these devastating complications, this should be one Do not underestimate "simple" headaches lightly and visit the dentist at an early stage to find the cause and provide targeted therapy.
Read more about the topic here: Bacteria in the blood - how dangerous is it?
Accumulation of pus as a symptom of tooth root inflammation
However, if there is no immediate treatment, the inflammatory processes within the tooth and jaw tissue will continue. Pus accumulates, which penetrate deeper into the bones and can cause severe damage.
At this point the initial pain usually subsides, which is a rather bad sign. The pus can migrate from the jawbone into the surrounding tissue. It becomes particularly dangerous when pus travels towards the eye socket or throat. A tooth root inflammation is therefore always in need of treatment!
Read more on the topic: Purulent tooth root inflammation
Fever and tiredness as symptoms of tooth root inflammation
If a tooth root inflammation manifests itself, so that bacteria from the inside of the tooth reach the bloodstream, the local disease can certainly lead to a fever with an elevated temperature. Fever is always a defense reaction of the body against an attack by germs. Symptoms such as tiredness and exhaustion are not uncommon. In combination with a fever and an increased heartbeat of more than 90 beats per minute, these symptoms can already indicate the onset of sepsis.
Sepsis is generalized inflammation of the body in response to infection with microorganisms such as bacteria, viruses, or others. The immune system tries to fight this inflammation with its own means, whereupon the fever develops. The specific response of the body depends on the type of germ.
Other symptoms besides an increased heartbeat are an increased respiratory rate, confusion and severe exhaustion. The specific inflammation parameters in the blood, such as B. the white blood cells are greatly increased. These symptoms can increase so much that the body can no longer fight the infection and the organs gradually fail. This condition is acutely life-threatening and can lead to heart failure and thus death.
At the first signs of a temperature increase above 38 degrees Celsius, it is advisable to consult a doctor, from a temperature above 40 degrees Celsius, extreme caution is required. The doctor prescribes antipyretic drugs. This condition can be life-threatening, as a temperature of over 42 degrees Celsius is no longer tolerable for the body.
What are the symptoms of a dead tooth?
As soon as a tooth is insensitive to heat and cold, it is called a dead tooth. The cause of the death are bacteria that inflame the nerve. The inflammatory process in the tooth pulp causes the blood and nerve vessels contained there to die off and the tooth is no longer supplied with nutrients.
Decomposition gases form inside the tooth, which cannot escape and lead to severe pressure pain. The tooth pounds, is sensitive to the bite and the pain often radiates to the face and head regions. The formation of an abscess is also possible. This encapsulated boil is swollen, painful, heated and reddened.
Read more on the topic: Abscess on the tooth
Sometimes the inflammation finds its way out and does not form an abscess, but a fistulous duct. This allows the pus secretion to drain inside or outside the oral cavity. Affected people perceive the end of the fistulous duct as a pimple that is sensitive to touch.
See also under: Fistula on the tooth
In general, non-vital teeth lose their fluid and become brittle. As a result, these teeth are at great risk of breakage and are no longer as chewing stable as the vital teeth. If a dead tooth breaks off, the broken edge can not only be sharp and annoying, it can also cause pain. If the pulp containing the vessels is opened by the fracture, bacteria can penetrate the tooth and infiltrate the tissue under the tip of the root. The bone can become inflamed and the tooth loosened enough to fall out.
In order to alleviate the various symptoms of a dead tooth at an early stage and to preserve the tooth for a long time, it should be treated and crowned as soon as possible in order to restore it as a full member of the dentition.
You can find more helpful information here: The dead tooth
If the root inflammation is left untreated, the pain appears to improve after the nerve dies. The bacteria colonize the pulp up to the root tip and then spread in the surrounding bone. This phase is often painless. Various secondary diseases can now result from a dead tooth. Inflammation that spreads to abscess is possible, as is radicular cyst or bone marrow inflammation (Osteomyelitis).
Most often, a radicular cyst forms first. The progressive inflammation is encapsulated around the tip of the root, but continues to expand, increasing in size and dissolving the surrounding bone. Because of the dead tooth, this process is painless. Under certain circumstances, the person concerned suffers from bite pains or increased tooth loosening is noticeable. In the dental practice, a so-called radicular cyst can be found on the X-ray.
Is pain after root canal treatment a symptom of root inflammation?
Severe pain and impairment can occur not only before or during treatment of a tooth root inflammation, complaints are also possible after a root canal treatment. It should be remembered that root canal treatment is only the attempt the tooth is to be preserved, but there is no guarantee that this form of therapy will work.
During dental treatment, the inflamed tissue is removed from the inside of the tooth, the root canal is disinfected and treated with a drug. The now empty root canals are hermetically sealed with flexible gutta-percha points that are reminiscent of flexible rubber pencils. An Art glue acts as a binding agent between the gutta-percha points and the tooth wall, in order to prevent bacteria from re-entering the tooth and to guarantee the absolute density of the root filling.
It is normal that the tooth may still have pressure problems for a few days after the root filling has been plugged and the therapy has ended, but these will subside completely after approx. 14 days. It can also happen that the root filling material pushes itself beyond the root tip and the surrounding tissue becomes inflamed. This can lead to uncomfortable pain. The region around the tip of the root can also be mechanically irritated by the instrumentation with the thin files. This is nothing to worry about, it is a very common occurrence. The tissue quickly recovers from it.
It is also possible that the tooth becomes inflamed after the end of the root canal treatment because the canal was not 100% disinfected or it was not sealed airtight. The tooth is then tender and painful when chewing. Symptoms such as swelling of the gums around the root of the affected tooth and severe reddening are conceivable.
Then going to the oral and maxillofacial surgeon is often the last option to save the tooth. This treats the tooth with a tip resection by cutting open the gums and removing part of the tooth root with the inflamed tissue.
So if after a root canal treatment there is pain or increased sensitivity to longer than 2 weeks persist or worsen steadily, there may be renewed root inflammation and a visit to the dentist is necessary.
More information is available here: Pain during a root canal treatment
Diagnosis: How do you recognize a tooth root inflammation on the X-ray?
Can you already see on an X-ray in the dental practice that the tooth root is inflammation? Yes, this is possible if the inflammation in the area of the root tip has been around for a little longer. However, if the tooth root inflammation is still in its early stages and the bones are not affected, the X-ray image is completely normal.
Only after the dentist has knocked on the teeth in question (Percussion test) and by a cold test (Vitality test) has located the affected tooth, he takes a small x-ray of the tooth, which also shows the entire root and the surrounding tissue. The characteristic feature on an X-ray of a tooth root inflammation is a dark round shadow below the tip of the root.
You might also be interested in: X-ray of teeth
The X-ray image is a composition of different gray values, each of which is created by the penetration of the rays through the tissue and thus characterizes each area. Metal-tight structures (e.g. a Golg crown) hardly let any radiation through and therefore appear white, structures such as bones and teeth allow more radiation to pass through and appear gray.
If there is now a shadow below the tip of the root where there should actually be bone, this speaks for inflammatory tissue. This is soft tissue that allows the X-rays to pass through almost unhindered and thus appears almost black. This inflammatory tissue can penetrate the surrounding bone and break it down (then the inflammation of the tooth root has already caused osteomyelitis). If left untreated, the causative bacteria can enter the bloodstream and lead to diseases such as endocarditis or heart attack.
You can find out how the dentist now proceeds here: Treatment of root inflammation
Recommendations from our editorial team
- Everything about treating a tooth root inflammation
- Do antibiotics help with root inflammation?
- Can you do sports while having a root inflammation?
- Pain in a tooth root inflammation - what helps?
- Root inflammation during pregnancy
- Root canal treatment - you should know that!

.jpg)