Pain therapy use of the Racz catheter
Synonyms

- Racz pain catheter
- Racz pain catheter
- Spinal catheter
- Racz - spinal catheter
- minimally invasive spinal catheter according to Prof. Racz
Definition of Racz catheter
Of the Racz catheter was founded in 1982 by the Texas anesthetist and pain therapist Prof. Gabor Racz developed.
The Racz catheter technique is a minimally invasive procedure for treating chronic back pain different origins.
The Racz catheter is a special catheter (thin tube) which, unlike conventional catheters, has a metal guide wire and can be used to pinpoint the location of the pain Spine controls.
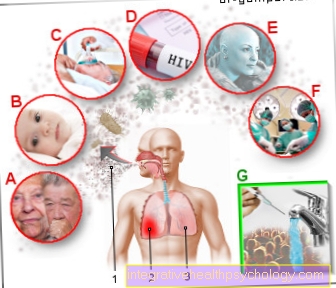
indication
The Racz catheter is a not undisputed procedure, both in terms of the technique of the procedure and in terms of its therapeutic uses. It is not a panacea for chronic back pain and should be reserved for all root irritation symptoms (radiculopathies).
Radiculopathy is a painful irritation (mechanical, chemical) of a nerve root in the spinal cord. Clinically, such an irritation is noticeable, for example, in the area of the nerve roots of the lumbar spine, through sciatic pain, also known as lumboischialgia in technical terms.
Lumboischialgia refers to back pain in the spinal column, which radiates from there over the buttocks into the leg, sometimes to the foot and toes. Depending on the nerve root affected, there may also be typical deficits in reflex behavior, sensation and strength development. Leg pain is often felt more excruciating than back pain.
Even if many wear-related (degenerative) changes can lead to nerve root pain, the Racz catheter should, according to the consensus of well-known orthopedic specialists, be reserved for the following diseases:
- Herniated disc with root irritation symptoms
- Disc protrusion with symptoms of root irritation
- Perineural (around the nerves / spinal cord) scarring (med. Referred to as postnucleotomy syndrome) with symptoms of root irritation
In the case of a herniated disc / protruding disc (nucleus pulposus prolapse / protusion), leaked disc tissue presses on the nerve root and leads to mechanical and chemical irritation with an inflammatory reaction of the affected nerve root and corresponding radiculopathy.
Perineural scarring often occurs after disc operations (postnucleotomy syndrome). The scars caused by the surgical trauma can wall nerve roots or the spinal cord and lead to irritation of the nerves through tension and pressure.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work.On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
From Gerdesmeyer et al. In 2005, the following inclusion criteria (indication) for the use of the Racz catheter were formulated:
- Chronic radiculopathy, unsuccessfully treated conservatively, for protruding or herniated discs or after disc operations
- Minimum age: 18 years
- Evidence of root irritation on imaging (MRI)
- 3 months unsuccessful conservative therapy
- Time window of> 6 weeks after the last (peridural) infiltration near the spinal cord (syringe).
- Pain assessment of> 4 on the visual pain analogue scale (VAS) (note: the patient should give a subjective assessment of his pain with a range of 0 = no pain and 10 = strongest, unbearable pain)
The exclusion criteria (contraindication) include Gerdesmeyer et al .:
- Indication for surgery in case of neurological deficits (loss of strength, loss of feeling, etc.)
- Rheumatic diseases / metabolic disorders
- Relevant inflammation
- Known neoplasms (neoplasms = tumor diseases) in the operating area
- Vertebral fracture
- Immunosuppressive therapy (e.g. methotrexate)
- Long-term cortisone use
- Lack of evidence of the disease on imaging
- Coagulation disorders / use of anticoagulant drugs (Marcumar ®, ASS ®, Plavix ®, etc.)
- Clinically relevant spinal stenosis
- Time window of <6 weeks after the last (peridural) infiltration near the spinal cord (syringe).
- Allergies to local anesthetics, hyaluronidase, X-ray contrast media
- Pregnancy or breastfeeding
- Clinically relevant genitourinary (lower urinary tract) or sexual dysfunction
Surgical procedure
In principle, the surgical procedure can be carried out on the cervical spine, thoracic spine and lumbar spine using a modification of the access technique.
By far the most common application is on the lumbar spine.
A natural opening point of the vertebral canal in the area of the sacrum is sought under sterile conditions (sacral canal / hiatus sacralis). This point is located in the course of the gluteal fold above the arched transition to the coccyx. A local anesthetic is placed in the entry area of the catheter.
First a rod sleeve (trocar) is inserted and the correct position is checked under X-ray control and the use of contrast medium. The special catheter is then introduced and placed at the desired location. The position is checked again by x-rays with a contrast medium (epidurography).
Then the medication is injected (local anesthetic, 10% saline solution, cortisone, hyaluronidase). After rinsing the catheter, it is securely attached to the skin, a bacterial filter is put on and a sterile bandage is applied.
Over the next two days, the catheter is washed up with medication and then removed.
advantages
At the Racz catheter is a minimally invasive surgical procedure in which no new soft tissue damage (Musculature, Ligaments, etc.) takes place and thus a renewed scarring should not occur. Therefore, the indication for catheter technology is made before a possible open surgical intervention.
The reason for this is the moderate to poor results in follow-up interventions (revisions) due to persistent radiculopathy after open disc interventions. Pain relief can only be achieved in approx. 50% of all patients who have been openly operated on for the first time. With the second follow-up operation, the success rate is reduced to approx. 20%.
The idea of Racz catheter is understandable. Existing scar tissue (connective tissue) is to be dissolved through the precise application of the connective tissue dissolving enzyme hyaluronidase to the affected nerve root. By injecting 10% saline solution, a herniated disc / protruding disc can be made to shrink by osmotic dehydration, relieving the nerve root of the disc pressure. Additional injections of cortisone and local anesthetic have a pain-relieving and anti-inflammatory effect and are said to lead to a decongestion of the nerve root, which results in a relative gain in space.
criticism
The Racz catheter technology is not without controversy, especially when it comes to the range of indications.
Since it is an expensive, individual health service that cannot be billed through the health insurance company, some claim that greed for profit has led to an unjustified expansion of the range of applications.
Others question the effectiveness of the method itself.
In addition, the commonly used drugs (hyaluronidase and 10% saline solution for use in the spinal canal are not approved.
In summary, the points of criticism include:
- Expensive surgical method
- No billing through the health insurance possible
- The drugs hyaluronidase and 10% saline solution are not approved for use in the spinal canal.
- No need for precise drug application
- X-ray exposure
- Risk of injury from the relatively rigid catheter system
- Chemical nerve irritation from the drugs hyaluronidase and 10% saline solution itself
- Insufficient scar tissue dissolving effect of hyaluronidase
- No persistent shrinkage of herniated discs with 10% saline solution. Only short-term effect.
Complications
With careful compliance with hygiene and a skilled surgeon, complications are rare.
Possible complications are:
- Infection / meningitis (meningitis)
- Hematoma in the spinal canal with pressure on the spinal cord from a vascular injury
- Catheter-related injury to the skin of the spinal cord
- Broken catheters.
- Application of medication and contrast medium into the spinal cord tube
- Neurological complications up to paraplegia
- Allergy to drugs used up to circulatory shock
Results
Since there are no placebo-controlled, prospective studies on Racz catheter technology to date, its use is classified as experimental. Various working groups have been able to demonstrate a positive benefit of this form of therapy for radicular pain.



.jpg)