Tendonitis of the tibialis posterior tendon
What is tendinitis of the tibialis posterior tendon?
Tendonitis of the tibialis posterior tendon is inflammation in a connective tissue area of the muscle in the posterior tibial muscle that connects the muscle to the bone. One can also speak of tendovaginitis, in which the protective covering that surrounds the tendon is also inflamed.
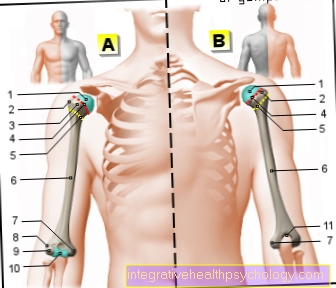
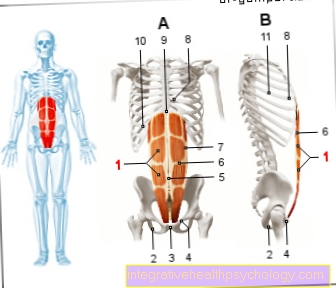
The tibialis posterior muscle is part of the deep lower leg muscles and plays an important role in the extension of the ankle, the supination of the lower ankle and in the structure of the longitudinal and transverse arches of the foot.
Read more on the topic: Tibialis posterior tendon or Tibialis posterior muscle

Concomitant symptoms
Signs of tendinitis are:
- Pain and pulling in the muscle and along the tendon
- Reduced strength
- Flat foot
- Failure of the tibialis posterior muscle
The first signs of tendinitis are usually pain and pulling in the muscle and in the course of the tendon. The pain often worsens with exercise. The pain usually manifests itself as severe pressure pain in the area of the inflammation. In the later course of the disease, the strength of the foot can be reduced and ultimately lead to a change in the position of the foot in the form of a flat foot. Chronic inflammation can tear the tendon, causing acute posterior tibial failure with a sudden flattening of the foot.
Further symptoms depend on the underlying disease. In the event of an infection or as part of an immunological disease, there is often fever, reddening and swelling in the tendon area.
Read more on the topic: Tendinitis
treatment
The most important treatment is to stop the offending stress and let it rest for some time. If the pain is acute, the area can be cooled with an ice pack. Exercise should not be restarted if there are still symptoms. If the pain persists, taking pain relievers and anti-inflammatory drugs (NSAIDs), such as ibuprofen or diclofenac, may help.If the pain is severe, a cortisone injection into the tendon area can also be given by the doctor.
Physiotherapy can also help accelerate the healing process. Exercise treatments and alternative training plans can be worked out with the therapist.
Shoe insoles (orthotics) and bandages can be helpful, in particular to reduce incorrect loads. In addition, shock wave therapy or the use of kinesiotape can lead to an improvement.
If all of these measures do not lead to improvement within a few weeks, stiffening of the ankle with the help of plaster of paris or splints can be appropriate to achieve complete relief of the tendon.
Surgical therapy is usually necessary if the tendon ruptures.
You might also be interested in: Anti-inflammatory drugs
Healing time
The duration of tendinitis depends on the underlying cause. In the case of acute inflammation caused by excessive stress, short-term immobilization and cooling can lead to healing within a few days. It is important, however, that you do not start again directly at 100%, but slowly approach the original load again.
Chronic inflammation due to infection or immunological reaction can take several weeks to months to heal. Pain-free or inflammation-free intervals can also occur. If there is still no improvement after several months, surgical treatment can be carried out. However, this entails immobilization and subsequent build-up training over several months.
Read more on the topic: Tendinitis in the foot
forecast
In the case of an acute inflammation of the tendon, after sufficient rest and cooling, complete healing without consequences can occur within a short time.
However, if it is a recurring, chronic inflammation, symptoms can persist for months to years, whereby smaller and smaller loads could lead to pain. Perhaps alternative training should be worked out or another sport should be practiced. Further stress on a chronically inflamed tendon can tear it, which in turn leads to a longer healing process. In addition, a loss of function of the tibialis posterior muscle can lead to a flat foot.
Read about this too: Tendinitis on the ankle
Causes of tendinitis
Tendonitis in the area of the tibialis posterior tendon can have various causes:
- constant overload
- Weakness of the tibialis posterior muscle
- immunological reactions
- Injury to the leg
- Bacterial or viral infections
The most common is tendon wear and tear caused by constant overload. It is not uncommon and occurs mainly in middle-aged women and young athletes, especially runners. Inflammation can occur, especially when the calf is put under prolonged stress, for example when running uphill or during a marathon. Other causes can include being overweight and prolonged incorrect stress, for example wearing poor or old running shoes or running on hard ground be.
In diseases such as flat feet, in which the tibialis posterior muscle becomes weak, the foot can be put under incorrect stress and, as a result, tendinitis.
Furthermore, immunological reactions can also be the cause of tendinitis. Diseases such as rheumatoid arthritis or gout are associated with inflammation of the tendons, muscles and joints. They often lead to long-lasting pain and swelling in the muscle area.
Finally, tendinitis can also be the result of an injury to the leg, for example a tendon tear or broken bones.
Bacterial or viral infections are only the cause in rare cases.
Read more about here: Causes of Rheumatoid Arthritis
diagnosis
Tendonitis is usually diagnosed based on a medical history and physical exam by a doctor. Meanwhile, the doctor will do some function tests on the muscle and examine the area of the tendon for possible redness, swelling, overheating, or tenderness.
An example of such a functional test is, for example, the isometric test, in which the doctor pulls the foot downwards slightly while the patient pulls it upwards-outwards or up-inwards. If the tibialis posterior tendon becomes inflamed, this leads to pain in the calf. Standing on your toes can also cause pain.
Usually, a physical exam is sufficient to suspect tendonitis, but in some cases additional tests may be needed to confirm the diagnosis. As part of a blood sample, inflammation parameters could be detected in the blood. Magnetic resonance imaging (MRI) or ultrasound can also help.






















.jpg)

