Peroneal nerve
Synonyms
Peroneal nerve, fibular nerve
introduction
The Peroneal nerve, also Fibular nerve called, is responsible for the nervous supply of the fibula and goes together with the Tibial nervewhich supplies the tibia, emerges from the sciatic nerve.

Course of the peroneal nerve
The Peroneal nerve arises from that Sciatic nerve on the back of the thigh a little above the hollow of the knee and then pulls as a lateral branch behind the head of the fibula Fibular islet. In the hollow of the knee, the blood vessels of the knee are located in close proximity to the nerves. There it then divides into its branches, the Deep and superficial peroneal nerves on.
The Peroneal nerve profundus then leaves the fibular islet through the Septum intermuscular anterius and thus changes to the Extensor box, in which the Extensor muscles of the lower leg and of the foot. The nerve runs parallel to blood vessels and in its course gives off motor branches to the muscles of the extensor box as well as sensitive branches to the skin between the big and second toes, where it ends.
The Peroneal nerve ssuperficialis remains in the fibular islet and runs parallel to the Musculus fibularis longus and Musculus fibularis brevis, which he supplies by motor. The nerve runs along the lateral lower leg without direct reference to the blood vessels and reaches the inner dorsum of the foot via the outer ankle, which it supplies sensitively.
Common peroneal nerve
The name of Common peroneal nerve means something like "the common nerve of the fibula" and makes that possible Lifting the foot as well as the outer lateral edge of the foot and the Extension of the toes.
Anatomically denotes the Common peroneal nerve the first share from the Sciatic nerve emerging Peroneal nervethat has not yet split into its branches.
Branches of Common peroneal nerve:
- Nervus cutaneus surae lateralis: is responsible for the nervous supply of the skin of the lower leg on the outer side and to a certain extent also the back and contributes a not inconsiderable part to the formation of the Sural nerve at.
- Deep peroneal nerve
- Superficial peroneal nerve
Deep peroneal nerve
The Deep peroneal nerve arises from the Common peroneal nervesee the Deep peroneal nerve is the name of a deep-lying nerve. It runs in the Lodge of the extensor muscles of the lower legwhich lies roughly in front of the connective tissue plate between the tibia and fibula.
On its way to the back of the foot, it repeatedly gives off smaller nerve branches to the muscles. It primarily supplies muscles that are necessary for those directed towards the shin Elevation of the foot and toes are responsible. These muscles include:
- Extensor hallucis brevis muscle
- Extensor digitorum brevis muscle
- Tibialis anterior muscle (anterior tibial muscle)
- Extensor hallucis longus muscle
- Extensor digitorum longus muscle
Superficial peroneal nerve
The Superficial peroneal nerve also goes from the Common peroneal nerve emerged. It is a superficial nerve and runs laterally on the lower leg with reference to the foot extensor muscles on the outer dorsum of the foot.
It supplies the muscles of the fibular group:
- Musculus fibularis longus
- Musculus fibularis brevis
In addition, it also cares for various areas of skin on the lower leg, especially the back of the foot.
Symptoms of nerve damage
Possible symptoms of the Peroneal nerve can cause include:
- Pain in the hollow of the knee, the outer side of the lower leg and the foot,
- Numbness on the back of the foot or between the first two toes,
- Paralysis of the extensor muscles to lift the toe and straighten the toes.
Pain
Pain from the Peroneal nerve can occur along its course from the hollow of the knee to the back of the foot. You can express yourself very differently, e.g .:
- Pain at rest
- Pain can be triggered by pressure
- localized pain
- radiating pain
In some cases, a reduced perception of pain, temperature and pressure can be observed downstream of the painful area. This may indicate a pressure point or a fresh lesion in the nerve and surrounding tissue, such as an operation or injury to the leg.
Furthermore, severe pain can occur in a so-called compartment syndrome of the extensor compartment of the lower leg, in which an increase in pressure causes compression of the Deep peroneal nerve can come. If no therapy to relieve pressure is initiated here, the nerves and other structures can die.
Read more on the subject at: Lower leg pain.
Peroneal palsy
It comes to damage of Peroneal nerve, so can one Paresis, so paralysis of the muscles supplied by the nerves. The affected muscles vary depending on the location of the nerve lesion and the affected nerve fibers.
Paresis can result from a direct injury to the nerve, for example in the case of a broken bone in the fibula, a deep cut on the outside of the lower leg or during an operation. Compression of the nerve due to an increase in pressure in a muscle box (e.g. due to muscle swelling), another mass or an improperly applied plaster cast can lead to nerve damage. Last but not least, a Herniated disc at the level of the lumbar spine among other things the paralysis of the Peroneal nerve trigger.
The earlier the Peroneal nerve Damage as it progresses, the more muscles are affected by the paralysis.
At a Lesion of the Common peroneal nerve falls the complete Extensor muscles of the lower leg, resulting in a Equinus position and a "stepper walk" leads, since the tip of the foot can no longer be actively lifted. In addition, the sensitive care of the back of the foot out.
In the case of isolated damage to the Deep peroneal nerve are still mostly those Extensor muscles of the lower leg affected and it comes to Equinus with stepper gear and to Sensory disorder between the first two toes.
On the other hand, it is only the muscles of the Superficial peroneal nerve Affected by the paralysis, the tip of the foot can still be raised. However, it comes to the lowering of the outer edge of the foot in relation to the inner edge of the foot, what is called Supination designated. Furthermore stands a Numbness on the back of the foot in the foreground.
If the nerve branches are damaged later in the course, some of the muscles that are connected in front of them are still supplied with nervous supply and the paralysis is no longer too severe.
causes
The cause of the pain is irritation or damage to the peroneal nerve. This can be done for example by increased pressure on the nerve in the foot extension box, for example at the Compartment syndrome, happen, which in the further course can lead to the death of the nerves due to insufficient blood supply. Often, work that involves kneeling on the floor, for example tiling, also causes discomfort due to pressure on the nerves. A direct damage (e.g. cutting) of the peroneal nerve can occur in a surgery or one injury of the leg. Also one Polyneuropathythat begins in the periphery of the body may be behind damage to the peroneal nerve.
Diagnosis
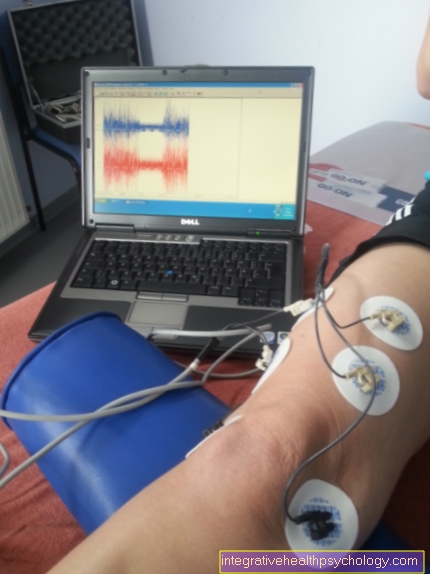
There are the following options for diagnosing possible damage to the peroneal nerve: With a EMG (electromyography) the electrical muscle activity of the muscles supplied by the nerve can be assessed. A measurement of the nerve conduction velocity can be carried out by a ENG (electroneurography) from branches of the peroneal nerve (Common, deep and superficial peroneal nerves) to get information about the nerve conduction velocity. Also the neurological examination the extensor muscles on the lower leg are extremely helpful in assessing the integrity of the peroneal nerve.
therapy
The only complaint is a compression of the nerve without permanent damage Basically, this can recover again through relief.
However, the nerve is irreversible and badly damagedso that there is a reduction in strength of the supplied muscles up to paresis, sometimes only a compensatory build-up of the surrounding muscles can be used for therapy. A restoration of the initial state is usually not feasible.
forecast
Nerves are very sensitive and can usually no longer heal completely in the event of major damage. This means that if there is severe nerve damage, there may well be remnants of muscle paralysis and numbness.