That's how dangerous a fistula in the mouth is
introduction
For weeks you feel an unpleasant pain in the oral cavity, especially near a tooth. The pain plagues you very much, but a visit to the dentist has not yet been possible. And suddenly the pain disappears. Has the inflammation around the tooth subsided?
How can the sudden decrease in pain be explained? A fistula can be the possible cause. It could explain the decrease in inflammation by its tubular connection. But what exactly is a fistula?
Read more on the topic: Fistula on the gums

definition
A fistula is a tubular or network-like connection between an internal hollow organ (this can also be an abscess) and other organs, or to the surface of the body. If it is the former, one speaks of internal fistulas, such as those that can develop between the stomach and colon. The latter is called an external fistula.
This can be from the intestines to the skin, or, referring to the oral cavity, from an abscess that is now connected to the mucous membrane. Fistulas don't just happen in the mouth, they can develop anywhere. Various examples are: intestinal fistulas, anal fistulas, vaginal fistulas or also fistulas between vessels, such as the carotid-sinus-cavernosus fistula. The latter is a vascular abnormality between arteries and the venous blood conductors of the brain.
All fistulas are not present from birth, but arise in the course of a clinical picture and are pathological. Looking more closely, one can distinguish two types of fistulas. The tubular and lip fistulas.
The tubular fistula is lined with granulation tissue (young connective tissue that is penetrated by many capillaries and thus appears granular). It can heal on its own after the cause has been eliminated. It looks different with lip fistulas. This has an epithelial lining (cell layer) and must be surgically removed even after the cause has healed.
There are three causes that cause a fistula to form. On the one hand, this includes chronic inflammation, such as Crohn's disease (this is a bowel disease that can affect the entire digestive tract). On the other hand, acute inflammation, such as an abscess, can also form a fistula.
An abscess is a newly formed capsule in tissue that contains pus inside. The third possibility is an external influence, such as an accident or an operation.
The task of the fistula is clearly defined. With its tubular, hollow shape, it creates a new way to remove the pus. If an abscess and the inflammation persists, so that new pus is added, either the abscess bursts or the body forms a drainage system, namely the fistula.
Find out more at: Fistulous duct
Special case of the oral cavity
In addition to the fistulas in the intestinal area, fistulas can of course also form in the oral cavity. These can arise due to an untreated root inflammation. This has different causes, such as poor oral hygiene, so that the bacteria attack the tooth and decompose its hard tooth substance until they reach the pulp.
External factors such as smoking, unhealthy diet or chronic illnesses can have a positive effect on the development of caries and thus also possible inflammation. Wounds in the oropharynx, but also pressure points caused by incorrect dentures, can be the cause of a fistula. The body tries to get rid of the unpleasant intruders and activates the immune system, which manifests itself with an inflammatory reaction.
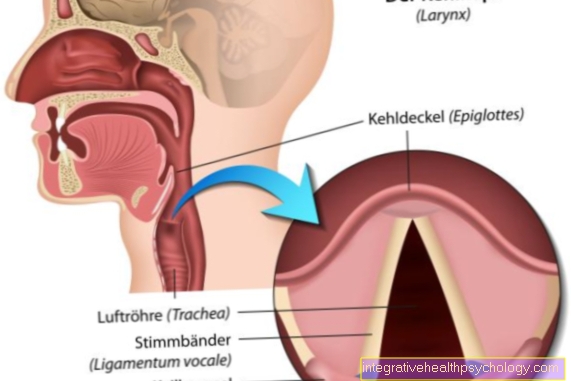
If the inflammation is left untreated, it increases, the tooth root dies and the bone tissue can be attacked. If the abscess, i.e. the focus of inflammation, has a fistula that creates a connection to the oral cavity, the pus can empty into the oral cavity. The situation is different if the accumulation of pus spreads into the throat, as there is a risk of suffocation.
If the pus has flowed through the fistula into the oral cavity, one could assume that the problem should have been resolved, because the previously very unpleasant pain has suddenly disappeared and the pus has also drained. The fistula allows the pus to escape to the outside, but does not ensure that the inflammation also disappears. This persists, so that it spreads in the bone and destroys tissue.
The easing of pain can therefore be a dangerous illusion. The fistula or its opening into the oral cavity is not really visible. When it is visible on the oral mucosa as a small pustule from which the fluid pours. There is no longer any real pain, but you can feel that something seems to be wrong in the affected area, but you cannot assign it precisely.
Also read: Fistula on the tooth
Pain and pain progression
At the beginning, the symptoms are relatively minor and tolerable. One does not notice the upcoming fistula formation and assumes a normal dental problem.
Over time, however, the pain increases, may knock and a feeling of tension develops. Outwardly it can only be recognized by a slight swelling in the affected area. As soon as the pressure is so strong that the contents of the abscess drain through the fistula into the mouth, the pain will decrease. If left untreated, however, this can occur again due to the progressive inflammation.
Treatment of the fistula is eagerly awaited by most patients, as the pain and the feeling of tension turn out to be very unpleasant.
diagnosis
In general, it is advisable to see a dentist at the first symptoms of pain, as this will stop the caries from progressing at an early stage. It is therefore not necessary for an abscess to develop, which then drains into the oral cavity via a fistula.
The doctor treating you will first examine the painful area in order to identify a swollen area. The vitality of the tooth is also checked. This allows conclusions to be drawn about the condition of the tooth root. Is it still vital or already dead?
The safest way to examine an inflammation and its dimensions, which are not externally visible, is an X-ray. The dentist will arrange for the image to be taken and can then examine the inflammation using the image. The further steps depend on the respective situation. If the inflammation is still manageable, a root canal treatment may be sufficient. However, if it is very advanced, it may be necessary to extract the tooth.
If there is a fistula, i.e. also an extended stage of the inflammation, the tooth and the entire inflamed tissue are removed. When the inflammation is removed, the fistula will heal on its own. Preserving the tooth, despite the formation of a fistula, is only possible if only the root is inflamed. The important thing is to remove the inflamed tissue and stop the cause.
This allows the fistula to open up and empty. The purulent liquid is sucked off with a suction device so that it does not spill into the oral cavity. Then the cause is treated, for example the inflamed root tips are removed, and the healing process is supported with antibiotic therapy. Home remedies for the fistula are not advisable, as only opening the fistula and stopping the purulent processes can prevent worse. Even if the pain is relieved, the cause is still there.
Symptom of pus
Pus is a classic symptom of fistulas in the mouth and always when the fistula or the fistula duct has made its way from the focus of inflammation to the surface of the mucous membrane.
The fistula or the fistula itself is a means to an end: the deeper inflammatory focus, in which pus forms, wants to get rid of the inflammatory secretion. One solution is to create a passage through the tissue up to a surface through which the secretion, i.e. the pus, can then be released or transported away. As a rule, however, fistulas in the mouth are already noticed by an inflammatory change in the area of the oral mucosa, i.e. before pus can finally be seen and tasted.
therapy
After a fistula in the mouth area has been diagnosed by the dentist, there are several ways in which it can be treated.
First and foremost, it is about containing the spread of the infection and the inflammatory process. To do this, the dentist first opens the pus bubble that has formed in order to suck out the contents. This immediately relieves the patient of the painful feeling of tension. In the next step, antibiotics are administered locally or orally (in tablet form). These usually have to be taken for a period of time after the dental treatment in order to kill the remaining bacteria.
To check the progress, an x-ray is made on which the attending physician can assess the spread of the inflammation in order to decide whether an additional surgical measure is necessary.
If the inflammatory process is limited to the tooth root, tooth extraction can still be avoided by performing a so-called root tip resection, in which the tip is removed from the rest of the tooth root under local anesthesia. However, if tooth tissue is affected, the affected tooth must be extracted to prevent it from spreading to the jawbone.
Home remedies
The treatment of choice for a fistula in the mouth is to remove the focus of inflammation as quickly as possible and to remove the entire fistula duct with the accompanying use of antibiotics. Only that leads to definitive healing.
Conservative treatment, for example through the use of home remedies, is not advisable, as the progressive spread of the fistulas and inflammation can be dangerous. This is at most also advisable to accompany the symptom relief, for example the use of disinfecting and pain relieving mouthwashes.
Treat fistulas in the mouth yourself
Treating fistulas yourself, or piercing the purulent focus yourself to drain the accumulation of fluid, is not advisable and should only be done by a doctor.
The exact localization of the fistula is difficult to determine and the unpleasant pain is usually the main focus, so that additional pressure with a sharp object should not be used. Non-sterile instruments can further stress the focus of inflammation. In addition, the cause is still there and relieving the pain could lead you down the wrong path.
The pus that flows out should also best be sucked off and not pour into the oral cavity. In general, abscesses in the head, throat and ears area should never be treated by yourself, as the bacteria migrate to the brain and trigger meningitis there. Treating the fistula yourself is therefore not advisable.
Should you puncture a fistula?
As a rule, the treatment of choice is surgical opening and emptying, as well as the complete removal of the entire fistula. However, this procedure is to be left to a specialist; independent manipulation in the oral cavity and an independent attempt at opening should be avoided.
The attending dentist or an oral surgeon removes the fistula under optimal conditions and usually initiates accompanying therapy with antibiotics. It is important to know that in the case of a fistula it is usually not enough to open it and empty it, even if the symptoms improve immediately afterwards.The focus of inflammation as well as the entire and complete fistula duct must be removed, otherwise it can form again.
Fistulas with different localization
Fistula on the gums
The causes of fistulas on the gums are usually inflammation in the area of the tooth root tip, which spreads over time and forms an inflammatory duct in the gums (fistula duct), which can then sometimes open up on the surface of the gums. It is therefore a kind of connecting passage between a cavity (root tip) and a surface (gum).
At the beginning of the fistula formation it is not always easy to recognize, only in the course do inflammatory gum swellings develop or when the fistula duct comes into contact with the surface due to the discharge of purulent secretion.
Read more on the topic: Fistula on the gums
Fistula on the palate
Fistulas in the mouth can spread anywhere, including the palate, for example. A source of inflammation in the mouth that spreads over time is sufficient. The germs can spread, among other things, in the form of a connecting passage between the cavity (focus of inflammation, e.g. in the area of tooth roots) and the surface of the mucous membrane (palate).
These passages are usually only noticed through inflammatory changes in the oral mucosa, for example through redness, swelling and pain in the area of the palate or even through the discharge of purulent secretion.
Fistula on the floor of the mouth
Fistulas can also develop in the floor of the mouth. If a focus of inflammation develops somewhere in the area of the floor of the mouth, one possible solution for the body to remove the developing pus is the formation of a fistula, up to the surface of the mucous membrane in the area of the floor of the mouth, through which the pus can empty.
Fistulas in the area of the floor of the mouth can both have an origin of inflammation in the area of the teeth, but inflammations in the area of the lower jaw bone or the soft tissue in the floor of the mouth are just as possible.
Fistula in the mouth after root canal treatment
Fistulas in the mouth can sometimes develop after a root canal treatment.
The reason for the formation of a fistula is always an active focus of inflammation. Since a root canal treatment is initiated in most cases due to a root inflammation, there is thus a focus of inflammation. If this cannot be completely repaired as part of the root canal treatment or if a new focus of inflammation develops in the area of the treated tooth, this can subsequently contribute to the formation of a fistula.
You may also be interested in this topic: Antibiotics after a root canal treatment
Fistulas on the lip
Fistulas can not only appear in the area of the teeth or in the vicinity of a tooth root, but can also be found in other places in the oral cavity, including the lip. If you notice such a fistula, it is advisable to visit a doctor, as the exact diagnosis can be made there. The lower lip fistula is a typical symptom of Van der Woud syndrome.
The openings of the fistulas open into the red of the lips, near the transition from the skin to the mucous membrane. These fistulas can affect not only the aesthetics, but also the function of the lip. The cause is suspected to be a gene mutation that prevents the primary or secondary palate from closing in the course of embryonic development.
Fistulas in the mouth in children
Not only adults can suffer from oral fistulas, but also children who still have their milk teeth.
Fistulas can appear anywhere in the body, but are most commonly found in the mouth. If a fistula is found on the tooth, a visit to a dentist is also advisable, as milk teeth are not protected from tooth decay and inflammation in the root area is possible. The milk teeth fulfill an important placeholder function for the later permanent teeth, so that a milk tooth should be preserved for as long as possible until the permanent teeth erupt.
There are also a lot of different home remedies in circulation that are supposed to fight the fistula, but their development is usually associated with a larger problem so that only the dentist can tell the exact circumstances, especially in children. The cause should be investigated professionally. It is advisable to check the children's daily oral hygiene routine to ensure that it is being followed correctly. You can also look into the mouth from time to time to detect possible changes, since changes in the oral mucosa, especially in smaller children, are not noticeable.
prophylaxis
Dental fistulas can be avoided, as their original trigger is usually bacteria that eat their way through the tooth as caries and eventually attack the root, causing the inflammation.
Adequate and correct dental care is therefore the best prophylactic agent. The bacteria are fought by daily cleaning (at least twice a day). Dental floss, mouthwashes and tongue scrapers can also be used. Furthermore, a regular check-up by the dentist is advisable, who will assess the general condition of the teeth and can detect any existing inflammation very early. Most patients hardly notice the fistula entrances themselves due to their small size, so that the dentist can already examine and treat an early stage radiologically.
More on this topic: Proper dental care
Summary
Fistulas are more common in the oral cavity and are usually associated with severe pain that is not caused by the fistula itself but by the cause of the fistula. You should be careful with fistulas, not treat them yourself and go straight to the dentist, as there may be a possible focus of inflammation that attacks the teeth and the tooth supporting structure and should be treated as soon as possible.













.jpg)