Spinal cord
Synonyms
Spinal nerves, spinal nerves
Medical: Medulla spinalis (medulla = Latin marrow, spinal = Latin thorny, thorn-like, belonging to the backbone or spinal cord), myelon (= Greek marrow),
English: spinal cord
definition
The spinal cord is the lower part of the central nervous system (CNS), which runs within the spinal canal and is responsible for the motor (movements) and sensory (sensations) supply of the trunk, the extremities (arms and legs) and also the neck; so it connects the brain with the peripheral nervous system.
This is accomplished by 31 pairs of segmentally arranged spinal nerves (spinal cord nerves). The spinal cord membranes (meninges) and the cerebrospinal fluid filled with nerve fluid surround the spinal cord and flow smoothly into the membranes and cerebrospinal fluid spaces of the brain.

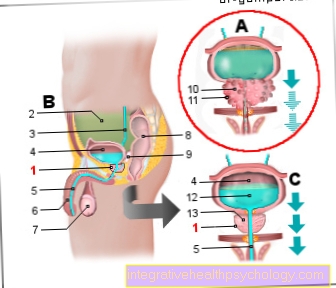
Figure spinal cord

1st + 2nd spinal cord -
Medulla spinalis
- Gray matter of the spinal cord -
Substantia grisea - White spinal cord substance -
Substantia alba - Anterior root - Radix anterior
- Back root - Radix posterior
- Spinal ganglion -
Ganglion sensorium - Spinal nerve - N. spinalis
- Periosteum - Periosteum
- Epidural space -
Epidural space - Hard spinal cord skin -
Dura mater spinalis - Subdural gap -
Subdural space - Cobweb skin -
Arachnoid mater spinalis - Cerebral water space -
Subarachnoid space - Spinous process -
Spinous process - Vertebral bodies -
Vertebral foramen - Transverse process -
Costiform process - Transverse process hole -
Foramen transversarium
You can find an overview of all Dr-Gumpert images at: medical illustrations
Location of the spinal cord
Upwards (cranial, = towards the skull), the spinal cord passes over the elongated medulla (medulla oblongata) directly into the brain as the upper part of the central nervous system (so that it can be viewed anatomically as an "extension of the brain") namely between the large occipital opening (foramen occipitale magnum) as the lower skull exit, and the uppermost cervical vertebra (atlas), where the bony skull merges into the spine.
From here the spinal cord continues through the entire spinal canal to the level of the 1st or 2nd lumbar vertebra. In adults it reaches a length of about 45 cm with a diameter of 10-14 mm. The spinal cord ends in the so-called conus medullaris, which in turn merges into a thin end thread (filum terminale). Below the 2nd lumbar vertebra there are only bundles of nerve fibers (the lower spinal nerves); these are called cauda equina (horse's tail).
The membranes of the spinal cord with the nerve water continue a little deeper into the so-called dural sac (from Latin dura mater = hard meninges), which is why one can easily take nerve water (liquor) at this point without fear of injuring the spinal cord . (Since this area is the lumbar, i.e. lumbar vertebra, the nerve fluid collection is referred to as a lumbar puncture. This is usually performed at the level of the 3rd / 4th lumbar vertebra).
Nerve water (liquor) is taken for CSF diagnostics to detect diseases of the nerve water or the brain.
Further information is also available under our topic: CSF diagnostics.
The so-called spinal anesthesia (spinal cord injection) is also performed at this height.
The spinal cord is fastened and suspended in the spinal canal, apart from by the laterally branching pairs of spinal nerves on the right and left of the so-called "toothed ligaments", the ligamenta denticulata. For a precise anatomical description including the membranes of the spinal cord, see also the contents of the vertebral canal (topic follows).
structure
The spinal cord is a symmetrical (= bilateral) reflex organ divided into two halves of the same kind and, in contrast to the brain, has a relatively original and simple structure that basically looks the same in its various sections. Analogous to Spine it can be divided into that
- Neck or cervical medulla (at the level of the 1st to 7th cervical vertebrae)
- Thoracic or thoracic medulla (at the level of the 1st-12th thoracic vertebrae)
- Lumbar or lumbar cord (at the level of the 1st-5th lumbar vertebra)
- Cross or sacral medulla (at the level of the Sacrum)
A rump or coccygeal medulla still present in other vertebrates is rudimentary in humans, i.e. only the non-functioning system is left.
From the spinal cord, pairs of nerve roots extend symmetrically on the left and right, the Spinal nerves (Nervi spinales). These pull evenly through the on each side Intervertebral foramen (foramen intervertebralis), which are formed by two vertebrae lying one above the other on the right and left of the vertebral bodies. In this short section they will Spinal nerve roots (Radix spinalis) because they can still be distinguished from a front (motor = for the muscles) and a rear one (sensitive = for the feeling) Share exist.
Figure spine and spinal cord

- Transverse process
- outgoing nerve (spinal nerve)
- Vertebral bodies
- Spinous process
- Spinal cord
Only after leaving the intervertebral holes do the two parts of the root unite to form the actual spinal nerve, which pulls into the periphery of the body.
This means that the spinal root is both the control center for two fundamentally different qualities as well as for two different directions of conduction: felt input from the outside is directed from the periphery to the central unit (spinal cord and brain) - and at the same time movement requests from the central unit to the muscles, to the periphery .
The two qualities (motor and sensory parts) naturally remain in the nerve, they are simply no longer distinguishable from one another and run as a common "cable".
Since they are electrically isolated by the fatty nerve sheaths (myelin sheaths), they do not get in each other's way.
Situation development
In infants the spinal cord fills the spinal canal up to the lower lumbar vertebrae, in children it extends to the 4th lumbar vertebra. This must be taken into account when withdrawing nerve water; you then have to go further down the spinal canal in order not to endanger the spinal cord.
In the following years of life, the spinal cord moves further and further upwards, as it is "attached" to the brain, but grows more slowly than the spine. This "ascent" of the spinal cord is medically called Ascensus medullae spinalis.
Originally during embryonic development, a nerve segment is opposite the associated vertebra. The spinal nerves are therefore forced to grow with the bony structures; therefore they have to descend more and more steeply with increasing age: their course in the vertebral canal becomes steeper and more oblique downwards.
In adults, therefore, the height of the spinal cord segment roughly coincides only in the upper cervical cord with the exit point of the associated pair of nerves. The spinal nerves originating in the lower parts of the spinal cord are compressed by "pulling up" the spinal cord to form the cauda equina, the horse's tail. This development process is completed by the age of 12.
Feinbau
The solid spinal cord shows a deep incision on its front (ventral or anterior), the fissura mediana ventralis / anterior, in which the anterior spinal artery (A. spinalis anterior) runs, and on its back (dorsal or posterior) a shallower groove, the so-called sulcus medianus dorsalis / posterior.
This furrow continues towards the inside into a fine septum, a so-called septum (septum medianum dorsale). The anterior incision and the posterior septum divide the spinal cord into two mirror-image halves.
If one looks at a cross-section of the spinal cord, then with the naked eye (= macroscopic) the inner, butterfly-shaped one is visible gray matter to recognize, which are clearly each in a front and a rear "horn" structured.
From it one can see the fibrous surrounding it white matter (Substantia alba) delimit the outside. The expression of this butterfly figure is different depending on the location. Both at the level of the chest and at the level of the lumbar section of the spinal cord, there is a small lateral horn between the two in the gray matter on each side, apart from the anterior and posterior horns.
In the middle runs the Central canal (canalis centralis), only visible as a tiny hole in cross section; it is filled with nerve water and represents the internal liquor space of the spinal cord.
When looking at a longitudinal section, you can also see that the spinal cord is thicker in these areas than in the rest of the course, as this is where the nerve roots emerge, which have to supply the arms and legs - so more nerve fibers and more nerve cell bodies are necessary here.
These thickenings are also called Intumescences (Intumescentia cervicalis in the cervical marrow or lumbosacralis in the lumbar area).
The Front horn (Cornu anterius) the gray matter of the spinal cord is broad and contains Nerve cell bodies, their Processes (axons) pull towards the muscles (so-called. Motor neurons).
They thus form the origin of the front, motor (thus serving the movement) Part of the spinal nerve root, which pulls out laterally from the spinal cord.
The Back horn on the other hand is long and narrow and forms the entry point for the rear, sensitive part of the spinal nerve rootsthat convey "felt" information generated in the periphery up to the brain (e.g. pain, temperature, sense of touch). Their nerve cell bodies, however, are located in the so-called spinal ganglion, which is located outside the spinal cord (but still in the spinal canal).
Nevertheless, there are cell bodies in the dorsal horn, namely those of the long front and side strands of the white matter, the so-called. Strand cells (see below)
The Side horn contains vegetative nerve cells (Neurons) of the sympatheticus (in the thoracic and lumbar marrow) and des Parasympathetic (in the sacral cord).
These "horns" are only shown in cross-section as "horns" ("butterfly wings"); they can be found - in different forms - throughout the spinal cord, regardless of where it is cross-cut. Therefore, viewed three-dimensionally, they are actually columns, and they are also referred to as columns or strips (Columnae). The Vorderhorn column is therefore called Anterior Columnawho have favourited Hinterhorn pillar Columna posterior and the side horn column Lateral Colum.
These “pillars”, in turn, should not be imagined as strands of equal strength everywhere that are connected from top to bottom whole Pull the spinal cord through, because they actually consist of juxtaposed Cell groups, mostly five.
These cell groups form short Columns that can extend over several segments, i.e. levels of the spinal cord.
They are also called core areas (kernels = nuclei). The cells of such a cell group are then each time for one Muscle responsible. If z. For example, if a group of cells extends over three segments, their processes (axons) leave the spinal cord through three anterior roots.
After they have stepped out, they later encamp one Put your nerves together that too one Muscle pulls. This is then called a peripheral nerves.
If a peripheral nerve is damaged, one will develop peripheral paralysis, It means that a muscle all fails.
If, on the other hand, a nerve root is damaged, one develops radicular paralysis (Radix = root), i.e. it fall Parts different Muscles off. (see also Root syndrome).
In the area of the arms and legs, the exiting spinal nerves assemble into nerve plexuses, the so-called. Plexus.
The area of skin that is supplied by the nerve fibers of a segment is called Dermatome.
The muscle fibers that are supplied by the nerve fibers of a segment are called accordingly Myotome.
It is important to remember that it is not one segment that supplies a muscle, but rather “different muscles may each supply a little”.
Finally, nerve fibers that connect the two symmetrical halves of the spinal cord with each other (commissure fibers) run directly around the central canal; Commissura grisea) so that half of the spinal cord knows what the other is doing.
This comparison is necessary for equilibrium processes and others. They also belong to the so-called self-apparatus of the spinal cord. This consists of nerve cells and their fibers that only communicate with each other within the spinal cord and enable processes that can take place without using the central circuitry via the brain; this includes e.g. the reflexes of the spinal cord.
Spinal cord disorders
Basically, it has to be said that the pattern of failures that occurs depends on exactly where the damage is in the spinal cord.
Even without diagnostic imaging like that CT (Computed tomography) or that MRI (Magnetic resonance imaging) one can already make very directional statements in this regard on the basis of the clinical picture due to the individual supply areas of the individual segments.
Common spinal cord disorders
- Developmental disorders of the spinal cord:
- Spina bifida ("open back")
- Syringomyelia
- Injuries:
- Paraplegic syndrome
- Whiplash trauma
- disc prolapse
- Spinal canal stenosis
- Anterior spinal syndrome (obstruction of the anterior spinal artery)
- Tumors in the spinal cord
- Poliomyelitis (polio)
disc prolapse
In the case of a herniated disc, the gelatinous mass of the disc emerges. This gelatinous mass can protrude into the spinal canal and press the spinal cord.
If the pressure becomes too great, it can lead to pain, sensory disturbances, paralysis and complete loss of function.
For more information on this topic, visit: Herniated Disc.
Whiplash trauma
In the case of whiplash injuries, sudden and unexpected violence on the head often results in damage to the cervical spine and the surrounding muscles.
By “throwing the head” the neck muscles try to catch the head, but are overwhelmed by the force due to the force.
Further information on this topic is available at:
- Whiplash trauma
- Cervical spine syndrome
Brown Sequard Syndrome
The most impressive example of the complexity of a pattern of failures is half-sided damage to the spinal cord with the interruption of the conduction of one half of the spinal cord in a segment, the so-called. Brown-Séquard syndrome, also known as "dissociated sensory disorder".