Physiotherapeutic treatment of spinal instability
Back pain
General medical information on the cause, diagnosis and treatment of back pain can be found at Back pain.
introduction
Back pain have become the number one widespread disease and a significant cost generator for the health system and the economy in Germany. The total costs for the care of chronic back pain are approx. 20 billion euros / yearwhere the majority of the costs are caused by sick leave.
The average costs per patient are around 1200 euros, of which the direct (medical) costs account for 54%, the indirect costs (caused by sick leave and production losses) account for 46% of the total. Back pain causes approx. 15 % of all sick leave / year and are the reason for 18% all early retirement.
About 60% of all adult men and women report back pain (regardless of severity and duration) within the last 12 months, and chronic back pain (this means back pain that lasts for at least 3 months and longer and occurs almost daily) within one year about 20% of all adults, based on the entire lifetime that is about 30% of all adults. Overall, women are more affected in terms of frequency and intensity.
While back pain used to be more of a problem for older people, those affected are now younger and younger and the need to have therapeutic options at hand to avoid recurrence (recurrence of symptoms) and chronification is increasing.
The main goal In the treatment of back pain, therefore, there is not only a temporary improvement in symptoms, but rather because of the tendency to relapse and become chronic long-term therapeutic success and avoidance of recurrence.
There are many causes for the development of back pain, although it is not always possible to determine a clear cause despite the most modern diagnostic options. For the development of back pain and the tendency to become chronic, in addition to physical factors, there are many accompanying circumstances such as Workload, social class, and cognitive assessment of pain depressive mood significant,
In the following topic I would like to refer to the Spinal instability caused by weakness in the local (deep) muscle system as a possible cause of high recurrence rates.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Figure spine

- First cervical vertebra (carrier) -
Atlas - Second cervical vertebra (turner) -
Axis - Seventh cervical vertebra -
Vertebra prominent - First thoracic vertebra -
Vertebra thoracica I - Twelfth thoracic vertebra -
Vertebra thoracica XII - First lumbar vertebra -
Vertebra lumbalis I - Fifth lumbar vertebra -
Vertebra lumbalis V - Lumbar cruciate ligament kink -
Promontory - Sacrum - Sacrum
- Tailbone - Os coccygis
I - cervical spine (red)
II - thoracic spine (green)
III - lumbar spine (blue)
You can find an overview of all Dr-Gumpert images at: medical illustrations
Stabilizing system of the spine
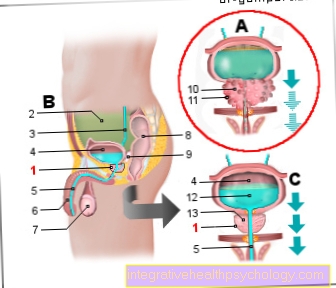
The stabilizing system of the spine consists of three parts, which can only guarantee optimal movement control of the spine in posture and movement when fully functional and in cooperation.
1st and 2nd part: active movement system = muscles, consisting of the global and local muscle system.
- The global muscle system consists of long, more superficial muscles that have a primarily moving function. You are able to move the spine and limb joints quickly and with great force and are responsible for controlling your balance. The muscle fibers of the global muscles are dependent on intensive blood circulation for their work and therefore tire quickly with prolonged holding work.
- The local muscle system consists of small muscles lying deep and close to the joints of the spine, which predominantly have a stabilizing function. They are responsible for our upright posture and work with little effort because they are in constant use all day. The local muscles ensure that the small vertebral joints always remain in a certain position, even with intense movement, fall or impact, they prevent this Malfunctions (painful movement restrictions, "blockages") of the spine and relieve the passive support system of the back.
- Part: passive support system, consisting of the bony components of the spine, capsule and ligamentous apparatus, the intervertebral discs, and the central (the part of the nervous system located in the skull and spinal canal) and peripheral (consisting of the cranial and spinal nerves) nervous system.
More information can be found here: The ligaments of the spine
Complicated control and management systems in our nervous system ensure that both muscle systems are activated at the right time and in the right order when they are posture and move. Thus, our body is able not to lose stability at the same time with optimal execution of movement sequences. Movement execution can be planned in advance and adapted after the movement has been completed for further perfection.
Stability = movement control
Only at optimal function and coordination (Cooperation) the moving and holding muscles, control via the nervous system and the intact passive structures painless movement is possible. In many studies it could be determined that back pain patients with poor motor control (coordination of all factors involved) have a high relapse rate.
Every severe acute pain of the back, regardless of the cause, a herniated disc or a slipping vertebra always lead to one Weakening of the deep muscle system.
This system is also always disturbed after a pregnancy has ended. Therefore, the training program for the local muscles is definitely recommended for women after childbirth, regardless of existing back pain.
Spinal instability
Symptoms of instability:
- the patient describes sudden shooting pain in the lumbar or cervical spine when moving e.g. when bending over or turning the head quickly
- the feeling that the back is breaking through or the head is not supported by the neck
- Pain and stiffness after getting up from the prone position or after long periods of sitting in the car and desk work
- Pain and stiffness in the morning after getting up
- Pain after strenuous activities such as carrying weights for a long time (e.g. when shopping)
- frequently recurring (recurrent) attacks of pain
However, these symptoms can also occur due to other causes. However, they give the doctor or physiotherapist possible tips on how to steer further diagnostics in certain directions.
Clinical examination
- When coming up from a stooped position, the patient is not able to get up again with straight legs, but has to bend his knees and support himself with his hands on his thighs
- the therapist feels the depth Musculature directly on the spine in the prone position or the deep ones Abdominal muscle in the supine position and tests the ability to tense
- Reduced flexion in the lumbar spine and compensatory increased mobility in the lower thoracic spine
- When testing the play of movement of individual vertebrae, the patient feels the pain that is typical for him and the therapist (possibly also the patient) feels too much freedom of movement compared to other vertebrae;
- when the patient is on the test Back muscles tense, the pain subsides
- other possible causes of the back pain must be ruled out, as mechanical dysfunctions or structural changes to the spine (e.g. herniated disc, Vortex sliding) occur in parallel
- in the MRI (imaging method) a reduced muscle cross-section of the local muscles is visible, this often remains even after the acute pain situation has subsided
- in the Electromyography reduced activities of the deep muscles can be measured
- In operations on the open spine (e.g. intervertebral disc operation) in the lumbar or cervical spine, the surgeon can see the reduced muscle cross-section of the deep muscles
Therapy goals
The prerequisite for starting the training is the elimination of accompanying possible causes of pain, such as mechanical dysfunction.
Short-range goals
- Learning to activate the deep muscles through perception training
- Improvement of the strength endurance of the deep muscles
- Integration of both (global and local) muscle systems, activity without loss of stability
- Automatic transfer of the correct muscle activity in everyday situations
Long-term goals
- Improvement of the spinal column stability and reduction of the back, neck or headache caused by instability in relation to pain duration and intensity
- Reducing relapse rates and preventing chronification
It is an arduous and absolute path for the patient to achieve the last two therapy goals Compliance (Motivation and cooperation). 3 months of intense everyday To practice are required to have improved basic stability and lasting Pain reduction after that, in most cases the training units can be reduced. However, after initial learning, many individual exercises can be carried out in the supine, lateral or quadruped position in an upright posture such as sitting or standing. Therefore, the exercise units can be integrated very well into everyday life.
In order to make it easier for the patient to improve motor control, complex exercises are taught in individual steps and, after learning individual tensions (can take up to 4-6 weeks), 2 combined exercises (cervical flexors / extensors, shoulders / abdomen, back, pelvic floor) or can be merged into a total body tension, which significantly reduces the daily exercise time.
If the patient is able to maintain the basic body tension correctly, additional movement sequences (activity of the global locomotor muscles) are added.
In the last step, the learned tension and movement sequences are integrated into everyday life for the purpose of automation. Everyday situations that cause difficulties for the patient are preferably trained.
Important NOTE
The training must not cause the patient's typical pain.
On the part of the physiotherapist, a good methodology and the ability to convey perception exercises clearly are required. Especially at the beginning of the training, the therapist has to give a lot of support through easy-to-use exercise instructions and tactile help and feedback via his hands.
The physiotherapist can use a biofeedback device, a pressure meter for muscle tension or an ultrasound device as additional control and feedback for the patient.