Stem cell transplant
definition
A Stem cell transplant denotes the Transfer of stem cells from a donor to a recipient. Stem cells are body cells that have the origin for the development of other cells. They have the ability to differentiate into, for example, muscle, nerve and blood cells.

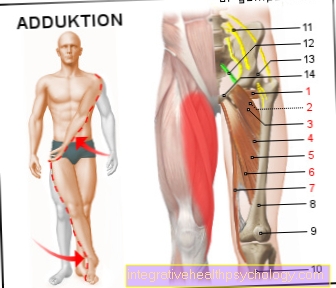
Mature stem cells are found in more than 20 organs in our body. They perform the special task of forming replacement cells and develop into a certain type of tissue.
In everyday clinical practice, mature stem cells are usually obtained with the help of a Bone marrow aspiration obtained from the pelvic bone. Blood stem cell transplantation is of the utmost importance today.
Allogeneic stem cell transplant
An allogeneic stem cell transplant is defined as the transfer of stem cells between two different people.
The recipient receives the stem cells from a suitable donor. The transplant is preceded by a so-called conditioning phase. On the one hand it serves the Suppression of an immune response of the recipient against the transplanted cells and on the other hand destroys the malignant, functionless cells. For this purpose a high-dose chemotherapy alone or in combination with a radiotherapy used.
Autologous stem cell transplant
At a autologous stem cell transplant are Recipient and donor the same person. The Stem cells be the patient removed and stored. The transplant takes place later and also after a so-called conditioning phase. As a result of chemotherapy and / or radiation therapy treatment, the bone marrow and its cells are destroyed and replaced during the transplant.
The therapy efficiency is significantly increased compared to chemotherapy or radiation therapy alone.
Stem cell donation
If a suitable donor with similar characteristics to the recipient is found in the German donor register, the donor is examined in detail about one month in advance.
There are two ways of collecting stem cells.
The stem cells are either from the Bone marrow or from the Blood drawn.
The Withdrawal from the blood by means of Stem cell apheresis The most common method for obtaining stem cells is through a vein. It is carried out on an outpatient basis and takes between four and five hours. A few days before the stem cell separation, the Dispenser of a drugwhich causes the stem cells to pass into the blood. Stem cell apheresis takes place in specialized centers. The venous blood goes into a separator that filters out the stem cells and directs the blood back to the body.
A method that is carried out much less frequently is Bone marrow puncture of the iliac crest. The Bone marrow donation is under general anesthetic carried out. Between 0.5 and 1.5 liters of bone marrow are removed from the donor via a needle. The puncture takes about an hour. Since the procedure can be associated with a greater loss of blood, the donor is given an autologous blood donation at the same time as the withdrawal.
Stem cell transplant process
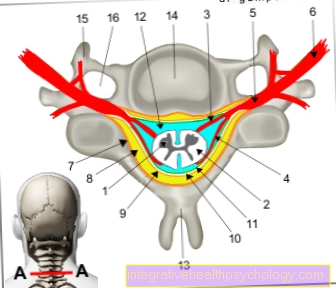
The stem cell transplant from the recipient's point of view begins with what is known as conditioning. It is a Preparatory phase, the the Destruction of malignant cells serves in the bone marrow and with a Suppression of the body's immune system goes hand in hand. Come for this purpose Chemotherapy and radiation therapy such as Antibody therapies that can be combined in different ways.
The stronger the dosage of the treatment is chosen, the more pronounced the side effects the patient will experience. At the same time, however, the probability of a relapse, i.e. a relapse, is reduced. In the best case scenario, all diseased cells are destroyed. The treating physicians decide individually on the exact procedure.
The transplanted cells have their own immune cells that destroy the recipient's remaining bone marrow cells after the transplant. Identical twin pairs tolerate each other's stem cells almost without any problems, but in this case the immune response of the new immune system to the diseased cells is also rather low. Malignant cells can persist for this reason.
Similar to a blood transfusion, the patient receives the healthy stem cells or the bone marrow im Following the conditioning through a vein. The transplanted blood stem cells settle in the medullary cavities of the bones and form functional blood cells. Within three weeks the blood values normalize and the process of bone marrow growth is complete.
Conditioning
Under Conditioning one understands the preceding stem cell transplant Destruction of the bone marrow through chemotherapy or radiation therapy measures. In this way, malignant cells are destroyed. In the best case one succeeds Destruction of all cancer cellsso that the chance of recovery increases.
Besides, that will immune system Recipient inoperable made. This plays an important role in allogeneic transplantation, as the rejection of the donor cells is to be prevented.
Stem cell transplant for leukemia
Under leukemia one understands one Group of diseases of the hematopoietic system, in which malignant subgroups of white blood cells multiply in an uncontrolled manner.
The Treatment of leukemia is based on one chemotherapy and / or radiotherapy destruction of the malignant and functionless cells in the blood as well as in the bone marrow.
In particular acute leukemiaThose that progress quickly can be combated well in this way and in some cases even cured entirely. In other cases, this form of treatment is less promising. This is especially true for that chronic forms of leukemiathat progress more slowly and over a longer period of time. They are more likely to show resistance to radiation or chemotherapy alone. The disease can be controlled temporarily, but it has a high likelihood of relapses.
In such cases, as well as in patients with other forms of leukemia that are difficult to treat, there is Possibility of conditioning with subsequent stem cell transplant. First, the sick, but also some healthy cells of the recipient are destroyed before the healthy stem cells are transfused.
Complications and Risks of a Stem Cell Transplant
Stem cell transplantation is not risk-free and can be associated with possible complications. Regardless of autologous or allogeneic transplantation, there is a low probability that the donated cells will not grow in the medullary cavity of the bone.
One complication of allogeneic stem cell transplantation is the so-called "graft versus host disease" (GvHD). The immune cells of the donated transplant are directed against the cells of the recipient and destroy them. Such an immune reaction can occur acutely or with a delay. The organs most commonly affected by destruction are the skin, liver and intestines. The consequences can be life-threatening for the patient. The risk of GvHD is different in each case. The attending physician explains the individual risk. So-called immunosuppressants are supposed to reduce the risk of GVHD after the transplant. They reduce the immune reaction and are associated with an increased risk of infection.
There is no such complication with autologous stem cell transplantation because the immune system of the donor and recipient is the same. Possible complications in this case result in particular from the temporary pancytopenia, the lack of all blood cells. The time between transplantation and full bone marrow recovery is between one and three weeks. During this time, the patient is particularly at risk from infections with bacteria, viruses and parasites. The same applies to allogeneic transplantation.
Another possible complication of allogeneic stem cell transplantation is occlusion of the hepatic vein. At the same time, swelling of the organ and a significant increase in liver-specific laboratory values are observed. However, in most cases it is a reversible process.
Other complications of both autologous and allogeneic stem cell transplants are the side effects of the previous treatment, chemotherapy or radiation therapy. The gastrointestinal tract is particularly affected. The therapies destroy the mucous membrane cells and can cause inflammatory changes. Patients often complain of painful inflammation in the mouth area. The mucous membrane in the urinary system is also destroyed. Other organs that are affected are the liver and lungs.
Long-term complications of high-dose radiation and chemotherapy are infertility in both sexes and a possible clouding of the lens (cataracts) after whole-body radiation.
Read more on the topic Chemotherapy side effects
As part of the stem cell transplant, HLA is also determined in order to avoid rejection by the recipient. For detailed information, read the following article: HLA - Human Leukocyte Antigen
Stem cell transplant survival rate
The Survival rates after a allogeneic or autologous stem cell transplantation have risen continuously in recent years. This is due to increasingly safe transplants and a decrease in transplant-associated mortality. The Survival rate depends however from many factors from.
Stage of the disease and Disease form, Age and constitution, as well as the Degree of correspondence between recipient and donor cells in allogeneic transplantation play an important role.
Within the first year after an allogeneic stem cell transplant, the risk of dying or relapse is highest.
Among the most common Complications and possible causes of death include the "graft versus host disease", infections and damage to organs. If the percentage risk is around 80% in the first year, it drops to around 50% in the following five years. For autologous stem cell transplants, a relapse in the first year after the procedure is associated with a poorer prognosis.
In 2014, the survival rates were published for the first time by the German Register for Stem Cell Transplants (DRST). From cure one speaks when the Recipient is disease free five years after the procedure.
A cure was found in about 50% of patients with an allogeneic stem cell transplant acute myeloid leukemia (AML) achieved. In other words, the 5-year survival rate was 50%. For some other forms of leukemia, the 5-year survival rate after allogeneic transplantation was around 40%.
The 8-year survival rate after autologous stem cell transplantation is around 50%. In the case of multiple myeloma, a cure can be achieved in around half of the cases.
Stem cell transplant costs
The costs for one Stem cell transplant are from the Health insurance of the recipient. This also applies to all examinations, hospital stays and the resulting loss of work of the respective donor. The billing of the health insurance is regulated by the German bone marrow donor database, DKMS for short.
At the preceded Initial typing and the Inclusion of the donor in a donor register, there are also costs. However, these are not paid for by the health insurance companies, but primarily from donations financed. The German bone marrow donor register is financed on the one hand through donations and on the other hand through reimbursement of costs from the health insurance companies. These provide reimbursements for laboratory tests, the removal of stem cells and their process and organization, among other things. The cost of registering in the donor database is 50 euros.
The total cost for a stem cell transplant in Germany amount to around 100,000 euros.