What are the signs of pneumonia?
introduction

Pneumonia is an inflammatory disease of the respiratory system - the lungs. This disease, which is the scientific name pneumonia is mostly caused by pathogens of all kinds - bacteria, viruses, Mushrooms and other harmful organisms. In some cases, it can also cause lung tissue poisoning inhalation (inhalation) of toxic substances or gases cause inflammation. Also play immunological processes a role, i.e. processes in which the immune system is directed against the body's own cells. However, infections are in principle more relevant as a cause.
Pneumonia is that most common infectious disease in the world. In Germany alone, 300,000 people are affected by this disease every year. In the meantime, good therapeutic approaches have been developed and the death rate from pneumonia is no longer high. However, this only applies to immunocompetent people, i.e. people with an intact immune system. Is this weakened, can a pneumonia the General condition of the patient greatly deteriorate and even lead to death.
The signs of pneumonia are strongly related to the cause of the disease. The course of the disease can vary depending on the pathogen. The place where the pneumonia developed also plays a role. A distinction is made between one outpatient (outside the hospital) acquired pneumonia (CAP: community-acquired pneumonia) and one nosocomial (during the hospital stay) Infection (HAP: hospital-acquired pneumonia). In principle, one can say that HAP has a worse prognosis than CAP, because mostly patients who develop pneumonia in addition to their actual condition are immunocompromised (immunosuppressed).
Signs (symptoms) of pneumonia
Bacterial pneumonia, such as that caused by the bacterium Streptococcus pneumoniae is triggered, has a relatively rapid course. It is also called lobar pneumonia (lobe = Lobes) because the inflammation is limited to one or more lobes. As soon as the mass of pathogens has overwhelmed the patient's immune system, blood flow to the lung tissue increases and immune and blood cells as well as substances of the coagulation system are deposited. These form a alveolar exudate, a liquid secretion in the alveoli that catalyzes the inflammation. Within a few hours, the patient feels seriously ill. The temperature rises to 40 ° C and there is also chills. The one with the pneumonia Associated cough is dry at the beginning. This changes after 2-3 days - yellow to red-brown sputum appears. The inflammation continues to take its toll by affecting breathing and the heart. Difficulty breathing occurs even when you are completely at rest (Resting dyspnea) and the speed of breathing increases to compensate for the decreased oxygen uptake (Tachypnea). The cardiovascular system joins this compensation - the heart beats faster in order to provide better blood flow to the lungs (Tachycardia). The overall poor condition of the sick person can affect their consciousness. It has been observed that patients with severe pneumonia are confused and increasingly sleepy. The lungs are surrounded by a kind of envelope, the Pleura. It is fused on the one hand to the lungs and on the other hand to the chest. If the pneumonia spreads and there is a corresponding involvement of the pleura (pleurisy), then in addition to the general symptoms, people feel painful breathing.
Read more on the topic:
- Fever, dizziness and headache
- Pneumonia pain
While lobar pneumonia must be localized, there is one interstitial pneumonia a unlimited infection. The Interstitium is the tissue of the lungs. Interstitial pneumonia is mainly caused by Viruses but also some bacteria can be the cause of such a disease. In contrast to lobar pneumonia, however, the inflammation does not exist in the alveoli, i.e. in the lumen of the lungs, but in the tissue, in the interstitium. The immune cells absorb the pathogens and then wind into the tissue, where the inflammatory processes then take place. Because the lung function is not initially restricted, interstitial pneumonia arises rather creeping there is one Infection without a fever or just one slight temperature increase (Fever is always a sign of bacterial infection!), slight cough with no sputum, but still increasing problems with breathing. Depending on the pathogen, general symptoms of an infection appear: feeling sick, headache and body aches, pain in the throat and chest.
Both of the last-described types of pneumonia are mostly acquired on an outpatient basis. In the case of HAP, i.e. a hospital infection, the clinical picture can be more complicated. As mentioned earlier, are more likely immunocompromised Patients affected by hospital-acquired pneumonia. That means that to the serious underlying disease, another severe inflammation occurs that may not even be recognized as such. Affected patients are often so limited in their condition that they need ventilation. Since they are not conscious, they cannot report any complaints. The responsibility now rests with the medical and nursing staff. New fever and changes in the blood count, such as in the Inflammation parameters, can provide information about pneumonia. The oxygen content in the arterial blood should also be monitored in order to detect any loss of function of the lungs.
Risk factors for pneumonia

Various factors can increase your risk of developing pneumonia. In many cases, this results in secondary pneumonia. This means that the inflammation can be seen as a result of another underlying disease. The risk factor "old age" must be differentiated from this: both people of old age and small children fall ill more quickly than people in other age groups.
-
Lung diseases: If there is already a disease of the lungs, the risk of an inflammation is logically increased. The classic diseases include the following: COPD (Chronic Obstructive Lung Disease) - a disease that largely affects smokers and restricts the lungs in various functions; Cystic fibrosis (MS) - an autoimmune disease; Bronchiectasis - an expansion of the bronchi; a pulmonary emphysema
-
- the end stage of many chronic lung diseases in which the lungs lose their elasticity. As a result of all the diseases mentioned, the lungs lose their vitality and the cells are increasingly damaged. This makes it easier for pathogens to settle.
Read more on the topic: End-stage COPD
-
Immunosuppression: If the immune defense is restricted, the body's defense against all pathogens and harmful external influences is weakened. The pathogens are not opposed and they can attack the body unhindered. Since the lungs are an optimal entry point - they are moist, warm and well supplied with blood - an infection can often be found here in immunosuppressed patients. The immune system can be switched off by various diseases, but also by treating other diseases. Such treatments are, for example, chemotherapy for cancer - the chemotherapeutic agent is designed to kill cancer cells, which inevitably also dies healthy cells - or drug immunosuppression, such as must be carried out after an organ transplant, in order to reduce the risk of it from the body is repelled.
Illnesses that limit the immune system are for example diabetes mellitus and alcoholism. Both are associated with an unhealthy lifestyle and a poor general condition, which negatively affects the immune system. However, these two clinical pictures represent conditions that can be influenced and that can be kept within limits with correct therapy. Cancer and an HIV infection cannot be influenced by the patient. In principle, an HIV infection can be prevented through sexual contraception and careful handling of blood, but once infected, there is no cure, based on current knowledge. The right medication can weaken the course and delay the deterioration of the condition for years. In the final stages, however, AIDS always occurs - that Acquired Immune Deficiency Syndrome (in German: "acquired immunodeficiency syndrome"). The HI viruses attack the immune system's defense cells and thereby destroy them. This opens the door to any infection and a mild cold can turn into serious pneumonia that is fatal.
- Other factors: Inhaling various substances can inflame the lung tissue. This also includes stomach acid or food particles. Tobacco smoking in general damages the lungs and can cause various chronic lung diseases is already known. The risk of developing pneumonia also increases when consuming tobacco products. The circumstances in which intensive care patients are in the hospital are also a risk for the lungs: bed rest (consistently shallow breathing) and intubated ventilation (the body's own immune system is bypassed) can promote pneumonia.
Also read our article: Incubation period of pneumonia
Affected patient groups
-
Pneumonia in babies: In newborns, pneumonia often takes the form of sepsis, that is, one Blood poisoning. The small body is taken by surprise by the massive occurrence of the pathogens, which means that the pathogens also get into the blood. Since the baby still has antibodies from the mother, which only disappear in the course of the next few weeks and months, the immune system is not completely defenseless. The pathogens in babies are mostly staphylococci, streptococci, and others gram negative bacteria such as E. coli and various strains of viruses. In addition to sepsis, there are other symptoms of pneumonia, such as coughing and difficulty breathing.
-
Pneumonia in toddlers: The symptoms can sometimes be difficult to combine into one clinical picture in toddlerhood. They are often unspecific, but usually have one thing in common - fever. Pneumonia should be ruled out with every appearance of unclear febrile conditions. But at this point there should be no panic: As a toddler, humans have built up antibodies against a wide variety of pathogens and the immune system is developing. Pneumonia is no longer as dangerous as it is with a baby. Overall, the pathogens are similar to those found in babies. In small children, however, there is also a critical bacterium: Haemophilus influenzae. In addition to pneumonia, it can colonize all other parts of the respiratory system and one too Meningitis (Meningitis).
For more information, see: Pneumonia in the child
-
Pneumonia in children: In childhood, especially when starting school, the body is again confronted with a wide variety of influences. The main symptoms of pneumonia in children apply here: coughing, difficult and fast breathing, noticeable onset of the auxiliary breathing muscles (strenuous lifting of the chest beyond normal breathing), pain and fever. Here, too, individual differences can occur. Depending on the pathogen, specific signs may be added to the main symptoms.
- Pneumonia in adults: The severity of pneumonia in adults can vary due to several factors. The state of health plays a major role in this. More on this under risk factors. The first signs are an initially dry cough and difficulty breathing. If this combination occurs, a doctor should be contacted to initiate treatment and support the immune system. All other symptoms can be found under signs.
Read more on this topic at: Pneumonia in old age
Diagnosis

Various examination methods can be used to determine pneumonia. However, several should always be combined in order to be able to make a clear diagnosis. In the Auscultation typical rustling noises can be heard in the lungs, i.e. when listening to the chest with a stethoscope. An experienced doctor can thus differentiate between different lung diseases and receives an indication of the location of the inflammation through auscultation. This knowledge can then be used in the examination with imaging methods.
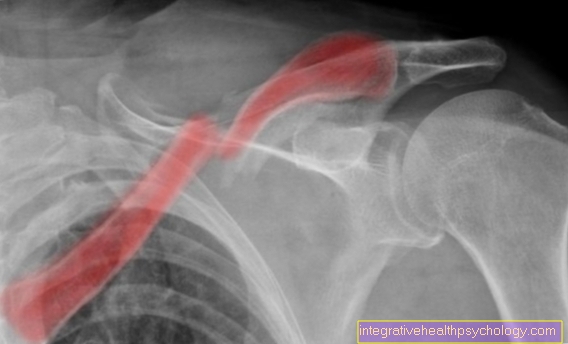
If pneumonia is suspected, an X-ray is usually taken first. If light spots or shades can be seen in the lungs on the image, these areas are poorly ventilated. This in turn means that fluid is pooling or has collected in the lungs - a sign of pneumonia. If anything is unclear or particularly difficult, a computer tomography (CT) be necessary. If the patient has painful breathing, pleurisy must be excluded. This can be done through an ultrasound scan. Laboratory diagnostics can be used to examine the blood as well as samples from the lung secretion or a biopsy (tissue sample taken by surgery). The inflammation parameters are checked and antibodies tested to identify the pathogen strain.
Find out all about the topic here: Diagnosis of pneumonia.
Therapy for pneumonia
Basically, antibiotic therapy is carried out. The drugs used are tailored to the age of the patient. Other antibiotics can be used for penicillin allergies, as some people have. It is treated as broadly as possible so that all common pathogens are affected. This enables therapy before the pathogen has even been identified. Cold compresses or antipyretic drugs such as paracetamol or ASA can help against the fever. The patient should stay mobile, do breathing exercises and drink enough to keep the body strong and to ventilate the lungs as well as possible, as well as to promote blood circulation. If the infection is caused by special pathogens, the medication must be adjusted to this and the use of substrates beyond the antibiotic group is necessary.
For more information, read on here: The therapy of pneumonia.