Female reproductive organ
Synonyms
Scabbard
engl .: vagina
definition
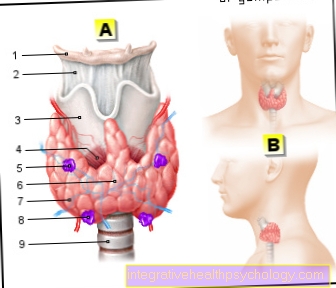
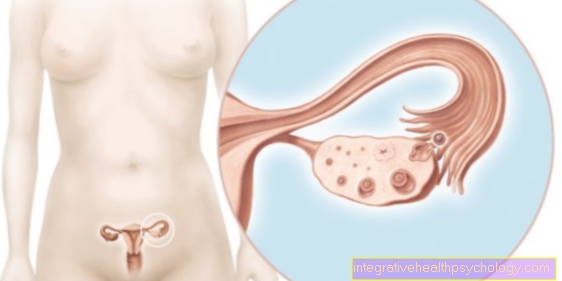
The vagina or sheath is one of the female sexual organs and is a thin-walled, approximately 6 to 10 cm long, stretchable tube made of connective tissue and muscles. The so-called portio, the end of the cervix (Cervix); its mouth is in the vaginal vestibule (Vestibulum vaginae, vestibule = Atrium).

anatomy
The vagina extends from the cervix (Cervix uteri, Cervix = Neck, uterus = uterus) to Ostium vaginae (Ostium = Mouth), which extends into the vaginal vestibule (Vestibulum vaginae, vestibule = Atrium).
The part of the vagina near the Cervix forms the vaginal vault (Fornix vaginae) with a front, a back and side parts. The posterior picks up the ejaculated sperm during sexual intercourse, which is why it is also known as the “semen container”.
As Vaginal introitus (Introitus = Entrance) is the name given to the vaginal entrance and is found at the ostium. This is closed by the hymen (Hymen = wedding god) or the remains of the hymen (Carunculae hymenales).
The walls of the vagina have different lengths, the front being about 2 cm shorter than the back, and are usually directly on top of each other, so that an H-shaped cross-section is created. This is furthest at the point of the vaginal vault and narrowest in the lower third of the vagina below the pelvic floor muscles (Levator gap).
Regarding the anatomical position, the urinary bladder and urethra are found on the front of the vagina, and the rectum on the back (rectum) and anal canal.
The vagina is connected to these surrounding structures by connective tissue septa. Between the bladder and vagina, this is known as Vesicovaginal septum (Vesica = Urinary bladder), between urethra and vagina as septum urethrovaginale (urethra = urethra). The rectovaginal septum is located on the back of the vagina to the rectum (rectum).
The inside of the vagina has several longitudinal and transverse folds, the longitudinal folds (Columnae rugarum; columna = Latin column-like organ, ruga = Latin skin fold) are raised by the venous plexus underneath. A particularly prominent elongated fold (Carina urethralis; carina = Spur, urethra = Urethra), on the other hand, is formed by the urethra lying behind it. The transverse folds in the vagina (Rugae vaginales; ruga = Latin skin fold) in turn usually disappear after the first birth of the woman.
The vagina is supplied with blood through several arteries, namely through branches of the Uterine artery (Artery of the uterus) and Arteria pudenda interna, on the other hand via the Arteria vesicalis inferior (Artery of the urinary bladder). The venous blood of the vagina is drained through a plexus of veins, the Vaginal venous plexus, into the great venous vessels (Internal iliac veins).
Responsible for the nerve supply to the vagina is on the one hand an autonomous nerve plexus, the uterovaginal plexus, and on the other hand an independent nerve, the Pudendal nerve.
The vagina is also connected to the lymphatic system. The lymphatic drainage passes through several lymph nodes (Nodi lymphatici), namely the internal pelvic lymph nodes (Nodi lymphatici iliaci interni) as well as the superficial lymph nodes of the groin (Nodi lymphatici inguinales superficiales).
Histology / tissue
The tissue of the mucous membrane of the vagina is divided into several layers from the inside out:
- Mucosa = multi-layered, uncornified squamous epithelium and connective tissue lamina propria, no glands
- Muscularis = smooth muscles, elastic fibers, connective tissue
- Adventitia / paracolpium = connective tissue; Anchoring in the area
The mucosa of the vagina, in turn, is divided into several layers, namely into a multi-layered, uncornified squamous epithelium and a connective tissue lamina propria (lamina = plate).
The squamous epithelium of the vagina consists of the following 4 layers:
- Stratum basale (stratum = cover): Basal cells, responsible for the multiplication of cells
- Stratum parabasale / Straum spinosum profundum: Parabasal cells, beginning differentiation of the cells
- Stratum intermedium / Stratum spinosum superficiale: Intermediate cells with a lot of glycogen
- Stratum superficiale: Superficial cells with a lot of glycogen
- Langerhans cells: cells of the immune defense, in between
This epithelium is subject to changes that are caused by hormones depending on the female cycle:
- Before ovulation or pre-ovulatory, all layers are strongly developed by the influence of estrogen.
- After ovulation or post-ovulatory, the superficial stratum is broken down, releasing the glycogen contained in the cells.
The mucous membrane of the vagina is kept moist in two ways: on the one hand, the cervical mucus moistens it, and on the other hand, the transudate, which is pressed out of the venous plexus of the vagina. The amount is 2 to 5ml on day, with sexual arousal up to 15ml can be formed.
The vagina is also colonized by bacteria, which creates the vaginal flora. The type and number of organisms that settle in the vagina depends on the glycogen content and thus on the hormone level, since the hormones regulate the release of glycogen from the superficial cells in the female cycle and during sexual maturation. Up to puberty, staphyloococci and streptococci predominate and the vagina is in an alkaline environment.
However, this changes with the onset of puberty and lasts until post menopause. Now, mainly lactic acid bacteria (lactobacilli) are found in the vagina, which break down the released glycogen into lactic acid (lactate), which makes the vaginal environment acidic (pH 3.8 to 4.5).
In addition to the germs mentioned, others can also occur.
function

The vagina itself has several functions. On the one hand, it serves to derive the Cervical secretions as well as menstrual blood (see also menstrual bleeding, on the other hand it is to a certain extent the reproductive organ during sexual intercourseCopulatory organ), during which time it expands due to its elasticity.
The vagina also acts as the last part of the birth canal when giving birth to a child. Here, too, vaginal elasticity plays a decisive role, as it enables adaptation to the baby's head circumference.
The vaginal flora also fulfills an important function in that, on the one hand, it kills pathogenic germs in the vagina through the acidic environment and, on the other hand, by protecting the colonization of the vagina with non-pathogenic germs as a “placeholder” from infections with pathogenic germs. This is to be understood in such a way that there is no settlement area for the pathogenic pathogens, as this is already occupied by the non-pathogenic organisms.
In this way, the flora of the vagina also offers protection against ascending diseases in higher organs such as the uterus or ovaries (germ ascension).
Investigations
There are diverse ones with regard to the vagina and its surrounding structures Investigation methods: The manual vaginal examination including colposcopy and smear, an examination of the Douglas room or a vaginoscopy.
Vaginoscopy is an inspection of the vagina with the help of an endoscope, which is an optical instrument ("Light hose") With a connected camera, which enables the" mirroring "of hollow organs. This procedure is used either in children or in women with a very narrow vaginal entrance (Introitus) or even intact hymen. Overall, however, this examination method is rarely used.
In contrast to this, the vaginal examination, which is carried out by the gynecologist for example (gynecologist) is carried out as part of cancer screening. Here the gynecologist adheres more or less to a fixed scheme; at the beginning there is the external assessment (inspection) pubic hair, skin, Vulva, clitoris, labia (Labia) as well as the vaginal entrance (Introitus) and the urethral outlet (Ostium urethrae). Furthermore, the patient should press once under the doctor's view to check whether urine is leaking (in Stress incontinence) or the uterus (uterus) comes to light (at Descensus or Prolapse).
This inspection is followed by an examination of the vagina using special instruments - specula. This allows the labia minora be carefully pushed aside to allow an assessment of the vaginal wall and the portio. The whole thing can be done as a simple colposcopy; that is, the vagina is viewed through a microscope (Colposcope) viewed with 6 to 40 times magnification. This method is called extended colposcopy if acetic acid or a certain solution (LugolSolution) is dabbed onto the portio to examine the cells for changes.
In addition, the gynecologist can use a spatula and a brush to take a swab from the portio and cervical canal during this procedure cytological examination to connect. This is also known as a PAP smear, which is used for the early detection of cancer of the cervix (where also Polyps may have occurred as a preliminary stage) (cervical carcinoma).
A pathogen smear can also be taken if necessary and if there is clinical suspicion.
At the end there is the bimanual vaginal palpation examinationThe gynecologist usually inserts two fingers of one hand into the vagina to check the position, shape, size and consistency of the vagina, portio, uterus, ovaries and surrounding structures. With the other hand he feels against it from the lower abdomen. If necessary, this is followed by a rectal examination.
Furthermore, an assessment of the deepest protrusion of the peritoneum, the Douglas space, via the vagina is possible. The doctor can use this space through the back of the vaginal vault (Fornix) palpate and puncture if necessary.
The smear of the vagina shows different findings depending on the point in time of the female cycle:
- In the proliferation phase / pre-ovulatory = many parabasal cells
- At the time of ovulation = many superficial cells
- In the secretion phase / postovulatory = many intermediate cells
- In children and postmenopausal = many parabasal cells
Diseases / anomalies
The vagina can be affected by various diseases. These include inflammation, injuries, cancer formation (Vaginal tumor) as well as a lowering (Descensus) or an incident (Prolapse) the vagina.
Inflammation of the vagina is known as vaginitis or colpitis; it is caused by bacteria, viruses or fungi. Typical symptoms are discharge, itching and burning pain. Pain when urinating or having sexual intercourse are also characteristic symptoms.
Vaginal fungus

Vaginal fungus, also known as vaginal mycosis, is one of the most common gynecological diseases. The most common pathogens are Candida, a special type of yeast fungus. Candida species are part of the normal flora and also occur in healthy people. Due to an imbalance in the vaginal flora, immune system weaknesses, hormones or a change in the pH value, these fungi can multiply and cause symptoms. People who are immunocompromised or weakened, such as chemotherapy patients, diabetics and pregnant women, are particularly at risk. Excessive personal hygiene, especially intimate hygiene and stress, can also promote the development of vaginal fungus. Usually, people report itching around the genitals and white discharge. Skin changes and discomfort when urinating can also occur. To fight vaginal mycosis; It is recommended to take suitable antimycotics in the form of tablets or ointments. In order to avoid the spread of the disease and reinfection, it is advisable to also treat the sexual partner. To prevent further fungal infestation, excessive intimate hygiene and non-breathable underwear (for example made of synthetic fibers) should be avoided.
Read more about this under Vaginal fungus.
Vaginal dryness
Vaginal dryness occurs when the vagina does not produce enough moisture. Typically, between two and five grams of discharge is produced per day. This discharge takes on various functions, including a protective function and friction protection during sexual intercourse. If the discharge is no longer sufficient and the vagina is dry, various symptoms such as itching, pain and burning sensation can occur. Vaginal dryness also makes you more susceptible to various bacterial and fungal infections. Vaginal dryness can be caused by hormones and particularly affect women going through menopause.
Read more about this under Vaginal dryness.
Pregnancies and various medications can also have an influence on the hormones and thus on the vaginal discharge. Since the secretion of the fluid depends on the vaginal blood flow, nerve and vascular diseases can cause vaginal dryness. Women who suffer from multiple sclerosis, diabetes mellitus or high blood pressure are particularly affected. Excessive alcohol and nicotine consumption also have a negative effect on blood vessels and can affect vaginal discharge as well. Vaginal dryness can also occur as a result of chemo or (anti) hormone therapy. Mental stress such as stress or anxiety as well as excessive intimate hygiene can also cause vaginal dryness. If vaginal dryness is suspected, a gynecologist should be visited. It is important to determine the cause in order to be able to initiate adequate therapy.
Itching in the vagina
An itchy vagina is often an indication of bacterial or parasite infection. Herpes simplex virus infections lead to genital herpes, which is characterized by burning and itchy blisters in the genital area. An infection with chlamydia can also lead to itching, although chlamydia infections are usually asymptomatic. Parasite infestation often leads to inflammation, which is accompanied by itching. Itching can also appear as a side effect of eczema. Fungal infections or hormonal disorders as well as vaginal dryness can also cause itching. Urinary tract infections can also cause similar symptoms. Lichen sclerosus et atrophicus vulvae mostly occurs after menopause and is characterized by degeneration of the skin and pronounced itching. This condition can lead to cancer. It is generally important to see a doctor to determine the exact cause of the itching and to initiate appropriate therapy. The cause of a prolonged itch should always be clarified, as it can also be a malignant disease.
Read more on the subject at: Itching in the vagina
Vaginal inflammation
Inflammation of the lining of the vagina is also called vaginitis. One speaks of vulvovaginitis from the moment the labia are pulled in pity. Inflammation of the vagina is in most cases the result of an infection by bacteria or parasites. Possible pathogens are anaerobes that lead to vaginosis, fungi such as the Candida species that lead to vaginal thrush, or infections caused by sexually transmitted pathogens such as trichomonads. Inflammation can also occur as a result of an allergy or as a reaction to a foreign object, but this is less common than infection. Women who suffer from vaginal infections often have reddening of the vagina, the labia and possibly the perineum. Other symptoms include an unpleasant intimate odor, increased discharge and pain when urinating or during sexual intercourse. If a vaginal infection is suspected, a gynecologist should be visited. After a detailed questioning and examination, the appropriate therapy can be initiated. The therapy depends on the origin of the inflammation, the pathogen and the resistance of the pathogen.For bacterial infections, antibiotics should be prescribed, for fungal infections, antifungal drugs should be prescribed.
Read more on the subject below Vaginal inflammation.
Vaginal cancer

Vaginal cancer is a rare malignant form of the female genital tract. The origin of this degeneration is not clear, but it is assumed that recurring irritation, radiation and long-term use of IUDs (intrauterine device) favor the development of vaginal cancer. In most cases, however, they are more likely to be tumors of the surrounding organs that spread into the vagina. Vaginal cancer is mostly squamous cell carcinoma and tends to cross the boundaries of the organs. For example, the rectum or the urinary bladder are also affected. Many women complain of bleeding after intercourse and hardening of the mucous membrane. In addition, the vaginal fluid turns red. If the tumor affects or displaces the rectum and urinary bladder, it can also cause discomfort when urinating and defecating. Depending on where the tumor is and how big it is, different therapeutic approaches come into question. In order to successfully remove the tumor, the vagina must often be removed, and possibly the uterus as well. If the tumor is too large, local radiation can be performed to reduce the tumor mass. Relapses are common despite successful therapy.
Read more on the subject at: Vaginal cancer
Discharge from the vagina
The secretion of vaginal fluid can be increased for various reasons. During sexual arousal, more fluid is produced to enable smooth sexual intercourse. Infections from bacteria, fungi, or other pathogens can also lead to increased discharge. Hormonal disorders (lack of estrogen and excess estrogen or gestagen), such as during pregnancy or during the menopause, also affect the secretion of vaginal fluid. In addition, there are misconduct such as excessive intimate hygiene or non-adapted douches that lead to a pH change. Before initiating therapy, it is important to find the trigger. Increased secretion can only be successfully treated if the therapy is appropriate and targeted. Important differentiating criteria are, for example, the amount, color and consistency of the discharge, whether there is itching or whether certain medications (contraceptives, hormones) are taken. A tissue sample should also be taken to rule out cancer.
Swollen vagina - what's behind it?
Vaginal swelling can have a number of causes. For example, a swollen vagina can result from an accumulation of blood: Blood accumulates in the labia and makes them look larger. This accumulation is normal in the context of sexual arousal. Any swelling that persists after intercourse may indicate irritation of the mucous membrane or the labia. Gels, sexual toys and pubic hair can all cause irritation. If the swelling does not appear immediately after intercourse and is also painful, this indicates an infection. Various pathogens can cause the vagina to swell, especially sexually transmitted pathogens. For example, infection with the Treponema pallidum bacterium can lead to syphilis (also known as syphilis). The first symptoms are a painless ulcer in the genital area and swelling of the nearby lymph nodes. Genital herpes can also lead to swelling and itchy blisters on the genitals. Infestation by the parasite Trichomonas vaginalis can also lead to inflammation (trichomoniasis). This inflammation is often accompanied by redness and swelling of the vagina. If the swelling feels lumpy or hard, it could be an indication of a malignant vaginal disease.
Another typical clinical picture that can cause vaginal swelling is so-called bartholinitis. This is an inflammation and clogging of the Bartholin glands in the vaginal wall. This inflammation can cause a large swelling with severe pain.
Read more on the subject below Bartholinitis.
Vaginal tear
A rupture of the vagina is called a vaginal tear. This injury can have various causes. The most common cause is birth trauma during natural delivery. Using a suction cup or forceps can injure the vagina and cause it to tear. Even if the child's head is too big compared to the birth canal, it can rupture. Vaginal ruptures can also result from sexual trauma, such as rape or the introduction of a foreign body into the vagina. A ruptured vagina is usually painful, although the intensity of the pain varies from woman to woman. The tear usually occurs lengthways and can lead to bleeding. Vaginal tears are more common in women with a weak cervix (cervical insufficiency) during pregnancy or with a tear in the perineum. Previous vaginal injuries also leave scars and lead to instability and vulnerability of the tissue. In severe cases, the connection between the uterus and vagina can be completely torn off (so-called colporrhexis). The therapy of choice for a torn vagina is surgical suture.
Further information on this topic can be found at: Vaginal tear - can it be prevented?
Vaginal cramp
The uncontrolled cramping of the pelvic floor muscles that leads to a closure of the vagina is called vaginismus. The spasmodic closure of the vagina makes it difficult or even prevents any penetration into the vagina. For this reason, a sex life is severely restricted by vaginal cramps. The use of tampons or gynecological examinations is also particularly difficult in everyday life. Vaginal cramps are divided into primary and secondary vaginismus. Primary vaginismus is congenital and mostly complete, i.e. the spasms prevent any penetration into the vagina. Secondary vaginismus develops over the course of life and is often incomplete. Secondary vaginismus mostly only affects sexual intercourse and makes sex life very difficult. Vaginal cramps are always psychological and often occur as a reaction to trauma (rape, painful childbirth). The therapy of choice is psychotherapy or behavioral treatment by a psychologist to deal with the underlying problem. Stretching can also help reduce the severity of the cramps.
Read more on this topic at: Vaginal cramp.
Injuries to the vagina
Injuries to the vagina can occur in a number of different ways. Examples include sexual intercourse (cohabitation), rape, circumcision, the intrusion of a foreign body, surgery or defloration (defloration, tearing of the hymen).
An injury to the vagina through cohabitation usually manifests as a tear in the posterior vaginal vault, which leads to profuse bleeding and requires surgical treatment.
In the case of rape, on the other hand, the tear is usually on the side of the vaginal vault.
Changes in the position of the vagina
In the event of a lowering (Descensus) the vagina and uterus go deeper as a whole due to weakness of the pelvic floor muscles or the connective tissue or due to increased pressure in the abdomen, but not so far that they are visible to the outside.
In the event that the organs step outside, it is called an incident (Prolapse). With these diseases, patients complain of a feeling of pressure, pain in the lower back and poor urine control (Incontinence). These complaints are treated either with pelvic floor exercises or in the event of an incident (Prolapse) operational.
You might also be interested in the following articles: Uterus subsidence and prolapse
Vaginal abnormalities
Congenital malformations exist as further clinical pictures relating to the vagina (Anomalies). These can be the hymen (Hymen) or affect the vagina as a whole.
In this context, vaginal aplasia occurs, which is understood to mean a lack of development of the created vagina. Another clinical picture is the septate vagina, where the vagina is partially or completely divided by a septum.
Hymenal atresia can also occur in newborns. Here the opening of the hymen is missing.
All of these anomalies are treated surgically.











.jpg)