Wisdom tooth
development
The third molar (Wisdom teeth) develop very late, between the ages of 18 and 25, and for this reason are known as wisdom teeth.
In some adolescents, the first mineralization is not visible on the X-ray until they are 14 years of age.
In others, wisdom teeth never break through.

shape
The wisdom teeth belong to the molars, but do not follow any specific rules in their structure.
So there are wisdom teeth with only three humps, but also with five tooth humps.
Also the number of root is very different and some of them are fused together or bent into a hook shape. This can include the removal of the Tooth roots make it much more difficult. In very rare cases further molars can grow behind the wisdom teeth, which are then called "Nines“Or also called distomolars.
clinic
Because of these significant differences and the irregularity of their occurrence in one jaw the wisdom teeth can lead to significant problems.
The upper wisdom teeth are usually less of a problem than the lower ones. A common problem is limited space.
Since the wisdom teeth erupt as the last molars at the back of the jaw angle, there is often insufficient space so that they cannot erupt or only partially erupt.
When the teeth don't erupt at all (full retention) there are usually no symptoms. Partially erupted teeth (partially retained) can cause inflammation and Abscesses to lead. These are very painful and can lead to general symptoms fever and exhaustion lead.
If the wisdom teeth only grow in the upper or lower jaw, they lack their opponents when they grow, so that they grow beyond the occlusal plane. This also often results in a shift of the teeth, which leads to tooth damage at night Grinding teeth and TMJ discomfort can lead.
If symptoms of this kind occur, the wisdom teeth must be surgically removed (extraction). If the tooth germs are removed before they break through, one speaks of one Germectomy.

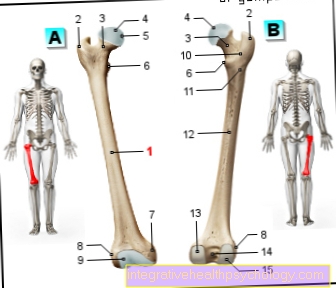
a - tooth crown - Corona dentis
b - tooth neck - Cervix dentis
c - tooth root - Radix dentis
- Tooth enamel -
Enamelum - Dentin (= dentine) -
Dentinum - Tooth pulp in the tooth cavity -
Pulp dentis in Cavitas dentis - Gums -
Gingiva - Root canal
- Cement -
Cementum - Root skin - Periodontium
- Opening of the tooth root tip -
Foramen apicale dentis - Nerve fibers
- Alveolar bone (tooth-bearing
Part of the jawbone) -
Pars alveolaris
(Alveolar process) - Blood vessels
- Tooth root tip -
Apex denitis - Point of division of the tooth roots
(Fork) - Bifurcation - Tooth furrow
You can find an overview of all Dr-Gumpert images at: medical illustrations
Inflammation of the wisdom tooth
Pain and inflammation in the wisdom tooth are triggered by various causes. As with other teeth, tooth decay can cause the tip of the root to become inflamed, causing pain and a thick cheek. A typical symptom that leads to an inflamed wisdom tooth is the "dentitio difficilis". This is a difficult tooth eruption due to lack of space or an unfavorable position of the tooth. ly the two lower wisdom teeth are affected. Often the tooth does not break through completely, so that a gum pocket is created on the back surface.
Read more on the topic: Inflammation of the wisdom tooth
In some cases even the chewing surface is still covered by mucous membrane. These areas are not easily accessible to the toothbrush, so that bacteria can multiply quickly through the accumulated food residues. The resulting plaque can then trigger tooth decay and inflammation of the gums. Often the dentist is then visited, who can quickly provide relief in the event of acute problems.
He removes the hard-to-reach plaque with special instruments and then puts a drug into the gingival pocket. The area heals within a few days. In most cases, however, further inflammation cannot be prevented. The excess mucous membrane or the entire tooth must then be removed in order to sustainably alleviate the pain. The dentist decides exactly which therapy is suitable based on the individual situation.
Wisdom tooth pain
Sore wisdom teeth are an extremely common symptom. Most of the time, they appear similar to swelling in adolescence due to difficult tooth eruption. Due to the lack of space, it can happen that the wisdom tooth erupts incompletely and does not reach the occlusal plane. However, since part of the tooth can usually be seen, gingival pockets can form. Inflammation is felt here as a throbbing. Furthermore, a transverse wisdom tooth in the lower jaw can press on the root of the tooth in front of it. A growth spurt can increase the pressure and lead to pain if it persists for a long time.
Read more on the topic: Wisdom tooth pain
Swelling of the wisdom tooth
Swelling of the soft tissues (gums) can occur when the wisdom tooth erupts. Often it is a symptom of difficult tooth eruption and goes along with it Pain, swollen lymph nodes and possibly a jaw clamp. Especially those lower wisdom teeth are affected by this. Since the teeth erupt only partially or at an angle in the majority of cases, the Hygiene is very difficult. A Inflammation of the gums can set in and thus further promote the swelling. A single occurrence of these complaints is not a problem. If this occurs more frequently, you should consider removing the affected wisdom tooth so that the tooth in front of it is not damaged.
Have surgery on the wisdom tooth / wisdom tooth pulled
If one or more wisdom teeth are to be removed, a detailed consultation must have taken place at least one day in advance. The dentist must personally communicate the advantages and disadvantages, as well as risks and complications, and any questions raised should be clarified. This advice may not be taken over by the dental assistant. The extraction, as the tooth extraction is also called, begins after the oral cavity has been inspected with local anesthesia. The tooth nerve is numbed by a syringe so that pain stimuli are no longer transmitted. However, it is normal to pull or push gently during the operation.
Read more on the topic: Operation on the wisdom tooth
After the anesthetic works, the dentist will begin removing it. The wisdom teeth in the lower jaw often require an incision in the mucous membrane so that the tooth is completely visible. Depending on how deep the tooth is still, the bone under the gum has to be milled away. If the wisdom tooth is completely visible, it is levered out of its tooth socket with another instrument, the Bein’s lever. If the tooth is very crooked or has very crooked roots, it is divided and then removed in several pieces. After it has been checked that the tooth has been completely removed, the inflammatory tissue is removed. To do this, the tooth socket is scraped out with a spoon-like instrument.
If the wound is very large, another drug can be placed in the alveolus before the mucous membrane is sutured back in the correct position. In the upper jaw, the teeth usually protrude completely from the mucous membrane, so that no additional incision is necessary here. However, a connection to the maxillary sinus can open up here if the wisdom tooth had long roots. This common complication, also known as the mouth-antrum connection, can be confirmed by simple tests. The wound must then be closed with a suture to prevent chronic inflammation caused by a persistent connection between the mouth and maxillary sinus.
After closing all wounds, the dentist usually explains what to do after an operation. In the first few days after the operation, it is important, for example, to cool the cheek well to avoid swelling, to refrain from smoking, and to eat soft foods. In this way, the risk of inflammation can be reduced to a minimum. Then the patient is discharged with a prescription for the important medication. Usually a wound check follows the day after, as well as a suture removal after about a week.
This could also be of interest to you: Wisdom tooth pulling under general anesthesia - when does it make sense?
Inflammation after a wisdom tooth operation
After a wisdom tooth has been removed, inflammation is not uncommon. The causes are often already existing difficulties in this region due to the location or a difficult tooth eruption. But also a tooth root left behind in the tooth socket or an inflamed alveolus can cause similar complaints. If you follow the medical advice on how to behave, the risk of inflammation can be greatly reduced. For example, you shouldn't smoke after an operation and you shouldn't eat anything crumbly. In certain cases it is also advisable to administer antibiotics, for example if the surgical area was often inflamed before.
If an infection does occur, there are typical signs of inflammation that appear after a short time. Despite taking painkillers such as ibuprophen or paracetamol, the pain cannot be relieved properly. There is also a reddening of the wound and a swelling of the cheek. The wound area is often warmed up by increased blood flow, and fever is not uncommon. If the typical loss of function then occurs, it can be very dangerous.
Read more on the topic: Inflammation after a wisdom tooth operation
An abscess lifts the floor of the mouth or causes the throat to swell. This caused shortness of breath and a feeling of suffocation. Since an abscess can also spread to internal organs, a medical examination is urgently recommended. A (dental) doctor's visit should take place immediately after the signs of inflammation have ceased, preferably at an early stage.