Tendon injuries to the knee joint
synonym
- Patellar tendon tear
- Patellar tendon tear
- Biceps tendon tear
- Quadriceps tendon ruptured
definition

As Tendons one denotes the ends of the Muscles. The musculature ends in tendons and is connected to it bone attached. In order to be able to move a joint, you have to pull over it.
The Kneecap lies embedded in such a tendon (Quadriceps tendon). The quadriceps tendon (tendon of the Thigh muscle) from below through the so-called patellar tendon (patella (lat.) = kneecap) held. If one speaks of a patellar tendon tear, then one means the tear of the tendon below the kneecap.
Summary
Ruptures of the patellar tendon (Patellar tendon tear) are very rare and usually occur as a result of trauma or an enormous amount of force exerted by the muscle. If the tendon breaks, it can leg no longer be stretched against resistance and one Operation becomes necessary. Other complaints of the person concerned are pain and swelling. The ultimate diagnosis is made by means of CT but mostly MRI posed.
Appointment with a knee specialist?
I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
root cause
Most often, a torn kneecap tendon is caused by trauma due to lifting, i.e. when the strong thigh muscle (Quadriceps muscle) has to provide an extremely high braking power. On the other hand, even with uncomplicated knee injuries, it can tear off or injure the Patellar tendon come.
Symptoms
Like everyone else Tendon tear this also causes pain and swelling of the knee joint. Usually the rupture is also associated with soft tissue damage (Damage to non-bony structures such as muscles or other tissues) associated. The kneecap is elevated due to the lack of downward traction.
The rupture of the kneecap also has other noticeable consequences for those affected: the leg can no longer be stretched. This is due to the fact that the tendon is attached to the front edge of the shin below the kneecap, the thigh muscle pulls on the shin and thus that Knee joint stretches.
diagnosis

For rough orientation and to determine Effusion in the knee can a Ultrasonic be made. Here you will be able to see the torn tendon indirectly: it is missing in the affected area.
The MRI scan of the knee joint, the one allows more precise diagnostics. With an MRI of the knee, partial tears of the tendon or even just overstretching can be made visible.
MRI knee joint
The tendons of various muscles attach to the knee joint. The most prominent tendon is the tendon of Quadriceps musclethat spans the kneecap and inserts as a patellar tendon on the front of the tibia. The tendons of the various muscles are often affected when the knee joint is injured. Complete tendons are severed as well as partial tears.
For the diagnostic confirmation of the injury is a MRI scan of the knee joint Recommended because the soft tissue is shown very well.
Tears and partial tears of the tendons can thus be recorded very well. Inflammation of the tendons, e.g. the Inflammation of the quadriceps tendon, can be displayed in the MRI. An inflamed tendon usually appears thickened on MRI and shows increased signal intensity - this means that it looks lighter or darker than normal on the MRI images.
Furthermore, fluid accumulations in the bones can also be detected as additional accompanying injuries in the MRI. This bone marrow edema (also called "bone bruise") shows up on the MRI as a reduced or increased signal intensity in the bone in the affected area.
prophylaxis
A prevention of the Ruptured patellar tendon is difficult to do. Causing situations should of course be avoided. A strong muscle structure, which gives the knee joint stability on all sides, is probably the best way to prevent injury.
Quadriceps tendon injury
Quadriceps tendon ruptured
An acute one Quadriceps tendon rupture is clearly shown by a stretch deficit in the knee joint. The tendon attaches to that of the Teresitas Tibiae (bony roughening on the anterior upper part of the tibia) and has embedded the patella (Kneecap). The quadriceps muscle is the main extensor in the knee joint.
With a complete rupture of these tendons, the ability of the affected leg to stretch is almost completely lost.
This can be tested by having the patient e.g. should bend the knee while sitting with the thigh fixed. This is not possible with a complete rupture. In the event of a partial tear, the stretching force may still be retained.
When looking at the knee, there is a cranial indentation (above) of the kneecap in the course of the tendon. The tear of the tendon can also be noticeable by palpation. The ultrasound of the tendon will most certainly notice the rupture.
One of the most common reasons for quadriceps tendon rupture is to fall onto the flexed knee. In this state the tendon is already very stretched to the maximum.
With an additional pull by the forced (forced) Flexion when falling, it is sometimes no longer able to withstand this acute force and ruptures. This happens especially in older patients whose tendons have lost their strength and elasticity. In this patient clientele, the tendon often tears cranially (above - towards the thigh) the kneecap. In younger patients, the kneecap tears away and tears off.
A rupture must be treated surgically!
The operation of the quadriceps tendon
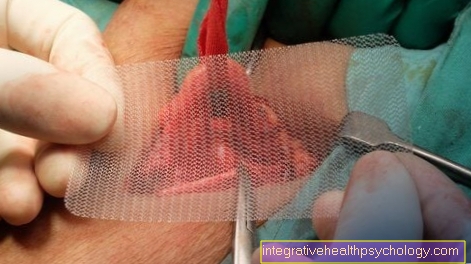
The incision is made on the outside along the quadriceps tendon.
In the next step, the fasciae are removed from the affected area with individual incisions. Now the tear in the tendon is searched for and exposed. If the capsule is impaired, it is also attached.
The tendon is adapted again with simple sutures (the stumps pulled together). These seams are End-to-end sewn into the tendon. They are placed in all layers of the tendon.
Often absorbable sutures are used here, which are broken down by the body after a certain time. In addition, a frame seam is placed to ensure that the seams do not tear.
This suture is sewn in a loop through the upper tendon stump and is usually made of non-absorbable material. It is pulled lengthways through the lower stump and then anchored in the kneecap. This is done by drilling a horizontal channel through the kneecap through which the suture is drawn. In addition, so-called augmentations can be used for backup.
Absorbable cords are used for this. These take over part of the tensile force from the tendon. After a certain time, however, they are absorbed by the body, i.e. they are broken down.
At this point, however, the tendon has healed enough that it can fully bear the tensile force again.
If the quadriceps has not ruptured but is torn from its bony anchorage in the kneecap, then the tendon must be reattached. This is done through small, perpendicular holes. Sutures are drawn through these holes and sewn into the torn tendon. Here, too, a frame seam is created to prevent tearing.
Aftercare
After the operation, the leg has to be immobilized for 3 weeks. In the course of a physiotherapeutic follow-up treatment, the knee is brought back to full mobility.
If a patient presents with an old rupture that had not been operated on, an operation should also be performed. Often these patients complain of weakness when stretching the knee. This is because the tendon is longer due to scarred healing. It grew back together by itself - but it's too long. During the surgical procedure, the tendon is shortened.
This is where the tendon z-shaped cut into two triangular ends. These are now placed on top of one another until the desired length of the tendon is reached.
As a further option, the scarred part that has grown back in the former rupture gap of the tendon can be cut out and the two stumps sewn together like a complete rupture.
If a ruptured site is to be reinforced, reverse plastic surgery can be used. A thin flap is cut from the front of the quadriceps tendon elsewhere. This flap is then placed over the already sutured rupture site and also sutured back into the eye.
The prognosis is usually very good and the patient can use the knee without complications after the treatment. A possible complication would be a new rupture in the event of premature loading. It is possible that the sutures were insufficient (insufficient).
Injury to the patellar tendon
The rupture of the patellar tendon (also Ligamentum patellae called) shows it like the rupture of the quadriceps tendon due to an extension deficit of the knee. This is explained by the fact that the patellar ligament is ultimately only the continuation of the quadriceps tendon below the kneecap - i.e. it is responsible for transmitting the stretching force of the quadriceps in the knee.
The x-ray should ensure that there are no bony injuries. A lateral x-ray can be used to diagnose a tear in the patellar tendon by having a Kneecap elevated present. In normal condition, the patellar tendon pulls the kneecap caudally (below). In the event of a crack, the kneecap moves cranially (above).
causes
Cause of one Torn patellar tendon As with the quadriceps tendon rupture, lies in a fall on the knee, which is already strongly to maximally bent. The patellar tendon can no longer be stretched and ruptures in the fall, which would require it to stretch even more.
Particularly in older patients, in whom the tendons' ability to stretch is reduced, the tendons tend to tear. Younger patients tend to tear the tendon from the lower pole of the kneecap. A more complicated rupture occurs when the Tibial tuberosity tears off - i.e. when the attachment point of the tendon completely or partially from the Tibia (Shin) tears off.
If the patellar tendon is diagnosed with rupture, surgical treatment is essential.
surgery
An incision is made along the knee from the kneecap to the level of the tendon insertion (Tibial tuberosity/ slightly below the shin-joint plateau).
The rupture site is exposed and the surrounding structures and tendons are checked for possible injuries. The two stumps are made with so-called Braid seams connected. A thread is used that is sewn lengthways through the tendon and is continued parallel to the rupture site so that a square suture is created at the end.
In addition, absorbable sutures are inserted directly into the two stumps so that the two ends are pulled directly together. As a further securing mechanism, a frame suture is inserted, which is pulled through the kneecap through a horizontally drilled channel, so that the tendon is pulled taut against the kneecap. In addition, the frame suture can be fastened through the tibial tuberosity through a horizontal hole. This ensures that the tendon is stretched tightly between the kneecap and the attachment point and, above all, is securely attached.
Aftercare
In order to achieve the correct length of the patalleal ligament, an X-ray of the other knee is made and the appropriate length is then set up accordingly. As with the restoration of the quadriceps tendon, a Z-plasty can be used. If the amount of functional tendon tissue is insufficient, the tendon of the semitendinosus muscle can be used.
Drains must be left in place after the operation to allow blood and other fluids to drain. At the beginning a thigh cast must be worn for about 1-2 weeks. This is split - means cut open so that swelling of the thighs in the cast does not lead to a narrowing. Then a normal cast can be applied. This must be worn for a period of around one and a half months.
In the course of the follow-up treatment, careful training with physiotherapy and controlled strength training is necessary. It should be ensured that there is no premature overload (avoiding ruptures in the healing process).