Intercostal neuralgia
introduction
In medicine, neuralgia describes pain that can arise along a nerve and its supply area. Intercostal neuralgia is therefore a nerve pain that affects the nerves of the intercostal spaces (inter - between; costa - rib).
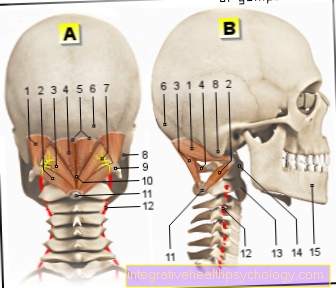
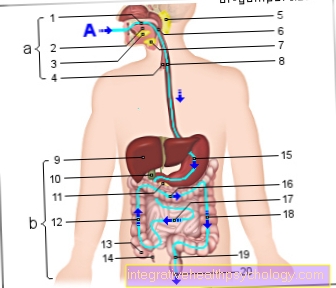
The intercostal spaces, as the name suggests, extend between two ribs. They are formed by the muscles lying there (musculus intercostalis externus and internus), which in turn are enclosed on the outside by the outer and inner chest wall fascia, which must be imagined as tight and firm connective tissue sheaths. In the immediate vicinity, namely on the underside of each rib, run the blood vessels of the intercostal spaces as well as a corresponding nerve - the intercostal nerve. This nerve innervates the intercostal muscles and the abdominal muscles. In intercostal neuralgia, these intercostal nerves are the trigger and cause stabbing, pulling, and possibly persistent pain.

causes
In the vast majority of cases, intercostal neuralgia is caused by an underlying disease, so that in principle it is not an independent disease. Rather, it can be described as a complaint that arises in the context of another ailment.
There can be many different causes for intercostal neuralgia. Possible origins can be the spinal cord or the spine.
If the spine is the cause of the disease, degenerative diseases are usually the trigger. These are diseases that are associated with a breakdown or regression of certain structures of the spine and can be traced back to genetic predisposition or permanent harmful influences.
As part of these diseases, it is possible that nerve roots become trapped and irritated, which can then lead to intercostal neuralgia. This includes, for example, what is known as osteochondrosis, in which there is increased wear and tear on intervertebral discs and vertebral bodies. Even with herniated discs, which often, but not necessarily, occur due to excessive stress, nerve roots can become trapped. A herniated disc can therefore also be a possible cause.
Likewise, traumatic (accident-related) changes, such as fractures (broken bones), in particular rib fractures, can, in the worst case, lead to mechanical pressure on the nerve roots and trigger intercostal neuralgia.
A myogelosis resulting from physical work or intensive sporting activity (hardening of the intercostal muscles caused by overexertion or incorrect loading) is a conceivable cause.
An operation that involves opening the chest or even removing ribs can also be a possible reason for intercostal neuralgia.
You may also be interested in this topic:
- Nerve root entrapment
Infectious causes
Infectious diseases can also be responsible for the occurrence, as it can lead to nerve inflammation or nerve irritation in their course. The most clinically known trigger is infection with the varicella zoster virus, which causes herpes zoster, also popularly known as shingles. In the course of the disease, nerves can become inflamed, which promotes the occurrence of intercostal neuralgia. The pain may still be present even after shingles has healed.
In the context of infectious disease processes that take place in the immediate vicinity of the intercostal nerves, nerve root irritation or damage can occur.
So it is possible that intercostal neuralgia occurs as a result of diseases such as pneumonia, tuberculosis, osteomyelitis or pleurisy.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You will find me:
- - orthopedic surgeons
14
You can make an appointment here.
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
For more information about myself, see - Orthopedists.
Frequency distribution
Exact numbers are sometimes not known directly. Basically, however, intercostal neuralgia is one rare disease.
diagnosis
When diagnosing a Intercostal neuralgia Early diagnosis is of enormous importance. Because if the pain persists for a longer period of time without treatment Risk of chronification, that is, persistent pain, possibly for a lifetime.
The diagnosis of intercostal neuralgia requires a comprehensive one History takingto track down the underlying disease that is responsible for intercostal neuralgia. By a Palpation examination certain pressure points can be stimulated. Lead this to characteristic pain, the suspected diagnosis of hissing rib neuralgia can be confirmed.
To clarify the actual Underlying disease further procedures can then be used. Above all, are conceivable here imaging procedures such as an x-ray of the chest or spine to check for any disease or damage to the skeletal system. Other imaging techniques such as Ultrasound (sonography), Computed tomography (CT) or Magnetic resonance imaging (MRI) can provide important diagnostic information, depending on the underlying disease.
Symptoms
In intercostal neuralgia, belt-shaped, stabbing, pulling, and possibly persistent pain occurs in most cases.
They can get stronger or weaker at times, or suddenly become extremely strong out of nowhere. The pain occurs in the area of the chest. Those affected also report the pain radiating to the back. Certain movements of the chest or coughing can make the symptoms worse. Intercostal neuralgia can also lead to sensory disorders of the skin and itching.
In addition to the pain, intercostal neuralgia is also a psychological burden.
Patients who suffer from constant pain often experience panic or even fear of death, as particularly severe pain can lead to shortness of breath and possibly also make breathing difficult. This is why it is often assumed that the symptoms come from the heart or the lungs.
The fact that some patients suffer from pain almost all of the time, and over a longer period of time, can have a negative impact on the psyche of those affected and, in the worst case, trigger depression.
Do you have pain between your ribs but the symptoms are inconsistent with intercostal neuralgia? Read more about this:
- Symptoms and causes of pain between the ribs.
Pain
The main symptom of intercostal neuralgia is severe pain in the area supplied by the affected nerve.
These are usually expressed by movement-dependent, belt-shaped pain in the course of a space between the ribs. Often, even light movements are enough to trigger the pain. Expanding the chest when breathing in can be sufficient for this. Affected patients often report the pain with great intensity. They can be accompanied by discomfort and tingling sensations.
Read more about this:
- Nerve pain
Shortness of breath
The nerves that are affected in intercostal neuralgia are not responsible for the respiratory muscles. This means that breathing cannot come to a standstill because both the diaphragm and the auxiliary breathing muscles can work.
However, intercostal neuralgia is accompanied by severe pain between the costal arches. These intensify when the chest moves, e.g. on inhalation and exhalation. In pain-plagued patients, this can lead to extremely shallow breathing, which can be accompanied by a subjective feeling of shortness of breath or even fear of death. In this case the patient should be encouraged to breathe as calmly as possible and to relax. Relief from pain through appropriate pain management will help prevent shortness of breath from occurring.
What symptoms suggest a cause in the heart?
In the case of acute pain in the chest area, as is also the case with intercostal neuralgia, one should always keep a cause of the heart in mind.
Above all, the life-threatening heart attack should not be neglected. In addition to acute chest pain, a heart attack often also radiates pain, especially in the left arm. Accompanying abdominal pain is also possible. Many patients with a heart attack have sudden shortness of breath and often suffer from extreme panic and even fear of death. A heart attack is often much more dramatic than an intercostal neuralgia. However, especially in women and also in diabetes patients (diabetes), a very subliminal course of a heart attack can occur.
Therefore, if chest pain occurs suddenly, a doctor should always be consulted, e.g. Can rule out a dangerous heart attack with the help of an EKG.
- Signs of a heart attack
- Heart attack risk
therapy
When treating intercostal neuralgia, the first thing that is treated is the underlying disease in the context of which the intercostal neuralgia occurred or developed. It often happens that no clear cause can be found, so that the symptoms are treated. This means that primarily the pain is treated with medication.
You can choose from the so-called non-steroidal anti-inflammatory drugs, for example, which have both pain-relieving and anti-inflammatory effects. Examples are ibuprofen and aspirin. Both drugs are available in all pharmacies without a prescription, but the maximum daily dose indicated should be observed when taking them, otherwise severe side effects may occur. Long-term use of the pain medication should also be discussed with a doctor.
In the case of more severe pain, the significantly more potent (more effective) opioids can be used, which, with a few exceptions, are subject to the Narcotics Act (e.g. morphine). They may only be used in very severe pain. Opioids are both potentially addictive and have some undesirable side effects.
Pain inhibition can also be achieved by injecting a local anesthetic. These are drugs that only provide an anesthetic to the site of application.
The use of muscle relaxants, i.e. substances that relax the muscles, can also be promising under certain circumstances, as can manual therapy or physiotherapy.
Furthermore, the use of so-called transcutaneous (trans- through; cutis - skin) electrical nerve stimulation is also quite conceivable as a treatment option. The effectiveness of this method has not been proven in every case, but it is a popular method because no medication has to be prescribed.
Read more on the subject at:
- Duration of an inflammation of the nerves - what you should be aware of!
Home remedies
Many patients resort to home remedies for intercostal neuralgia. In particular, heating and cooling applications can be helpful here. These can be done with moist compresses or warm grain pillows, for example.
Since an intercostal neuralgia is often associated with improper stress in the back area, it is also important to make your everyday life as easy on your back as possible. Attention should be paid to good posture, heavy carrying should be avoided and objects should be picked up from a crouch without straining the back. In this way you can contribute a lot to healing but also to the prevention of intercostal neuralgia.
Are heat applications better or cold?
Both heat and cold applications can relieve pain in intercostal neuralgia. Heat patches or a warm grain pillow can release muscular tension in the back area and relieve the affected nerves.
For some patients, however, it helps more to work with cold. This can be very beneficial, especially with inflammatory causes of intercostal neuralgia. It remains to be recommended that the affected patient tries both and can find a remedy with light home remedies.
homeopathy
Homeopathic remedies can also be used concomitantly. It should be noted here that there is currently no scientifically proven effect of homeopathy and that it can only be used in conjunction with medically guided therapy.
E.g. Arsenicum album, Colocynthis, Rhus toxicodendron and Ranunculus bulbosus provide relief from burning, neuralgic pains. A suitable combination can be put together for you by an experienced homeopath.
Which doctor treats neuralgia?
If an intercostal neuralgia occurs, the first step should be to see your doctor. He or she can carry out the first doctor-patient interview and the physical examination and make an initial suspected diagnosis. Is it an uncomplicated intercostal neuralgia e.g. In the context of muscular tension, the therapy can be carried out by a general practitioner with painkillers and, if necessary, physiotherapy.
If there is evidence of a traumatic injury to a rib or even a herniated disc, imaging by a radiologist or treatment by an orthopedic surgeon may be necessary. If these injuries make an operation necessary, an appropriate surgeon must of course be called in. In the vast majority of cases of intercostal neuralgia, however, targeted treatment by a family doctor or an orthopedic surgeon in an outpatient setting should be sufficient.
prophylaxis
Due to the fact that the intercostal neuralgia as part of another illness occurs, prevention of neuralgia in itself is practically impossible.
In the case of heavy physical work or regular sporting activities you should therefore rely on the correct movement be respected. The strain and the Warm up the muscles can have a positive effect. In order to avoid the pain that occurs becoming chronic, professional help should be sought immediately if possible.
forecast
The prognosis for intercostal neuralgia varies depending on which one Underlying disease has preceded.
If the original disease is identified and treated early enough, the prognosis is good. It worsens the longer the pain is left untreated, in part because the underlying condition cannot be clearly identified.
If the pain persists over a longer period of time, there is a risk that it will develop chronic pain syndrome trains what a great mental stress can cause.
Duration
The period of time during which patients suffer from intercostal neuralgia varies greatly from person to person and depends largely on the cause of the neuralgia.
If it is a symptom that occurred as part of a rib injury, the pain can last for several weeks until the original injury has healed. Intercostal neuralgia, which occurs as part of inflammation, usually heals much faster. A quick and correct diagnosis of the cause is crucial for the fastest possible pain relief so that an appropriate therapy can be initiated.
How long are you unable to work?
Intercostal neuralgia is usually an extremely painful disease and in many cases leads to temporary incapacity for work.
How long this lasts is very individual from patient to patient. The different causes of intercostal neuralgia each have a different healing time. The occupation practiced can also influence the length of the sick leave. For example, patients with a job with high physical stress may need a longer period of rest. The individual duration of the incapacity to work must be discussed with the attending physician and at least freedom from pain should be achieved before work is resumed.
When can you start exercising again?
Many patients with intercostal neuralgia ask themselves when they are allowed to do more physical activity again and also when they can do sports. This is a decision that must be made individually for each patient together with the doctor and is largely dependent on the cause of the intercostal neuralgia.
Did this e.g. in the context of a rib injury, it is important to wait until it has healed completely in order to rule out another injury. It is important to note that only in very few cases is it necessary to take complete physical rest. Often, light physical activity is helpful in the healing process. Consultation with the attending physician should be held here and, if necessary, aids such as physiotherapy should be used.