Angina pectoris
definition
Angina pectoris is an insufficient supply of oxygen to the heart, which is associated with attack-like pain. Angina pectoris is divided into stable, unstable and Prinzmetal angina. All are based on an insufficient supply of oxygen to the heart. Prinzmetal's angina differs from the other two in the cause of the insufficient supply.
With around 300,000 hospital admissions per year, angina pectoris is one of the most common causes of hospitalization.

Symptoms
The most common symptoms are listed and explained below.
- Chest pain / pain behind the sternum
- Chest tightness / pressure on the chest
- Shortness of breath
- Fear / panic
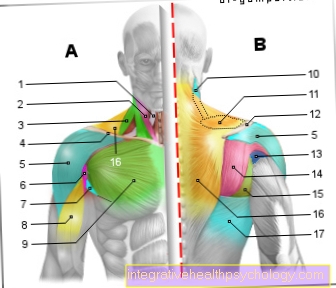
- Back pain
- Neck / sore throat
- Upper abdominal pain, nausea / vomiting
- Pain in the left arm / left shoulder
- Jaw / toothache
You can find more on this topic on our subpage: Symptoms of angina pectoris
Chest pain and tightness in the chest
The typical symptom of angina pectoris is sudden onset of chest pain behind the breastbone, which most patients find dull, oppressive or constricting.
Chest pain is the leading symptom in heart disease. Angina pectoris itself describes the tightness of the chest and chest pain that arise due to coronary heart disease (CHD). CHD leads to an insufficient supply of the heart muscles and thus causes pain. Most of the time, the pain is felt in the chest area, often just behind the breastbone. The chest is also affected by a feeling of pressure or tightness. Those affected describe the feeling as if someone had put a heavy sack on their chest. The chest pain and tightness in angina pectoris typically appear seizures and last for about one to five minutes. Such an angina pectoris attack is often triggered by stress or physical strain. It can usually be relieved well with nitro spray.
Only rarely do the patients only feel a feeling of pressure or anxiety, a tightness or a burning sensation in the chest. In many cases, the pain radiates to the left arm, but it is less common to radiate to the right arm or both arms, but it is possible.
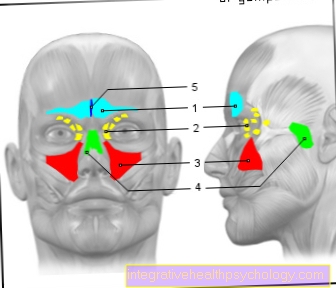
Angina pectoris can also radiate to the neck, lower jaw, back, or upper abdomen.
More on this topic at: Chest pressure- what to do
Fear or panic
The symptoms of angina pectoris are very similar to those of a heart attack and should definitely be taken seriously as a warning symptom. Chest pain can be accompanied by shortness of breath, weakness and dizziness.
Affected people very often have feelings of fear or even fear of death.
Angina pectoris is often triggered in pre-stressed people by physical exertion such as climbing stairs or fast walking. Emotional stress such as stress or arguments can also cause angina pectoris. A cold outside temperature and a large meal shortly before the onset of symptoms can make the pain worse, but it can also trigger it.
Angina pectoris usually lasts five to fifteen minutes and gets better with rest or the administration of nitro spray, which contains the active ingredient nitroglycerin and increases blood flow to the heart muscle and thus alleviates the symptoms.
In patients with diabetes mellitus, angina pectoris can also run completely unnoticed, since diabetics perceive the pain differently than patients without diabetes due to the nerve damage caused by diabetes (diabetic neuropathy). Such angina pectoris is referred to as "silent angina pectoris".
Back pain
In addition to chest pain, back pain is also one of the symptoms of angina pectoris. Many sufferers describe pain that runs in a belt-shaped manner around the chest. The chest and back are equally affected by pain. Attack-like pain in particular indicates angina pectoris. Usually the pain is perceived as dull, stabbing, or piercing. Since the heart is affected in angina pectoris, the back pain is usually felt at the level of the thoracic spine.
Read more on the topic: pain in the back
Nausea and upper abdominal pain
Women, older people over 75 years of age and patients who have had heart surgery also perceive pain differently, so that in these groups of people, above all, unspecific symptoms can be observed, including nausea, dizziness, shortness of breath or radiation to the upper abdomen. Chest pain can be completely absent.
Angina pectoris is said to be stable if the symptoms remain the same over a long period of time in several episodes. Unstable angina pectoris refers to the first occurrence of angina pectoris or an angina pectoris attack that is stronger than the previous attack.
Typical signs of angina pectoris
The first signs of angina pectoris are usually noticeable during physical exertion or psychological stress. In such situations, the body's need for oxygen increases. As a result, the heart has to do more pumping work, which in turn requires a better blood supply to the heart. However, the increased blood flow to the heart muscles is not possible due to the coronary heart disease, and there is an oxygen deficiency in the heart. This causes sudden sharp or dull pain in the chest area. Typically, a strong feeling of tightness in the chest occurs at the same time, which causes additional shortness of breath. If the coronary heart disease intensifies, the angina pectoris attacks occur even with less stress. In particularly severe stages, complaints at rest are also possible. An increase in pain and tightness with each attack also suggests that the disease is progressing. If the symptoms do not change over time, this tends to indicate stable angina pectoris, in which the disease does not progress.
Causes of Angina Pectoris
Angina pectoris (chest pain) is the main symptom of coronary heart disease (CHD), a disease in which the coronary arteries become increasingly clogged due to arteriosclerosis (calcification of the arteries) and thus become narrower. These narrowings limit blood flow to the heart and are known as coronary stenoses. The poor blood circulation results in a disproportion between the heart's need for oxygen and the supply of oxygen; this fact is called coronary insufficiency in technical terms. You will also find an overview of the main factors in angina pectoris, which will then be discussed in more detail.
- Arteriosclerosis and increased blood lipid levels
- stress
- high blood pressure
- Psychosomatic causes
- Cold as a risk factor
- Other possible causes
You can also find more information on this topic here: Causes of Angina Pectoris
arteriosclerosis
So the cause of angina pectoris is arteriosclerosis. In arteriosclerosis, the risk factors mentioned below lead to damage to the endothelium, the innermost layer that lines the arterial wall. The endothelial damage changes the properties of the arterial wall:
Blood components can now stick to the vessel wall more easily. In addition, messenger substances are released that mediate inflammation and tissue growth.
This leads to an inflammatory process and tissue growth in the arterial wall; in addition, various cell types and fats are deposited in the affected vessel wall. The deposit is known as a “fatty streak” and does not yet lead to any significant vasoconstriction.
Over the years, the deposits become larger and larger and built into the vessel wall under a cell cap.
The diameter of the artery is now significantly reduced, and the affected vessel can no longer expand if necessary. If there is now an increased need for oxygen, as is the case with physical exertion, the heart does not get enough oxygen due to the poor circulation, which manifests itself in angina pectoris.
The risk factors for hardening of the arteries therefore largely correspond to the risks for angina pectoris. The main causes of arteriosclerosis are increased blood lipid levels, arterial high blood pressure, diabetes mellitus, smoking and an age over 45 years for men and 55 years for women.
Other risk factors for calcification of the arteries are sedentary lifestyle, obesity and metabolic disorders of fat and sugar regulation.
You may also be interested in this topic: Atheromatosis
Stress as a cause
Stress is a very big risk factor for all types of heart disease. Regardless of whether the stress has physical or psychological causes, it has an equally negative effect on the cardiovascular system. The hormone cortisol, which is increasingly released during stress, leads to an increased production of vascular-damaging molecules. Cortisol leads to increased fat deposits on the blood vessel walls. Over time, plaques and calcifications develop from the deposits, which narrow the vessels. If such a deposit takes place in the coronary arteries, it can quickly lead to an undersupply of the underlying heart muscles, which causes angina pectoris symptoms.
You might also be interested in this topic: Ways to reduce stress
High blood pressure as a cause
For many people, high blood pressure is responsible for the development of diseases of the cardiovascular system. It will cause a faster blood flow in the vessels, whereby greater forces act on the vessel walls, which favors the formation of arteriosclerotic plaques. In addition, the increased blood pressure creates many small eddies in the blood flow, which in turn means that greater forces act on the vessel walls. On the other hand, this turbulence can cause cells from the blood to settle on the plaques. This makes the constricting calcifications on the vessel walls larger. The more plaques there are in the coronary arteries, the poorer the blood flow, which can lead to angina pectoris.
Find out more about this: Therapy of high blood pressure
Psychosomatic causes
Psychosomatic causes are psychological factors that have an influence on the development of physical (= somatic) diseases. In angina pectoris, psychological stress plays a major role. It leads to the release of the stress hormone cortisol, which accelerates the production of vascular damaging substances. These harmful substances lead to the increased formation of plaques in the coronary arteries, which promotes the development of angina pectoris. Conversely, a heart disease (somatic = physical illness) can also have an impact on the psyche. Angina pectoris attacks often trigger fear and panic in those affected. This fear also falls under the concept of psychosomatics, since here psyche and body interact with one another.
Cold as the cause
Cold is a major risk factor for angina pectoris attacks, especially in winter. Due to the low temperatures, the blood vessels on the surface of the skin contract. This mechanism is intended to ensure that as little heat as possible reaches the surface. However, the contraction of the blood vessels results in increased resistance in these vessels. The heart has to pump against this resistance and therefore increases the blood pressure.To maintain the higher blood pressure, increased work of the heart is necessary, which in turn requires an improved blood supply to the heart muscles. Due to the constrictions in the coronary arteries, however, increased blood flow is not possible, which is why there is an insufficient supply of the heart tissue. This triggers angina pectoris complaints.
Classification
Angina pectoris is divided into the following forms:
- Stable angina pectoris
- Unstable angina pectoris
- Prinzmetal angina
- Angina decubitus
- Other forms such as stress angina or pre-infarct angina
There are also different degrees of severity (CCS classification CanadianCardiovascularsociety):
- 0: silent angina pectoris, more of an incidental finding
- 1: AP symptoms only occur during the heaviest physical exertion (shoveling snow, heavy gardening)
- 2: AP symptoms occur easily with normal to heavy physical exertion (e.g. climbing stairs quickly)
- 3: AP symptoms are more pronounced with normal physical exertion
- 4: AP symptoms even with the slightest physical exertion (e.g. severe pain while getting dressed) or at rest
Stable angina pectoris
90% of the cases of stable angina pectoris are narrowing of at least one of the coronary arteries. It is characterized by the fact that the symptoms always occur with the same loads and always subside through the same countermeasures. Countermeasures include rest and medication.
Unstable angina pectoris
Unstable angina pectoris is first of all any new angina pectoris that occurs or any change in symptoms of stable angina pectoris. If the seizures e.g. occur even with less stress or at rest, or the seizures occur more frequently or if the pain persists despite taking medication, one speaks of unstable angina pectoris. Usually this is due to a narrowing of several coronary arteries or a narrowing of a larger coronary artery (Often a so-called left-sided main trunk stenosis). The unstable angina pectoris carries a very high risk of heart attack. Therefore, patients with unstable angina pectoris need immediate medical attention.
Prinzmetal angina
Prinzmetal's angina (Angina pectoris) got its name from the person who first described it, Myron Prinzmetal (1908 - 1987). He described the disease for the first time in 1959 as a special form of angina pectoris. Here, the heart is not supplied with insufficient oxygen due to a narrowing but due to a so-called vasospasm. This is a spasm of one or more coronary arteries that causes the vessels to narrow. The cause of the cramps is still unclear. A connection with the parasympathetic nervous system is suspected. This is a part of the vegetative (involuntary) nervous system that is responsible for all things like digestion (Parasympathetic nervous system) or flight reflexes (sympathetic nervous system). Prinzmetal's angina occurs completely independently of stress. But rather in the early morning hours, since this is the time when the parasympathetic nervous system is most active. It is typical for Prinzmetal's angina that it occurs as early as the 3rd to 4th decade of life. Like the other forms of angina pectoris, it can cause a heart attack.
Angina decubitus (angina nocturna)
This form of angina pectoris occurs mainly at night or after lying down for a long time. It is a form of unstable angina pectoris. When lying down, there is an increased return flow of venous blood into the heart. If the heart muscle cells are previously damaged, this is the trigger for angina decubitus / nocturna.
Other forms
Occasionally one hears or reads other names for angina pectoris. However, these terms are only synonyms or other terms for the forms of angina pectoris described above. E.g. An angina of exertion is only a description that the angina pectoris occurs only under exertion. (So at least a degree of severity 1). Pre-infarct angina is also used more frequently. This describes angina pectoris that occurred before a heart attack and thus probably caused it. Therapy-resistant angina pectoris describes a severe form of unstable angina pectoris that cannot be treated or is difficult to treat.
What is an angina attack?
Angina pectoris describes pain and a feeling of tightness / pressure in the chest. These symptoms are usually not permanent. Rather, they occur like attacks in certain situations. Possible triggers include physical activity and psychological stress, as both situations increase the body's need for oxygen. Such an attack of angina pectoris usually occurs suddenly and usually lasts one to five minutes. During the attack, those affected suffer from sharp stabbing or pressing pain in the chest area. Back, jaw or abdominal pain can also occur. In addition, the tightness in the chest usually makes breathing difficult, which can trigger fear and panic. The symptoms subside after a few minutes. In the acute situation of an angina pectoris attack, the administration of nitroglycerin can alleviate the symptoms. It is usually administered in the form of a nitro spray. However, an accurate diagnosis of the heart disease must be performed before this drug is prescribed. Due to the sudden onset of symptoms, an angina pectoris attack can also be mistaken for a heart attack. Therefore, a cardiologist (heart specialist) should be consulted with anginal complaints.
Are you more interested in this topic? For detailed information, see: Angina pectoris attack
How likely is angina pectoris to lead to a heart attack?
The connection between angina pectoris and myocardial infarction is clear: Both diseases are based on coronary heart disease. While an angina pectoris attack results in a short-term inadequate blood flow to the heart muscles due to a narrowing of the coronary arteries, a heart attack is caused by the sudden complete closure of such a vessel. The transition between the two diseases is fluid. The higher the degree of stenosis (a distinction is made between 25%, 50%, 75% and 100% stenosis), the more severe the angina pectoris symptoms and the more likely it is to have a heart attack. The situations in which the angina occurs are also determined by the severity of the disease. While in stage I only heavy physical exertion leads to a seizure, in stage IV the symptoms occur at rest. The risk of myocardial infarction in a person affected in stage IV is many times higher than the risk in stage I. A further risk assessment is based on the division into stable and unstable angina pectoris. With stable angina, the risk of heart attack is low because the disease does not progress. In the case of unstable angina pectoris, on the other hand, the risk is significantly increased as the coronary artery disease becomes increasingly severe.
Is angina contagious?
Angina pectoris is not a contagious disease. The disease develops exclusively in the blood vessels of the affected person. There are many reasons for this, but they lie exclusively in the body of the person affected. Coronary heart disease, which triggers angina pectoris, only occurs through many metabolic processes. In contrast to infectious diseases, there is no pathogen that can be transmitted from one person to the next. However, angina pectoris can be inherited. Although not every descendant of affected people gets angina pectoris, the risk of developing heart disease is significantly increased. The reason for this lies in a genetic predisposition that favors the development of coronary heart disease.
therapy
The therapy of angina pectoris is divided into different areas. This includes symptomatic therapy during an acute angina pectoris attack, long-term drug therapy and the reopening of narrowed vascular segments (revascularization). Possible measures are listed below and then explained in more detail.
- Nitro spray
- Medical therapy
- Use of a stent
- Bypass surgery
- homeopathy
In the case of an acute attack of angina pectoris, the patient is given one or two sprays of nitroglycerin spray under the tongue, which can relieve the symptoms in a few minutes.
Caution is advised when taking sexual enhancers such as Viagra at the same time: The combination of both drugs can lead to a life-threatening drop in blood pressure.
Long-term therapy is intended to prevent further attacks of angina pectoris and delay the progression of the disease. The most important measures to be mentioned are a healthy lifestyle: quitting smoking, weight reduction and regular light endurance training, for example in cardiac sports groups.
In addition, existing high blood pressure, diabetes mellitus and increased blood lipid levels should be treated. These basic measures are supported by drugs that, depending on the active ingredient contained, improve the oxygen supply to the heart or reduce the heart's need for oxygen.
Cardiologists perform interventional balloon dilatation (PTCA) using a minimally invasive technique for severe constrictions over 50% of the diameter in a coronary artery. Usually a stent is then implanted, which keeps the lumen of the coronary artery open.
The mortality of the procedure is 0.5% in patients with stable angina pectoris. The success rate of this procedure is very high at up to 95%, but the implanted stent closes in up to 40% of patients in the first six months and thus triggers new angina pectoris.
Patients must take anticoagulants for up to a year to prevent stent obstruction.
In the case of severe narrowing of several coronary vessels or the main vessel, a bypass operation is performed in cardiac surgery. Here, the narrowed vessel sections are bypassed by implanting a vein or artery of the patient. Mostly the great saphenous vein or the internal mammary artery is used.
The mortality of this intervention is 1-3% with stable angina pectoris; the operation reduces the mortality rate within the first five years in comparison to drug treatment in patients with multiple affected vessels by 30%. The success rate is high with 80% symptom-free patients after the operation, venous bypasses close in 30% of cases after five years, arterial bypasses close much less often.
Read more about this topic on our subpage: Therapy of angina pectoris
Nitro spray
The nitrospray is the typical emergency medication for people suffering from angina pectoris. The nitroglycerin contained in the nitrospray releases nitrogen monoxide (chemical formula: NO) in the body. This acts on the smooth muscle cells of the vessels and leads to relaxation there. This causes the vessels to expand. By inhaling the nitro spray, it gets directly into the lungs, from where it is transported with the blood flow directly into the heart, where it causes the coronary vessels to dilate (vasodilatation). This vascular dilatation leads to a significantly improved blood flow to the heart muscles within a very short time and thus alleviates the angina pectoris attack.
Medical therapy
The acute therapy consists of the administration of one to two strokes of nitroglycerin spray and anticoagulants (heparin and ASA). If necessary, oxygen and strong pain relievers (morphine) can also be administered.
Long-term drug therapy includes the treatment of the underlying coronary heart disease. It should consist of ASA, a beta blocker, a statin and an ACE inhibitor or aldosterone antagonist. These drugs improve the prognosis of CHD and lower the death rate. ASA (aspirin) is an anticoagulant that inhibits blood platelets and thus reduces the attachment of these cells to endothelial damage.
Beta blockers are actually drugs used to treat high blood pressure and prevent attacks of angina pectoris. Statins have a regulating effect on lipid metabolism and lower the LDL cholesterol level, which means that less cholesterol is built into the blood vessel walls. ACE inhibitors lower blood pressure and thus reduce the heart's need for oxygen. They also inhibit what is known as remodeling in the heart, a process in which the heart muscle tissue is pathologically changed as a result of CHD. Aldosterone antagonists belong to the group of diuretics (water-driving agents) and also counteract these remodeling processes.
When do you need a stent?
The stent is a small wire mesh that can be inserted into a narrowed coronary artery. The stent is placed in the vessel using a catheter. There he should keep the vessel open and thus prevent angina pectoris attacks. The decision to use a stent depends on the patient's symptoms. The greater the level of suffering, the more likely one will resort to a stent. Vascular narrowing is considered critical when more than 50% of the vessel is blocked. Therefore, a stent is used from a degree of stenosis of around 50%.
You can find everything about the topic here: Stent
When do you need bypass surgery?
Bypass is a method that can be used to bypass clogged or severely restricted vessels. An endogenous vessel (often a piece of a leg vein) is removed and sewn to the heart in such a way that the blood flow is diverted around the blocked area. Since bypass surgery is a larger procedure than inserting a stent, bypasses are usually only used when the stent fails or the insertion of a stent is not possible. Bypass surgery is also not performed on every patient with angina pectoris. The decision for the bypass depends on the severity of the symptoms.
More on this topic: Cardiac bypass - when is it used?
homeopathy
Homeopathy plays an important role in the treatment of many diseases in addition to the drugs used in conventional medicine. Homeopathic gold drops are particularly useful for angina pectoris. Arnica and Pulsatilla are also used. Medicinal plants that help with angina pectoris complaints are skullcap and sage leaves. The homeopathic treatment also includes changing the diet from animal fats to a high-fiber and balanced diet. Green vegetables and nuts are particularly valuable here. Since homeopathic remedies can interact with classic medications, the use of such remedies should be indicated to the doctor.
Which sports are beneficial for angina pectoris?
In angina pectoris, excessive physical exertion often leads to an acute attack, so exercise should be started very slowly. In addition, it is essential to discuss with the attending physician which training intensity is allowed. There are specialized cardiac sports groups for safe entry into sport. With angina pectoris, sports that train endurance are particularly beneficial. A good start to such a workout is taking regular walks. The body can slowly get used to physical strain. Later on, jogging, cycling, hiking, walking and swimming are all suitable. These endurance sports strengthen the heart and breathing, they also promote muscle building and general physical fitness without suddenly putting the heart under stress.
EKG
To diagnose a Lack of oxygen in the heart muscle becomes a Exercise ECG performed on the bicycle ergometer. The patient gradually becomes one increasing physical exertion suspended while the doctor is watching the EKG.
Are typical of a lack of oxygen Lowering of the ST segment of at least 0.1mV in the Limb leads or one Elevation of the ST segment of at least 0.1mV in Leads without a Q wave.
The maximum physical load is applied to the Age of the patient customized. The meaningfulness of an exercise ECG is greater, the higher the Ergometer load and that achieved Heart rate are. If the maximum load is not reached, are 20% the normal ECG results false negative and a narrowing of the vessels in the heart is overlooked.
But also false positives are in up to 50% of the cases possible, these findings are then identified as incorrect by further examinations. The risk of a Exercise EKGs is minimal due to constant monitoring, but should always be carried out under medical supervision due to the possible complications of the heart.
physiology
The heart is supplied with oxygen via its coronary arteries. The main artery (aorta) connects directly to the valve of the left ventricle. The coronary arteries branch off from the aorta directly behind the valve. The heart reacts to a lack of oxygen faster than other organs with pain (see: heart pain). This is a very good warning system, as angina pectoris can be life-threatening if left untreated. In both unstable and stable angina pectoris there is a narrowing (stenosis) in the coronary arteries. Depending on the severity, this now ensures insufficient supply from certain loads.
Summary
The most common symptoms of angina pectoris are:
- Sudden onset of chest pain felt behind the breastbone (retrosternal), also "tear" in the chest
- Radiation of the pain to the shoulders (more likely the left), back and jaw
- heartburn
Women usually experience slightly different symptoms. Most of them are more likely to report back pain or stomach pain.
All symptoms do not always have to appear, or any symptoms at all (e.g. with so-called silent AP). Also, diabetics or patients with polyneuropathy usually feel no pain at all or only a little pain which is then not taken seriously.
One of the main causes of angina pectoris is vascular calcification (arteriosclerosis). Stress in any form and physical strain can also trigger a seizure and are a cause. Lush meals can irritate the heart to the point of an attack of angina pectoris. This is due to the proximity of the esophagus and heart. Cold or general weather changes can act as a trigger. When it's cold, the heart has to beat harder to warm the body, which is stress for the heart. Excessive consumption of alcohol and smoking cause arteriosclerosis and are therefore causes, at the same time both can directly trigger angina pectoris. For example, smoking has a vasoconstricting effect and thereby further cuts off the oxygen supply to the heart. Alcohol works the same way.
In summary, one can say that all activities or circumstances that increase the pulse and blood pressure are stress for the heart and can thus acutely trigger an angina pectoris attack. The same factors can then permanently damage the heart and thus have a causal effect. The more “stressed” the heart, the more oxygen it needs and the worse the symptoms become.