Antibiotics while breastfeeding
introduction
Many mothers take medication while breastfeeding. These are often antibiotics as well. In such an application, precise considerations must be made. Medicines can be excreted in breast milk and thus absorbed by the infant.
This problem can be exacerbated if the infant's liver is not yet fully detoxifying. On the other hand, treatments with antibiotics are often useful and protect mother and baby from serious infectious diseases.
Read more about this under: Medication during breastfeeding

Indications of antibiotics in pregnancy or breastfeeding
In principle, the indications for antibiotics during breastfeeding do not change. Antibiotics are the first choice for many bacterial diseases. These range from urinary tract infections to pneumonia.
However, certain bacterial diseases can occur more frequently during breastfeeding and require treatment.
An example of this is puerperal mastitis, an inflammation of the glandular tissue of the breast.
It can be triggered by bacteria and, in this case, treated with antibiotics.
There can be big differences in the choice of antibiotics during breastfeeding. Not all antibiotics are considered completely safe.
Read more on the subject under: Puerperal mastitis
Which antibiotics are allowed during breastfeeding?
With many drugs it is very difficult to prove that they cannot have any harmful effects.
Studies on nursing mothers or pregnant women are strictly regulated for good reason.
With certain antibiotics, however, we have years of experience in their use during pregnancy. These antibiotics are considered to be lower risk substances.
Penicillins and related substances, as well as cephalosporins, are considered to be particularly effective. Penicillins are among the oldest known antibiotics. Their use has therefore been tried and tested for years during pregnancy and breastfeeding.
Other proven agents are erythromycin and azithromycin. Second-line drugs are clindamycin, metronidazole, and certain carbapenems. They are also among the lower-risk substances, but there is less experience with their use.
In addition, substances that have to be taken as rarely as possible, for example only once a day, can be advantageous. The type of administration is also important. Many antibiotics are taken as tablets. However, there are also antibiotic eye drops, for example.
These are usually harmless as they are only absorbed by the body in very small quantities.
If in doubt, a doctor or pharmacist should always be consulted.
In addition, large databases have been created in which drugs are listed according to their risk potential for the child.
Many of these databases can also be viewed on the Internet.
Read more on the subject under: Antibiotics
Which antibiotics are contraindicated during breastfeeding?
Not all antibiotics can be used safely during breastfeeding. Above all, substances that have shown an increased risk for the child in animal experiments are only used under strict control. In addition, there is often insufficient experience for use in humans.
For some antibiotics, better tested alternatives are therefore recommended.
Examples of antibiotics that should be used hesitantly are co-trimoxazole or fluoroquinolones.
If there is no tried-and-tested alternative, these medications can also be taken while breastfeeding.
Drugs that have been tried and tested are still preferable. The use of tetracyclines and aminoglycosides should also be carefully considered.
If there is a proven alternative, this should be preferred in any case. If in doubt, a doctor or pharmacist should always be consulted. Databases facilitate the control of a specific drug.
Read more on the topic: Tetracycline
What are the consequences of taking antibiotics for my baby?
Many antibiotics taken during breastfeeding have only a very mild, often imperceptible, effect on the baby.
This is especially true for proven antibiotics, which are classified as rather harmless.
The consequences for the infant depend on several factors. Not all drugs end up in the same amount in breast milk and thus in the infant's diet. The time, frequency and amount of intake are also important for this.
In addition, the metabolism of a child can differ from that of an adult. The liver, in particular, may not be fully developed in its work. It fulfills important detoxification functions and is central to the metabolism of many antibiotics. As a result, the breakdown of many antibiotics in infants is often different than in adults.
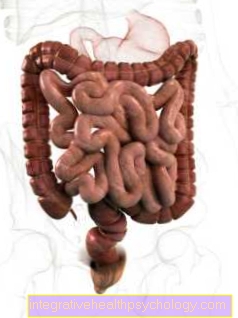
One of the most common adverse effects of antibiotics on babies is thinning stools and, rarely, diarrhea. However, this occurs relatively rarely and is usually only temporary. Antibiotics that are excreted in breast milk first reach the child's intestines. This means that they can have an impact on the child's intestinal flora.
In the first few months in particular, the intestinal flora is not yet fully developed and only develops slowly. There is evidence that a disruption of the child's intestinal flora can lead to health problems later in the child's life.
An increased BMI, i.e. a trend towards obesity, has already been observed.
Some antibiotics are known to be harmful to children. For example, antibiotics from the group of fluoroquinolones can cause cartilage damage, while gentamicin is suspected of damaging the ears. However, this applies to the direct intake of the antibiotic by the child. However, both drugs are only excreted in breast milk in very small amounts, so that side effects of this kind are almost impossible.
In principle, these drugs can therefore also be taken by the mother during breastfeeding. However, an even more precise risk assessment should be carried out here than already.
Read more on the subject under: Gut flora
Does the antibiotic pass into breast milk?
At least traces of any medication ingested can get into breast milk.
However, there are major differences in the amounts in which this can be done.
Two factors are particularly important for this.
- The first factor is the plasma concentration of the unbound antibiotic in the maternal blood. This depends on the time of ingestion, the amount administered and ingested, the metabolism and excretion of the drug. Not all antibiotics swim around freely in the blood. Often they are only bound to the body's own proteins, which makes it even more difficult to get into breast milk.
- The second factor is the nature of the antibiotic itself. While smaller molecules get into breast milk more easily, larger molecules are more about fat solubility. As a rule, only a very small proportion of the antibiotic ingested passes into breast milk.
For penicillin G, the relative dose, that is to say the proportion of the daily dose taken by the mother by the infant, is given as less than 1%, for example.
Antibiotics for a cystitis
Bladder infections are a common use for antibiotics. It is not always necessary to take antibiotics. A purely symptomatic treatment by the doctor can be recommended, especially in the case of mild symptoms, without fever or absence of signs of a serious illness. However, this is not always enough.
If antibiotics are used to treat cystitis during breastfeeding, penicillins, for example, are recommended, as they are also used in non-breastfeeding adults.
Read more on the subject under: Cystitis in pregnancy
Antibiotics for tooth inflammation
Tooth inflammation should be treated promptly. This may require taking an antibiotic. Here, too, antibiotics from the group of penicillins are a means of choice.
Most penicillins, such as the widely used amoxicillin, are among the tried and tested antibiotics during breastfeeding.
However, antibiosis is often not absolutely necessary. If in doubt, the dentist should therefore be informed about breastfeeding.
This enables him to plan further therapy better.
Read more about the topic under: Inflammation of the gums
Antibiotics for bronchitis
Acute bronchitis is inflammation of the bronchi, the airways in the lungs. The majority of acute bronchitis is caused by viral pathogens.
Since antibiotics do not have a sufficient effect against viruses, administration is also not advisable.
Bacterial infections mainly occur with a pre-existing, mostly known disease of the lungs. If bronchitis is caused by bacteria, the choice of antibiotic depends primarily on the pathogen.
Some pathogens causing bacterial bronchitis require the use of special antibiotics such as clarithromycin.
This can be used during breastfeeding if there is a medical benefit.
Read more on the subject under: Bronchitis
Antibiotics for tonsillitis
Another common use of antibiotics is in the treatment of angina or tonsillitis.
Here, too, it is true that not all tonsillitis or diseases perceived as such need to be treated with antibiotics.
Acute tonsillitis, in particular, can be caused by viruses. In this case, antibiosis is usually not useful. However, antibiotics are often used, especially after a bacterial infection has been detected. Usually it is a drug from the group of penicillins or cephalorsporins. Both groups have been tried and tested in breastfeeding and are used as the first choice.
Read more on the subject under: tonsillitis
Antibiotics for otitis media
An otitis media often occurs following a respiratory infection.
The basic therapy consists mainly of basic measures like drinking a lot and pain therapy. So antibiosis is not always necessary.
However, antibiotics are often useful, especially in serious or complicated cases, and prevent serious consequential damage. Amoxicillin is also the agent of choice in the treatment of otitis media.
It is considered to be well-tested and is a drug of choice during breastfeeding.
Read more on the subject under: otitis media
Antibiotics for breast infections
Inflammation of the breast can also occur during breastfeeding. Inflammation of the mammary glands that occurs during breastfeeding is known as purpuerperal mastitis.
Here, too, the focus is initially on basic measures. These include regular emptying of the breast with subsequent cooling or pain relievers. Antibiosis may be necessary, especially if the breast infection has persisted for more than two days.
Penicillins or cephalosporins are again the drugs of choice during pregnancy.
Read more about this under: Breast inflammation
Antibiotics for borreliosis
Lyme disease, often simply referred to as borreliosis, is a complex and long-term disease. It is caused by bacteria from the so-called Borrelia burgdorferi complex.
The disease usually runs in several phases. Different treatment may be necessary depending on the phase. Especially at the beginning of Lyme disease, amoxciillin can be given as a well-tested drug for breastfeeding.
Other antibiotics are also used in later stages. An example of this are cephalosporins. They are also considered well-proven means for breastfeeding.
Alternatively, it may be necessary to take doxycycline.
In principle, it is possible to continue breastfeeding while taking doxycycline.In general, Lyme disease is a serious disease that should be treated by a doctor.
Read more on the subject under: Lyme disease