Effects of back pain on the psyche
Synonyms
English: Low back pain
Lumbargia, lumbago, lower back pain, lumbar syndrome, lumbar root irritation syndrome, compression syndrome, lumbar intervertebral disc syndrome, sciatica, sciatica, lumbar sciatica, sciatica, facet syndrome, vertebral joint pain, myofascial syndrome, tendloomygenic reflex syndrome, spinal syndrome
definition
Chronic back pain is an ongoing and growing problem in our society. One can even now speak of a “widespread disease”, since chronic back pain leads to very frequent visits to the doctor, absenteeism at work and, ultimately, immense costs.
The reasons for chronic back pain can be many. Often organic causes can be found, which are mostly responsible for acute and often also for chronic back pain.

But what about the many patients for whom no findings can be made that could explain the intensity and duration of the perceived pain?
Medicine today assumes that the psyche plays a decisive role in the majority of pain patients. However, this means By no means that pain patients are mentally ill per se, that they imagine pain or Are simulants. Today's understanding of pain should be body and Unite psyche.
introduction
Classification of the causes of chronic back pain according to the WHO:
- physical causes - "impairment"
- subjective impairment - "disability"
- social level - "handicap"
- physical causes - "impairment"
The physical causes for the development of chronic back pain can be extremely diverse. Damage to the spine, its joints and ligaments and inflammatory processes are just as conceivable as, for example, tumor diseases or damage to other organs that "radiate" into the back. A majority of these causes can now be identified or excluded with diagnostic methods. What you cannot do, however, is to draw a direct conclusion on the pain perception from the findings.
- subjective impairment - "disability"
The central point here is the question: "What does the pain do to the patient and how does the patient deal with it?" Everyone knows pain and everyone knows that pain can influence our behavior. Since pain patients have to deal with this mechanism of cause and effect on a permanent basis, behavior and, in addition, the whole lifestyle can change. Pain patients run the risk of getting caught in a “vicious circle” that arises from this very mechanism.
Example:
Pain in the back leads to relief. Resting can lead to "fearful" behavior, since rest and caution promise freedom from pain. Anxiety, on the other hand, often leads to retreat. Retreat leads to loneliness and sadness, and in the end it can lead to depression. Depression, in turn, increases pain.Of course, this mechanism does not work for everyone. It has been found that certain personality traits are crucial for the development of such a vicious circle.
- The social level - "handicap"
The so-called "social environment" that surrounds us is made up of the people, but also the institutions that we deal with on a daily basis and that shape our lives. Now the social environment in this country has its peculiarities with certain groups, such as Dealing with sick people. Dealing with the sick is by no means always the same.
A person who breaks a leg while skiing is viewed differently than someone who suffers from schizophrenia, for example. This handling now also has a clear influence on the course of the disease. (E.g. a depressed patient will suffer significantly more if he is excluded because of his illness.).
In the same way, there are also factors with regard to patients with chronic back pain which one has to believe that they exacerbate the pain and thus “make it chronic”. E.g. If the patient is hurt by his environment, for example by accusing him of being a simulant, the symptoms will worsen.
You might also be interested in this topic: Psychosomatic back pain
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Differential diagnoses
The main disturbances to be mentioned here are:
- Somatization disorder
- Hypochondriac disorder
- schizophrenia
- depression
With all of these diagnoses, increased pain (also in the back) is conceivable.
Comorbidity
The diagnosis of chronic back pain is often associated with other psychosomatic disorders on the therapeutic side. The most common additional disorder is depression. The second most common are panic disorder / panic attack or agoraphobia. Only then should the somatoform disorders be mentioned.
In a large number of pain patients, pain medication abuse develops over time.
Diagnosis
Pain is very subjective. Nevertheless, it is possible to make pain a little more tangible by using various diagnostic instruments before and during a possible therapy.
- Pain Diary:
All important information for the therapist is recorded by the patient over a defined period of time (e.g. one week).
E.g. Frequency, severity and duration of pain, frequency of medication use, activities before pain, etc. - Pain Sensation Scale (SES)
The pain perception scale tries to capture the psychological changes in the patient that are caused by the pain. It is also a good tool during therapy to record progress.
- Tübinger sheet for the assessment of pain behavior (TBS):
This is a questionnaire in which relatives of the pain patient are asked how they experience the patient and how they deal with the pain.
- Functional questionnaire Hanover (FFbH-R):
This questionnaire primarily records the life constraints that the patient suffers from the pain.
therapy
Therapy of chronic back pain:
Nowadays, the treatment of chronic back pain typically takes place in several stages.
- Level: Teaching the model of disease development from a psychological point of view
The understanding of the interaction of body and soul in the creation, processing and maintenance is the basis of a successful therapy. Here it is the most important task of the therapist to explain and convey this model appropriately.
- Level: Progressive muscle relaxation
Pain creates tension. For this reason, learning and performing relaxation exercises is an important step in therapy. Progressive muscle relaxation has proven to be particularly helpful because it is easy to learn.
- Stage: Keeping minutes
Another important step is to log events, situations and thoughts that are directly related to the pain. The aim here is on the one hand to identify typical pain-triggering or pain-intensifying situations and on the other hand to make the pain more understandable as a problem, which is sometimes better and sometimes worse.
- Level: Recognizing and processing typical thoughts
In the fourth stage, the typical thoughts associated with the pain are processed. E.g. Thoughts that express one's own helplessness and which are possibly negative beyond the normal level are considered (“I can no longer practice any of my hobbies and only the pain is to blame!) and processed. The technology that is used here is called "cognitive restructuring".
- Distraction and enjoyment level
Pain and pleasure are usually two things that can only be easily reconciled with a few people. One stage of the therapy thus deals with the "training of enjoyment experience". The goal here can actually be a distraction from the pain, on the one hand, but also the realization that it is possible for a patient to have positive experiences despite pain and to consciously bring them about.
- Stage: Identifying causes that aggravate or maintain the pain
The primary concern here is recognizing conflicts in the patient's life. The prerequisite for this is a good relationship between therapist and patient. It's not about looking for the one scapegoat who is to blame for everything. Rather, today's understanding of pain assumes that conflicts are part of the problem and therefore dealing with them can be part of the healing process.
- Stage: The search for ways out of pain
This stage is about concrete possibilities for the patient to deal with findings from the therapy. Conflicts that are now "visible" can be dealt with in concrete terms. Such processing has e.g. the so-called "training of social competence" is recommended.
- Stage: hypnosis
In the therapy of chronic back pain, hypnosis can do two things in particular. On the one hand, it is a procedure that, when used correctly, can have a pain-relieving effect and, on the other hand, it allows better access to the "unconscious".
You can find a list of contacts with certified pain therapists in the appendix to our book “The unrecognized suffering - Chronic back pain and psychotherapy”.
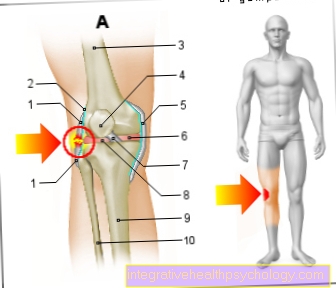
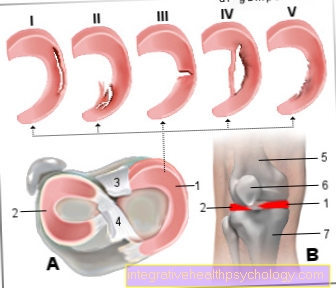
Figure back pain

A - neck pain
B - upper back pain
C - lumbar spine pain
Lumbago (lumbago)
D - lumboglutealgia
(Radiating into the buttocks)
E - Lumboischialgia
(Radiating into the leg)
- First cervical vertebra (carrier) -
Atlas - Seventh cervical vertebra -
Vertebra prominent - Trapezius -
Trapezius muscle - Broad back muscle -
Muscle latissimus dorsi - First lumbar vertebra -
Vertebra lumbalis I - Fifth lumbar vertebra -
Vertebra lumbalis V - Sacrum - Sacrum
- Tailbone - Os soccygis
- Iliac crest -
Iliac crest - Gluteus Middle -
Muscle gluteus medius - Gluteus Muscle -
Muscle gluteus maximus - Big Dresser -
Adductor magnus muscle - Two-headed hamstrings -
Biceps femoris muscle
a - Disc prolapse -
Nucleus pulposus prolapse (from above)
b - vertebral fracture
(Vertebral fracture)
c - spinal osteoarthritis -
(Joint wear)
You can find an overview of all Dr-Gumpert images at: medical illustrations




.jpg)