Blood transfusion
definition
A blood transfusion is the administration of blood or blood components via a vein. The blood used for this is taken from a donor when the blood is donated.

While blood was previously given without dividing it into its components, this so-called “whole blood” is now separated first. This creates 3 parts: Red blood cells, Platelets and the remaining liquid, that Blood plasma. The separation makes it possible to give a patient only the blood component that he needs. Among other things, this reduces the risk of side effects.
What are the reasons for a blood transfusion?
The administration of a blood transfusion is indicated in:
-
Blood loss (acute or chronic) e.g. from surgery or trauma
-
Anemia (anemia)
-
Bleeding disorders
-
Thrombocytopenia (Platelet deficiency)
In the case of blood coagulation disorders, in contrast to anemia, no red cell concentrates are administered, but the coagulation factors are substituted. Thrombocytopenia is a lack of blood platelets. In this case, platelet concentrates are given. In any case, the blood groups of the donor and the recipient must be compatible.
Reasons for a blood transfusion
The human body basically needs a certain amount of blood in order to function. Without enough blood, ours can Cells not supplied enough oxygen become, additionally collect toxic breakdown products on - this ultimately leads to death. We lose a large amount of blood or if certain blood components are used up too much, part of them has to be passed through a Blood transfusion replaced become.
The reasons for blood transfusions are very diverse. For example, red blood cells are given in cases of anemia, also known as anemia. This often occurs after major operations (postoperative anemia) or serious accidents. Also diseases of the gastrointestinal tract, such as the Ulcerative colitis or various cancers like that leukemia can lead to anemia. Faulty currencies, Kidney disease, Clotting disorders, as well as diseases of the blood-forming system in the bone marrow also often lead to anemia.
Platelet concentrates are usually administered to a patient when the platelets, too Platelets called, the blood drops so much that it can bleed heavily. This is common with severe blood loss after one Accident, in disorders of blood formation in the context of leukemia Drug side effects, to Irradiation or with diseases of the kidneys.
The reason for the administration of blood plasma is usually a blood clotting disorder. This can occur in liver diseases, congenital diseases or autoimmune diseases.

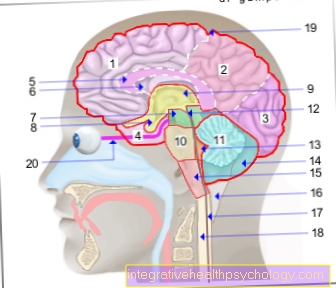
Blood - Sanguis
- Red blood cells
= red blood cells -
Erythrocytes - White blood cells
= white blood cells -
Leukocytes
2.1 - granulocyte
a - Basophils
b - Eosinophils
c - Neutrophils
2.2 - lymphocytes
2.3 - monocytes - Blood plasma
- Platelets -
Platelets - Oxygenated blood
(blue) - Oxygenated blood
(red) - Heart - Cor
You can find an overview of all Dr-Gumpert images at: medical illustrations
Blood transfusion for anemia
In anemia, also known as anemia, the level of hemoglobin in the blood is low. Hemoglobin is found in the red blood cells and is necessary to ensure that the cells are supplied with oxygen. If the concentration is too low, symptoms such as reduced performance, pale skin, dizziness or shortness of breath occur. Depending on the cause and extent of the anemia, it may need to be treated with a blood transfusion. Erythrocyte concentrates are then administered, i.e. a blood product that consists largely of red blood cells, because they contain the hemoglobin. If the anemia has to be treated with regular transfusions, there is a risk of iron overload. Red blood cells contain iron and release it when they break down. During transfusions, the body receives a large amount of it, but can only store a little. Iron is deposited in organs, where it can cause damage. This should be taken care of in the case of frequent blood transfusions, e.g. by iron chelators.
Blood transfusion in case of iron deficiency
Iron deficiency anemia is one of the most common deficiency diseases in the world. A deficit of iron in the body leads to decreased hemoglobin levels and thus to anemia. The most common cause of iron loss is chronic bleeding e.g. after surgery, trauma, bleeding from the gastrointestinal tract or menstrual bleeding. Therapy is usually carried out by giving iron supplements orally and stopping the source of bleeding. Blood transfusions usually do not need to be given. However, it may be needed if the bleeding is severe.
Blood transfusion for leukemia
The cancer of the precursor cells of our blood is called leukemia. Regardless of the type of leukemia a person is suffering from, blood formation is often so severely restricted as part of the disease that a blood transfusion has to be carried out. The reason for this is usually the migration of cancer cells into the bone marrow, where our blood is formed. If the cancer grows here uncontrollably, it displaces and destroys the healthy, blood-forming cells and thus causes anemia. With some forms of leukemia, such as "chronic lymphatic leukemia", it usually takes months or years before a deficiency of red blood cells, platelets or blood plasma develops. With other forms, however, things can happen very quickly: acute forms of leukemia can require a blood transfusion within days or weeks.
Read more on the topic: leukemia
In addition, chemotherapy is often necessary for leukemia. The drugs used here destroy rapidly growing cells - in addition to cancer cells, this also includes the healthy cells of the bone marrow that make up the blood. Therefore, a blood transfusion may also be necessary as part of the treatment. When a transfusion has to be carried out and which blood components are necessary is decided in the hospital based on the values from a blood sample.
Read more on the topic: chemotherapy
Blood transfusion for cancer
anemia is not a rare side effect in cancer patients. Especially tumors that affect the blood and the hematopoietic system, such as Leukemia are causes for this. However, other types of tumors can also contribute to anemia by attacking the bone marrow, increasing the breakdown of red blood cells or the release of inflammatory substances. The therapy of a tumor disease can also lead to anemia. Chemotherapy or radiation are aggressive procedures that do not leave the body without a trace. Blood transfusions cannot cure the cancer, but they can help the affected patient with the symptoms of anemia and thus restore quality of life. But here too there are risks. A blood transfusion is an additional burden on the immune system and in cancer patients who are already immunocompromised, the susceptibility to infection can increase. It must therefore be decided in each individual case whether a blood transfusion is useful for the patient or not.
Blood transfusion after chemotherapy
Chemotherapy is an aggressive therapeutic procedure that kills healthy cells in addition to the cells of a tumor. It is therefore also an enormous burden for the body. Since both the tumor disease and the chemotherapy can impair blood formation and thus also reduce the hemoglobin, it can be useful to give a blood transfusion both during and after chemotherapy . The transfusion does not cure, it only relieves the symptoms of anemia. However, especially after chemotherapy, the goal should be to bring the body's own functions, such as blood formation, back to a normal level. So you have to decide individually how useful a blood transfusion is.
Blood transfusion in the newborn
Anemia in the newborn is called fetal anemia. In this case, the children are often born very pale. Here, too, the cause is a lack of hemoglobin or red blood cells. This deficiency is often triggered by different Rhesus factors in mother and child, which means that the mother's immune system forms antibodies against the child's blood cells. Rhesus prophylaxis can prevent this. In severe cases, a blood transfusion is also necessary here. This can also be done in the womb by means of umbilical cord blood transfusion. A fatal course of fetal anemia is rare these days.
You might also be interested in this article: Rhesus intolerance
Blood transfusion after surgery
Blood transfusions are relatively often necessary during or after major operations.
The reason for this is usually the loss of blood during the operation or secondary bleeding on the part of the body that was operated on. Since mainly red blood cells are lost during a bleeding, so-called “erythrocyte concentrates” - concentrates from donated red blood cells - are usually used for the transfusion.
Before major operations in which greater blood loss is to be expected, blood supplies are usually provided in advance for safety. However, due to the risks associated with a blood transfusion, an attempt will first be made to replace the lost blood with fluids that contain saline (called infusions). Only when the blood loss is very great is the blood reserve used. An important decision factor is the hemoglobin value, which shows how much blood pigment is still in the blood: if it falls below a certain limit value, the patient must be given red cell concentrates.
After an operation, a blood transfusion is usually necessary if there is bleeding inside the surgical wound. This is often noticeable by a lot of blood in the bandage or in the drains, and sometimes only when symptoms of anemia, such as paleness or a fast heartbeat, occur.
Read more on the topic: Symptoms of anemia
How long does a blood transfusion take?
The duration of a blood transfusion may vary depending on required amount of blood, Previous illnesses of the patient and preferences of the attending physician vary in length. A blood bag contains approx. 250 ml of liquid. At the beginning, a small amount - approx. 20 ml - is usually transfused quickly. The flow rate is then reduced until the entire content has run into the blood. This takes approximately per can 45 minutes to 1 hour. As two or more packs of blood are usually given, the blood transfusion itself takes approx. 2 hours.
Should the blood be given on an outpatient basis - i.e. the patient comes to the hospital or a doctor's office, receives the blood transfusion and then leaves again - including preparation and monitoring after the administration of the blood products, they have to be approx. 4 hours for 500 ml of blood be planned.
A blood transfusion can temporarily worsen the general condition of people with heart failure or other serious pre-existing conditions if it is given too quickly. The reason for this is the sudden addition of blood that can stress the cardiovascular system.
How much blood is being transfused?
Blood transfusions are given in the form of donated blood. A blood supply contains approx. 300 ml of red blood cell concentrate. The amount of blood that is administered depends on the patient's hemoglobin level and to what level it is to be increased. One can roughly say that a blood reserve can increase the hemoglobin value by approx. 1 to 1.5 g / dl.
What are the risks of a blood transfusion?
The risk of serious side effects and complications during or after a blood transfusion is nowadays very low due to good control systems and extensive experience in the administration of blood products. The most common side effects include fever, allergic reaction, the Confusion of blood products and the resulting breakdown of blood cells that Infection with bacteria or viruses and the appearance of Lung waterthat breathing can worsen significantly.
A slight fever develops in about 0.1% of patients and is usually not dangerous. Allergic reactions to components of the donor blood are usually weak and occur in approx. 0.5% of cases. Confusion of blood reserves occurs in around one in 40,000 blood transfusions in Germany.The result can be the so-called “hemolytic transfusion reaction” - the breakdown of red blood cells. Symptoms such as fever, shortness of breath and pain in the back and chest, and in rare cases even circulatory problems with bleeding and organ failure can occur.
The risk that viruses get into the recipient's blood through a transfusion is particularly important for Hepatitis B., Hepatitis C. and HIV relevant. However, through strict controls, these viruses are transmitted in less than one in 1 million transfusions. Doctors try to minimize the risks mentioned by frequent monitoring of the patient and to quickly notice and treat side effects. As a result, serious consequences after a transfusion are extremely rare.
Blood transfusion complications
Complications are very rare during or after a blood transfusion. The reason for this is that, over the last few decades, better and better control systems have been developed that make blood products very safe in advance. In this way, many complications that occurred 30 years ago have been reduced to a minimum.
The most common serious complication that occurs today is the “haemolytic transfusion reaction”, which usually occurs after the blood supplies are mixed up. If the wrong blood group is transfused, the patient's red blood cells die and lead to fever, shortness of breath, nausea and pain, and sometimes to organ failure and severe bleeding. If the symptoms are recognized in good time, the disease can usually be well controlled.
Serious infections with high fever, drop in blood pressure and organ failure due to blood products infected with bacteria occur very rarely. Another serious complication is the so-called "acute lung insufficiency", in which fluid gets into the lung tissue and can lead to shortness of breath.
Side effects of a blood transfusion
Due to legal guidelines and examinations, serious side effects and complications with a blood transfusion are rare. Not only are the donors asked about different risk factors, the blood is also tested for various pathogens such as HIV, hepatitis B and syphilis. In addition, of course, the blood group is determined. Despite these precautionary measures, side effects can occur. Slight complications that can occur despite having the right blood type are nausea, fever and chills, which will go away on their own after a while. On the one hand, serious side effects occur when the blood groups of the donor and recipient are not compatible with each other. The recipient's immune system reacts to the foreign components of the blood and thus leads to anaphylactic shock, cardiovascular complications and, in some cases, kidney failure. This situation is life-threatening and requires immediate treatment. Another serious side effect can occur if the blood contains pathogens such as HIV or hepatitis B viruses, which then transmit the disease to the blood recipient. Based on tests for these pathogens, the chance of an infection through blood transfusion in Germany is very low.
What are the long-term effects of a blood transfusion?
Not only can side effects and complications occur immediately after the donation of the foreign blood, there is also a risk for the recipient some time afterwards. On the one hand, despite examinations, there may be pathogens in the blood that later lead to diseases. This is especially dangerous in less developed countries, as not all important tests are always carried out here. Pathogens such as HIV or the hepatitis B virus can lead to serious illnesses and thus even become life-threatening. Since there are strict requirements and laws for blood transfusion in Germany, this is a very rare complication in this country. Another long-term consequence is an increased susceptibility to infection. During a blood transfusion, foreign tissue is added to the body. Even if the blood groups are compatible, it is initially viewed by the immune system as foreign, which represents an additional burden and thus increases the risk of infections. In rare cases, a transfusion leads to the formation of antibodies against components of the blood. A later transfusion can result in hypersensitivity reactions or a reduced effectiveness of the transfusion.
How high is the risk of contracting HIV?
Before donating blood donors are asked about possible risk factors that would increase the likelihood that the blood is infected with pathogens. In addition, the blood is tested for various pathogens, such as HIV or hepatitis B tested. Nevertheless, a possible infection cannot be completely ruled out. The risk of becoming infected with HIV during a blood transfusion is very low and is estimated at 1 in 16,000,000.
Jehovah's Witnesses and Blood Transfusion
Most Jehovah's Witnesses refuse blood transfusions. The reason for this is their interpretation of some verses of the Bible. A transfusion is also forbidden among Jehovah's Witnesses in emergency situations in which donor blood would be necessary. A violation of this rule often leads to expulsion from the community.

.jpg)