The splenic infarction
What is a splenic infarction?
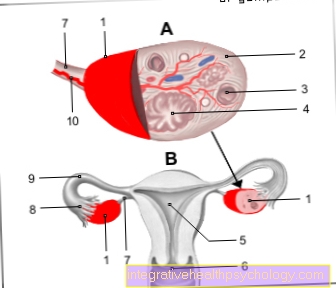
In the case of a splenic infarction, a blood clot causes (partial) closure of the main artery of the spleen, the so-called splenic artery or one of its branches. The oxygen and nutrient supply is no longer guaranteed due to the blocked vessel. Depending on where the vascular occlusion is located, there is an undersupply of certain areas of the spleen or, in the worst case, the entire spleen.
The lack of supply ultimately leads to the death of the cells located there. In this context, doctors speak of tissue necrosis.

The symptoms
A classic symptom of a splenic infarction is severe left-sided upper abdominal pain. In addition to abdominal discomfort, some people also experience pain in their left arm. This phenomenon is called pain radiation. Furthermore, nausea and vomiting can occur. Fever can also show up as part of a splenic infarction.
When the above symptoms occur, medical professionals also speak of an acute abdomen. The acute abdomen usually indicates a disease or insufficient supply of an organ in the abdominal cavity and requires immediate medical clarification.
Also read the article: Acute abdomen.
The diagnosis
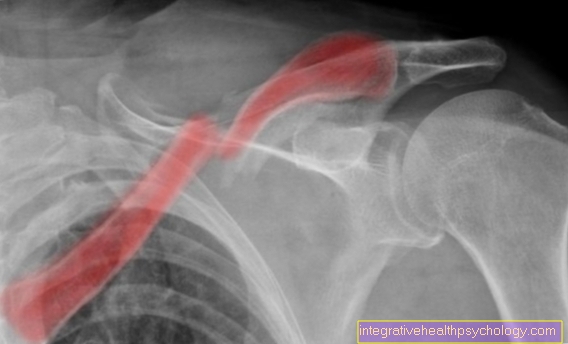
If a splenic infarction is suspected, a special ultrasound examination is usually carried out. It is a Doppler sonography. Here the vascular supply of the spleen can be examined with ultrasound waves, in addition to the graphic representation of tissue. Usually, Doppler sonography is sufficient to diagnose a splenic infarction.
In a few cases, computed tomography (CT) is also performed.
Find out more about the topic here: Ultrasound of the abdomen.
The treatment
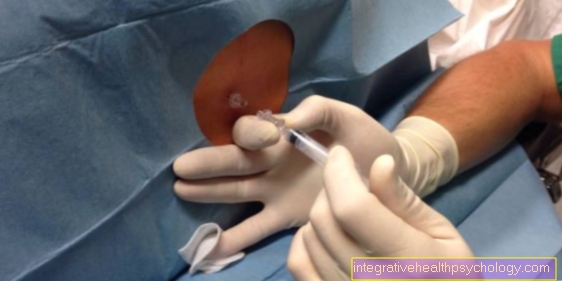
Treatment depends on the size of the infarct. With small vessels, often only supportive measures are taken. Those affected are usually treated with pain medication and initially placed under observation. The small area of tissue that was affected by the infarct then heals with scarring. The remaining part of the spleen can still fulfill its function.
In the case of a larger, acute infarct, anticoagulants can be administered. These are drugs that prevent further “clot formation” (thrombus). If the vascular occlusion has already led to the death of a large part of the tissue in the spleen, the spleen must be completely removed. This process is known as a splenectomy.
In addition to treating the splenic infarction, the cause or trigger of the infarction should always be identified and treated.
For more information, read on here: The removal of the spleen.
The blood thinning
Blood-thinning drugs, such as heparin, are used to treat acute blood clots (thrombus). They influence the coagulation processes and thus reduce the risk of further thrombus formation. Depending on the cause of a splenic infarction, they can also be taken prophylactically, i.e. to prevent a further infarction.
Find out all about the topic here: Anticoagulants.
Prognosis
A splenic infarction is caused by a disturbance of the blood flow in the tissue and usually occurs within a few minutes. The location of the infarct and the associated cell death make a decisive contribution to the prognosis.
In the case of small infarct areas, the spleen can usually continue to do its job. However, one should find out the cause of the infarction and treat it appropriately in order to avoid future infarcts.
Surgical removal of the spleen may be necessary in large areas of the infarct. However, people who have had their spleen removed have a much higher risk of infection. Bacterial diseases in particular are favored by the lack of defense cells in the spleen. Due to the risk of infection and the associated complications, such as blood poisoning, those affected usually have a poorer prognosis with regard to their lifespan.
What is the function and task of the spleen? Find out more here.
The course of the disease
Depending on the location, a splenic infarction leads to cell death. In the case of small infarcts, localized tissue destruction can occur without significantly affecting the function of the spleen. Those affected are often still able to continue living without restrictions.
In large infarcts with removal of the spleen, the course of the disease is more complicated. The lack of a spleen can lead to serious infections in those affected, some of which can be life-threatening. Many of those affected are then dependent on special medication for prophylaxis (preventive measures) against infections.
What are the long-term consequences of a splenic infarction?
The long-term consequences of a splenic infarction depend on the size of the destroyed spleen tissue. A “small” splenic infarction, in which only a small amount of tissue has gone under, is usually not associated with any significant loss of function of the spleen. Those affected then usually do not have to fear any health restrictions or risks.
In the case of a heart attack that has led to a large tissue defect, the spleen can no longer function. It is then often removed in a surgical procedure. The lack of a spleen then increases the risk of infection, especially for bacterial diseases. The reason for the increased risk of disease is the failure of special immune defense cells, which are normally located in large numbers in the spleen and play a crucial role in the defense against pathogens.
Can a splenic infarction be fatal?
A splenic infarction can be life threatening in certain circumstances. It is often not the heart attack that is responsible for the death of those affected, but rather the previous illnesses that favored the heart attack. For example with a tumor or cancer of the blood cells.
Removing the spleen after a major infarction can also greatly increase the risk of death. In the case of infections, people without a spleen are not adequately protected and run the risk of developing serious infections. Without the protective effect of the immune cells from the spleen, these can sometimes be fatal.